
Recognition and Treatment of Obstructive Sleep Apnea in Older Adults: A Case Report
*Corresponding Author(s):
Marjorie AlmedaMichigan Medicine Geriatric Primary Care, Michigan, 4260 Plymouth Road, Ann Arbor, MI 48109, United States
Tel:+1 7347646831,
Email:shelbs@med.umich.edu
Abstract
Obstructive Sleep Apnea (OSA) often goes undiagnosed in older adults. The sleep disturbances experienced by older adults are often believed to be part of the normal aging process, and this population may present with atypical symptoms. Thus, sleep disorders in older adults are often underdiagnosed and undertreated and are associated with significant functional impairment. We present a case of a non-obese, active 92-yo woman who presented with fatigue, difficulty sleeping, nocturia and nighttime toe cramping. Her medical history was remarkable for TIA and essential tremor. An overnight sleep study showed: 75 apneic episodes; AHI score of ~23 (moderate severity); and min %SpO2 of 85. She was diagnosed with OSA and prescribed a CPAP mask. At her 2-month follow up visit, she reported improved energy and reduced overall fatigue and her nocturia had resolved. Five months later, the patient reported improved sleeping and energy, and her nighttime toe cramping had improved. OSA should be recognized and treated in older adults who may present with atypical symptoms.
Keywords
Aged; Aged 80 and over; Continuous positive airway pressure; Obstructive; Polysomnography; Sleep apnea
INTRODUCTION
Age-related changes in sleep patterns are common and are often considered a normal part of the aging process. These normal alterations in sleep patterns include changes in the circadian rhythm that lead to a difference in sleep timing and a change in sleep architecture that results in lighter, less restful sleep [1,2]. However, these normal changes in sleep patterns can mask the presence of sleep disorders, such as insomnia, Restless Leg Syndrome (RLS), and Sleep-Disordered Breathing (SDB), which includes Obstructive Sleep Apnea (OSA) [1,2]. OSA is characterized as recurrent episodes of obstruction of the upper airway during sleep [3,4]. Common symptoms include snoring, nocturnal choking, episodes of apnea and daytime sleepiness [3,4]. Risk factors for OSA include obesity, male sex, thick neck circumference (men, >17”; women, >16”), increasing age, the use of alcohol, sedatives, or tranquilizers, and smoking [4,5]. OSA is typically diagnosed through polysomnography (PSG; i.e., a sleep study). PSA is used to determine the number of respiratory events (the cessation of airflow) per hour, which is quantified as the Apnea-Hypnotic Index (AHI) [6]. An AHI value >5 is indicative of OSA, and the severity of OSA is defined as follows according to the guidelines of the American Academy of Sleep Medicine [7]: AHI 5-14, mild; AHI 15-29, moderate; and AHI >30, severe [8]. OSA is present in ~20%-56% of women and ~28%-70% of men ages 65-99 [7].
Sleep disorders have been associated with obesity, type 2 diabetes, hypertension, hyperlipidemia, metabolic syndrome and cardiovascular disease [3,7]. In older adults, sleep disorders have been associated with a decrease in cognitive function [9,10] and other quality of life-related symptoms [1,2]. Thus, sleep disorders can have a profound impact on the health and daily functioning of older adults. However, sleep disorders such as SDB and OSA are often overlooked in the elderly. It is important to recognize that the symptoms may present differently in the geriatric population and to screen for sleep disorders in the presence of indicators of poor sleep.
Here, we report an elderly female without typical risk factors for OSA and with an atypical presentation. A diagnosis of OSA led to treatment with Continuous Positive Airway Pressure (CPAP) therapy, which resulted in improved sleep and energy levels and a resolution of her nocturia. The findings of this case report underscore the clinical need to evaluate older adults for sleep disorders, such as OSA, when suspected due to poor sleep or energy levels in the absence of traditional symptoms or risk factors, particularly as a proper diagnosis and treatment can improve cognition, function, and quality of life.
CASE REPORT
Patient
A 92-year-old female presented at the Geriatrics Clinic of our institution for insomnia and nocturnal spasms in her toes. She had been seen in the clinic several times over the prior two years with complaints of fatigue, chronic insomnia, nocturia (4-5 times per night), foot and toe cramping, and incontinence. She reported frequent daytime napping. She was a former smoker (>30 years since quitting) who consumed approximately 6 oz of wine daily and did not use sedatives. She had a normal body-mass index and was physically active with daily exercise. She could perform all activities of daily living and most instrumental activities of daily living independently. Her medical history was remarkable for transient ischemic attack and essential tremor. Past visits had discussed sleep hygiene and the use of stretches and a heating pad for the foot and toe cramping; the patient followed the suggested activities with no improvement in symptoms. Complete blood count analysis indicated that all values were within normal ranges with no indication of anemia. She was then referred for a PSG.
Sleep study
The PSG was performed in a standard fashion. Data acquisition and the scoring of sleep and all associated events were performed in accordance with the recommended standards and specifications as outlined in the AASM Manual for the Scoring of Sleep and Associated Events 2.4.0 (2017) [11].
The study had a total recording time of ~440 min; the patient recorded a total sleep time of <200 min, with almost 70 total arousals (~20 arousals/hour of sleep). The respiratory analysis indicated an AHI of ~23 (moderate severity); her Mean sleep %SpO2 was <95, and Min %SpO2 was 85. In total, the patient experienced almost 80 apneic episodes, the majority of which were hypopneas. sThe apneic episodes occurred while the patient slept on her left or right side, with no apneic episodes recorded while in the prone or supine position. Leg movement analysis indicated a total number of Periodic Limb Movements (PLMs) during sleep over >120, with a PLM Index (PLMs per hour of sleep) of ~35 (moderate) and a PLM Arousal Index of 1.2.
Diagnosis, treatment and follow-up
The patient was diagnosed with OSA and periodic leg movements of sleep. She returned to the sleep center approximately two weeks later for CPAP titration.
A follow-up visit approximately two months after the patient was fitted with the CPAP found that she was compliant with CPAP use. The patient reported that she felt more rested and much less tired. She still reported issues with RLS and toe cramping. Her nocturia had resolved, although she still experienced incontinence. At a subsequent visit 5 months later, the patient confirmed her continued compliance with CPAP use: she wore the CPAP all night, every night. She reported sleeping better and felt that the CPAP had been beneficial. Her energy level was good, and she no longer took daytime naps. She still reported some RLS although her nighttime toe cramping had improved. She continued to have issues regarding urinary incontinence but no longer reported experiencing nocturia.
DISCUSSION
Normal variations in sleep patterns occur with age, such as changes in the circadian rhythm that can lead to changes in the timing of sleep [2,12]. In addition, older adults exhibit differences in sleep architecture, with a decrease in deep, restful sleep and an increase in light sleep [2,12]. However, sleep disorders are also very common in older adults. A study by Endeshaw evaluated 94 community-dwelling adults aged 62-91 and found that over 30% of this population had moderate-to-severe OSA (AHI≥15) [13]; notably, traditional risk factors (snoring, body mass index and neck circumference) were not associated with OSA in this study population. In contrast, moderate-to-severe OSA was associated with symptoms such as not feeling rested in the morning, a higher score on the Epworth Sleepiness Scale and nocturia [13].
Importantly, sleep disorders can have serious consequences in the older population due to their adverse effects on cognitive function [9,10]. SDB has been shown to affect attention, response time, memory, concentration and the incidence of falls in older adults [1,2]. Similarly, some studies have shown improved cognitive abilities with improved sleep; for example, a study by Ancoli-Israel et al., showed that three weeks of compliant CPAP use resulted in a significant improvement in cognition in patients with Alzheimer’s disease [14]. Furthermore, treatment for sleeping disorders has been shown to improve quality of life in older adults [15,16]. A study of patients ≥70 years of age with severe OSA found that compliant CPAP use resulted in a significant improvement in all sleep-related quality of life domains (e.g., daytime and nighttime symptoms and social and emotional aspects), sleep-related symptoms (e.g., snoring, apneas, choking, nocturia, etc.), anxiety, depression and some neurocognitive aspects (related to working memory and executive function) [15].
Here, we describe a case of OSA in an elderly female with an atypical profile for OSA. She was a non-smoking female with a normal BMI who drank a moderate amount of alcohol (one glass of wine/day). Her primary complaints were symptoms of RLS (foot and toe cramping), nocturia and fatigue. A PSG confirmed her RLS and indicated the presence of OSA with AHI of ~23 (moderate severity). Treatment with a CPAP improved her sleep quality and her energy levels and her nocturia resolved. The patient reported feeling refreshed and felt that the CPAP has been beneficial.
At the time of this report, the patient is leading an active and full life in her 90s. She exercises daily and is socially engaged. Her sleeping and energy levels were improved by treating her OSA with a CPAP. This case report highlights the importance of a focused evaluation of sleep in the elderly, and a formal sleep study should be conducted when sleep disturbances are suspected even in the absence of typical risk factors for this disorder.
CONCLUSION
Sleep disorders, such as OSA, should be suspected and investigated in older adults who may present with ambiguous symptoms, such as fatigue or nocturia and no obvious risk factors. Many older adults believe that poor sleep is a natural part of the aging process. However, treating sleep disorders can improve the health and quality of life in the older population.
FUNDING
This research received no external funding.
ACKNOWLEDGEMENT
We would like to thank Christine Billecke, PhD, from Billecke Medical Writing LLC, for her assistance in the preparation of this manuscript.
CONFLICTS OF INTEREST
The author declares no conflict of interest.
REFERENCES
- Mazza M, Della Marca G, De Risio S, Mennuni GF, Mazza S (2004) Sleep disorders in the elderly. Clin Ter 155: 391-394.
- Neikrug AB, Ancoli-Israel S (2010) Sleep disorders in the older adult - a mini-review. Gerontology 56: 181-189.
- West SD, McBeath HA, Stradling JR (2009) Obstructive sleep apnoea in adults. BMJ 338: 1165.
- Russell T, Duntley S (2011) Sleep disordered breathing in the elderly. Am J Med 124: 1123-1126.
- Mayo Clinic (2019) Sleep apnea. Mayo Clinic, Rochester, USA.
- Greenstone M, Hack M (2014) Obstructive sleep apnoea. BMJ 348: 3745.
- Lin J, Suurna M (2018) Sleep Apnea and Sleep-Disordered Breathing. Otolaryngol Clin North Am 51: 827-833.
- Ruehland WR, Rochford PD, O'Donoghue FJ, Pierce RJ, Singh P, et al. (2009) The new AASM criteria for scoring hypopneas: Impact on the apnea hypopnea index. Sleep 32: 150-157.
- Dzierzewski JM, Dautovich N, Ravyts S (2018) Sleep and Cognition in Older Adults. Sleep Med Clin 13: 93-106.
- Zimmerman ME, Aloia MS (2012) Sleep-disordered breathing and cognition in older adults. Curr Neurol Neurosci Rep 12: 537-546.
- AASM (2017) The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. American Academy of Sleep Medicine, Darien, Illinois, USA.
- Rodriguez JC, Dzierzewski JM, Alessi CA (2015) Sleep problems in the elderly. Med Clin North Am 99: 431-439.
- Endeshaw Y (2006) Clinical characteristics of obstructive sleep apnea in community-dwelling older adults. J Am Geriatr Soc 54: 1740-1744.
- Ancoli-Israel S, Palmer BW, Cooke JR, Corey-Bloom J, Fiorentino L, et al. (2008) Cognitive effects of treating obstructive sleep apnea in Alzheimer's disease: A randomized controlled study. J Am Geriatr Soc 56: 2076-2081.
- Martínez-García MÁ, Chiner E, Hernández L, Cortes JP, Catalán P, et al. (2015) Obstructive sleep apnoea in the elderly: Role of continuous positive airway pressure treatment. Eur Respir J 46: 142-151.
- Suzuki K, Miyamoto M, Hirata K (2017) Sleep disorders in the elderly: Diagnosis and management. J Gen Fam Med 18: 61-71.
SLEEP ANALYSIS DATA
Weight: 139.5 lbs Height: 5’0.5” BMI: 26.8 kg/m2 Neck size: 12.6”
Test Description: PSG
Monitored: Frontal, central & occipital EEG, EOG, submentalis EMG, oronasal thermocouple, nasal pressure, ECG, thoracic and abdominal inductance plethysmography, right and left anterior tibialis EMG, snore sensor and pulse oximetry.
Procedure Note: This study was performed in standard fashion. The data acquired and the scoring of sleep and all associated events were performed in accordance with the recommended standards and specifications as outlined in the AASM Manual for the Scoring of Sleep and Associated Events 2.4.0 (2017). An epoch by epoch review is performed of the entire study by at least one of the sleep board-certified or board-eligible clinicians whose signature line appears below. The “AHI*” in this report uses the current hypopnea definition according to Medicare Criteria. The “AHI” is consistent with the current hypopnea definition according to AASM crit
Sleep analysis
|
Lights Out/On (clock times) |
22:56:45/06:14:46 |
|
Min |
% of TST |
|
Total Recording Time (TRT, min/hr) |
438.0/7:18.0 |
Wake after sleep onset |
236.5 |
|
|
Total Sleep Time (TST, min) |
199.5 |
Stage N1 Sleep |
17.5 |
8.8 |
|
Latency to sleep (min) |
2.0 |
Stage N2 Sleep |
91.0 |
45.6 |
|
REM Latency (min) |
162.5 |
Stage N3 Sleep |
30.0 |
15.0 |
|
Stage Shifts (#) |
74 |
Stage R Sleep |
61.0 |
30.6 |
|
Arousals (#) |
69 |
Sleep Efficiency |
|
45.5 |
|
Arousals/hour of sleep |
20.8 |
Stage R EMG Variance Score |
|
4.02 |
Respiratory analysis
|
Apnea/Hypopnea Index (AHI) |
23.2 |
Respiratory Disturbance Index (RDI) |
23.2 |
|
NREM AHI |
26.0 |
Obstructive Apnea Index |
0.3 |
|
REM AHI |
16.7 |
Central Apnea Index |
4.5 |
|
AHI* (hypopnea w/4% desat) |
9.3 |
Hypopnea Index (AASM Criteria)S |
18.3 |
|
Mean Sleep % SpO2 |
94 |
RERA Index |
0.0 |
|
Min %SpO2 |
85 |
|
|
|
% of Sleep Time with SpO2 ≤88% |
0.3 |
|
|
|
Number of events |
NREM |
REM |
|
|
|
Apneic Episodes (#) |
60 |
17 |
Additional apneic events during wake epochs: |
14 |
|
Obstructive apneas |
1 |
0 |
Cheyne Stokes breathing: |
No |
|
Mixed apneas |
0 |
0 |
% of Sleep Time with Cheyne Stokes breathing |
0.0 |
|
Central apneas |
15 |
0 |
Snoring: Frequent Loud |
|
|
Hypopneas |
44 |
17 |
|
|
|
RERAs |
0 |
0 |
|
|
|
Position |
Prone |
Supine |
Left |
Right |
||||
|
|
NR |
R |
NR |
R |
NR |
R |
NR |
R |
|
# of apneas & hypopneas |
0 |
0 |
0 |
0 |
34 |
6 |
26 |
11 |
|
TST/pos. (min) |
0.0 |
0.0 |
1.0 |
0.0 |
53.0 |
21.0 |
84.5 |
40.0 |
|
AHI |
0.0 |
0.0 |
0.0 |
0.0 |
38.5 |
17.1 |
18.5 |
16.5 |
ECG analysis
|
NREM HR (range) |
42 - 67 |
Sleep HR (max) |
67 |
|
REM HR (range) |
41 - 67 |
HR (TRT, max) |
67 |
|
Arrhythmias: |
Yes/No |
Comment |
|
Yes/No |
Comment |
|
Bradycardia |
N |
|
Wide complex tachycardia |
N |
|
|
Asystole |
N |
|
Atrial fibrillation |
N |
|
|
Sinus tachycardia |
N |
|
Other: N.A. |
|
|
|
Narrow complex tachycardia |
N |
|
|
|
|
Leg movement analysis
|
Periodic limb movements (PLMs) during sleep (#) |
125 |
PLM Index (PLMs per hour of sleep) |
37.6 |
|
Periodic limb movements during sleep with arousal (#) |
4 |
PLM Arousal Index |
1.2 |
Interpretation: This baseline polysomnogram showed obstructive sleep apnea mostly in the form of hypopneas with clear obstructive features. Central apneas were also noted at a higher than anticipated frequency. Sleep efficiency was reduced due to increased wake time after sleep onset during which patient had excessive leg movements and appeared restless. If patients had typical restless legs syndrome complaint, treatment may benefit her. Periodic leg movements in sleep were noted.
Please note that patient may not be ideal candidate for auto-titrating CPAP given the central apneas noted in the study.
Diagnosis: Obstructive sleep apnea, Periodic leg movements of sleep.
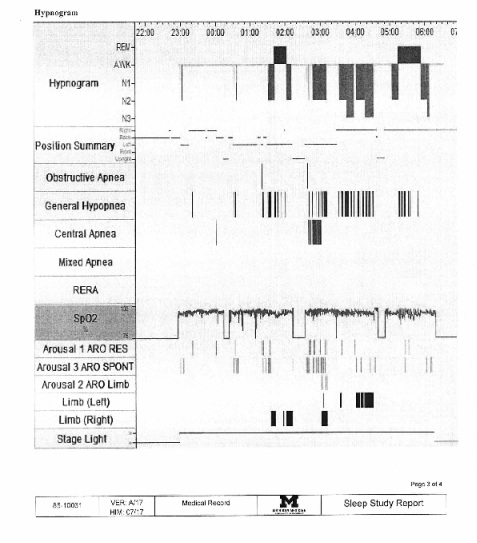 PSG tracing 1
PSG tracing 1
 PSG tracing 2
PSG tracing 2
Citation: Almeda M (2020) Recognition and Treatment of Obstructive Sleep Apnea in Older Adults: A Case Report. J Gerontol Geriatr Med 6: 049.
Copyright: © 2020 Marjorie Almeda, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

