
Reconstruction of Complex Chest Wall Defect with Perforator Based Abdominal Flap - A Case Report
*Corresponding Author(s):
Shailendra SinghConsultant Plastic Surgeon, Sterling Hospital, Ahmedabad, Gujarat, India
Tel:9825156277,
Email:shailendrabsingh21@gmail.com
Abstract
Reconstruction of chest wall defect is a complex procedure requiring acute understanding of the vascularity of local flaps used for reconstruction of the defect. This article describes the use of transverse abdominal flap based on superior epigastric artery perforator providing adequate healthy soft tissue cover to the large chest wall defect resulting from debridement of the underlying osteomyelitic ribs, from radio necrosis secondary to radiotherapy for breast cancer.
Keywords
Abdominal flap; Chest wall defect; Osteoradionecrosis
Introduction
Osteoradionecrosis of the chest wall is a complication seen after whole breast radiotherapy. Here we report a similar case involving underlying ribs following adjuvant whole breast radiotherapy and resulting chest wall defect after wide debridement and ligation of ipsilateral internal mammary artery. The defect was covered with abdominal flap based on perforators of the contralateral superior epigastric artery perforators and perforators from the watershed area between xiphoid to umbilicus.
Case Report
A 70 year old female presented with discharging sinuses and pigmented dried skin measuring 10 * 11 cm on the right chest wall lateral to midline with erythema resulting from osteoradionecrosis of the underlying 2-5 ribs and involvement up to pleura in an operated case of modified radical mastectomy followed by whole breast radiotherapy for ductal adenocarcinoma right breast. Swab culture showed Staphylococcus aureus and antibiotic was given according to sensitivity. Patient underwent routine blood workup and computed tomography of thorax to gauge the involvement of the underlying organs and was planned for excision and cover. The sinus, surrounding skin , intercostal muscle and 2-5 ribs with underlying adherent pleura was removed and ipsilateral internal mammary was ligated and secured proximally, creating a defect of 15 * 15 cm. Inter costal drainage tube was kept in the right chest, the defect covered with Polypropylene mesh. Defect was measured and flap based on 4 perforators of superior epigastric and deep inferior epigastric artery system of contralateral side was marked. A flap of 23 * 18 cm from the ipsilateral side of the abdomen was raised and rotated to cover the chest defect. Chest defect closed with negative drain over the mesh. Flap donor defect covered with split thickness graft harvested from the ipsilateral thigh. Flap was monitored regularly for vascularity. Drain was removed on postoperative day 10 and Patient was discharged uneventfully. Patient has followed up with healthy flap in postoperative period (Figures 1 and 2).
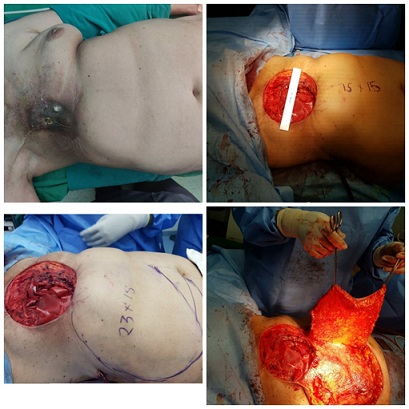 Figure 1: Pre-operative and intra operative pictures of delineating defect and raising abdominal wall flap.
Figure 1: Pre-operative and intra operative pictures of delineating defect and raising abdominal wall flap.
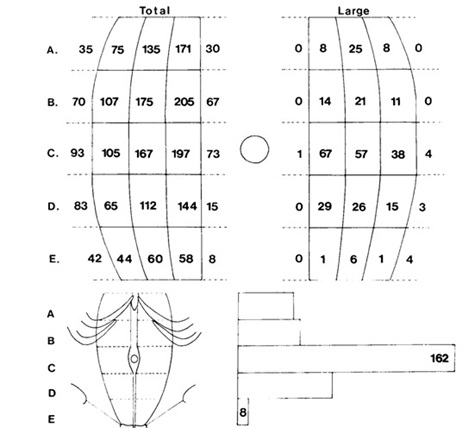 Figure 2: Diagram showing anterior abdominal wall perforators.
Figure 2: Diagram showing anterior abdominal wall perforators.
Surgical anatomy
The deep inferior epigastric artery divides into two to three large branches, below the level of the umbilicus. These vessels pass upward in the muscle to communicate with the superior epigastric system above the level of umbilicus. The superior epigastric artery originates at the bifurcation of the internal mammary artery opposite the 10th costal cartilage. Passing behind the seventh costal cartilage, it pierces the posterior rectus sheath to lie on the posterior surface of the muscle, it divides into three branches: medial and lateral muscular branch, and lateral segmental branch that skirts the costal margin in the neurovascular plane. Both muscular branches supply muscle, and give rise to musculocutancous perforators and anastomose with the deep inferior epigastric artery inferiorly [1-4].
The anastomosis has the following arrangements of the perforators
The cutaneous branches are arranged in three vertical groups; a medial group of fasciocutancous perforators emerging through the linea alba, a middle group of musculocutanecous perforators piercing the anterior rectus sheath, and a lateral group of fasciocutaneous perforators passing through the external oblique aponeurosis [5].
This is the picture taken from a study conducted by Boyd et al [5], which divides the rectus abdominis into horizontal 5 parts and vertical 3 parts giving a total of 15 zones per muscle. The total number of perforators is given on the left and the large ones on the right. The number of perforators decrease in number as we go laterally.
The points to be noted
- There are few perforators on lower 1/5th of the anterior rectus sheath (zone E), and are of small calibre.
- Although zone B has the most perforators, the paraumbilical zone C has the greatest concentration of major perforators.
- There is a tendency for the concentration of perforators to be less over the lateral third of the muscle in all zones.
- Few major perforators: emerge through either the external oblique aponeurosis or the lines alba.
- The greatest density of larger perforators is located over the middle and medial thirds of the muscle in the paraumbilical region.
Discussion
Breast carcinoma is the most common indication for the chest wall irradiation, leading to post radiation changes in, tissues of the chest and mediastinum. Patients with osteoradionecrosis can present with diverse symptomatology, ranging from occult disease to deep ulcers and major bone destruction with soft tissue necrosis, months to years after radiotherapy [3]. Full-thickness chest wall resection with reconstruction is one of the most challenging surgeries. The loss of effective chest wall rigidity can result in paradoxical respiration, ineffective respiratory effort and respiratory embarrassment.
The presence of necrotic bone and soft tissue with discharging sinus in our case required radical debridement and to avoid bleeding during debridement of necrotic tissue the internal mammary of the ipsilateral side was secured proximally, the debridement lead to exposure of the pericardium and right lung.
The defect created was 15*15cm and required a large tissue cover which led us to raise a transversely oriented Fasciocutaneous flap based on 4 contralateral supraumbilical perforators of the Superior Epigastric Artery (SEA) and Deep Inferior Epigastric Artery (DIEA) supplying the ventromedial skin of the lower thorax and supra and periumbilical abdominal wall measuring 23*18 cm to cover the chest defect [4]. 4-5 perforators per hemi abdomen can be expected on an average in the area between the xyphoid process and umbilicus [4].
A mediolateral orientation of subcostal SEAP angiosomes has better outcome than craniocaudal direction. The SEA connects to the DIEA in a watershed area midway between the xyphoid process and the umbilicus. A transversely oriented SEAP flap based on infraxyphoidal/ subcostally emerging perforators can be raised laterally as far as anterior axillary line and rotated cranially for breast, sternal or chest wall reconstruction. A vertically oriented superior epigastric artery flap design reaching up to the supraumbilical skin will include neighbouring DIEP angiosomes supplied by at least 2 choke anastomoses [4].
The length to breadth ratio of the mentioned flap was 1: 1.2 which is well within the maximum safe limit of 1: 2.5 which can be raised as stated by Tai and Hasegawa. They has also stated the lateral limit to be posterior axillary line and the flap we have discussed reached up till anterior axillary line [6] (Figure 3).
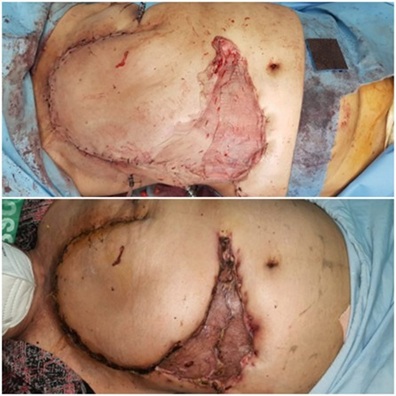 Figure 3: Abdominal flap covering the chest defect created; immediate post operative and after 1 month follow up.
Figure 3: Abdominal flap covering the chest defect created; immediate post operative and after 1 month follow up.
Conclusion
The transverse abdominal flap preserves the perforating vessels from superior epigastric artery and vein on the abdominal muscles and serves as an ideal skin donor site away from the field of the primary cancer which will provide a healthy cover where the tissue is not irradiated.
Declaration of Consent
The authors certify that they have obtained all appropriate patient consent forms in patients language. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflict of Interest
There are no conflicts of interest.
Financial Support
Nil.
References
- Sharma GN, Dave R, Sanadya J, Sharma P, Sharma KK (2010) Various types and management of breast cancer: an overview. J Adv Pharm Technol Res 1: 109-126.
- Nicholls L, Gorayski P, Harvey J (2015) Osteoradionecrosis of the Ribs following Breast Radiotherapy. Case Rep Oncol 8: 332-338.
- Pruksapong C, Burusapat C, Satayasoontorn K (2020) Osteoradionecrosis of the chest wall. Plast Reconstr Surg Glob Open 8: 2665.
- Schmidt M, Tinhofer I, Duscher D, Huemer GM (2014) Perforasomes of the upper abdomen: An anatomical study. J Plast Reconstr Aesthet Surg 67: 42-47.
- Boyd JB, Taylor GI, Corlett R (1984) The vascular territories of the superior epigastric and the deep inferior epigastric systems. Plast Reconstr Surg 73: 1-16.
- Tai Y, Hasegawa H (1974) A transverse abdominal flap for reconstruction after radical operations for recurrent breast cancer. Plast Reconstr Surg 53: 52-54.
Citation: Singh S, Narola S, Patel K, Zapadiya R, Bhatia V (2021) Reconstruction of Complex Chest Wall Defect with Perforator Based Abdominal Flap - A Case Report. Archiv Surg S Educ 3: 022.
Copyright: © 2021 Shailendra Singh, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

