
Relation between Maternal Vitamin D Concentration during Third Trimester and Maternal and Neonatal Health Outcomes: A Cross-Sectional Study in China
*Corresponding Author(s):
Jun ZhangDepartment Of Obstetrics And Gynecology, Beijing Anzhen Hospital, Capital Medical University, Chaoyang, Beijing, China
Tel:+86 13581566336,
Email:drzhangj@outlook.com
Abstract
Background: Vitamin D is a key nutritional factor for maintenance of maternal and fetal health. Fetal vitamin D acquisition is entirely dependent on the availability of the mother’s 25-hydroxyvitamin D, Vitamin D regulates parathyroid hormone level and increases calcium absorption, critical factors in fetal development.
Objective: Vitamin D deficiency occurs frequently in pregnancy and may lead to preeclampsia, gestational diabetes, postpartum depression, and stillbirth. Therefore, it is necessary to establish the risk factors for vitamin D deficiency during pregnancy to enable a preliminary and predictable diagnosis of vitamin D deficiency and its complications.
Materials and Methods: This cross-sectional study was conducted between February 2017 and January 2019 in a referral tertiary hospital in Beijing, China. All data were extracted from the hospital’s patient information system. Vitamin D deficiency was defined as total serum 25-hydroxyvitamin-D concentration less than 20 ng/ml, whereas concentrations between 20 and 30 ng/ml were classified as vitamin D insufficiency.
Results: We included 306 participants with singleton pregnancies. The prevalence of vitamin D deficiency was 57.51% (176/306). A significant correlation was found between vitamin D concentration and the gestational week of delivery (P ≤0.001).
Conclusion: Vitamin D deficiency is a common phenomenon among pregnant women in the Chinese mainland, and the concentration of vitamin D in their bodies is significantly correlated with the progress of pregnancy.
Keywords
Infant Health; Maternal Health; Pregnancy Trimester; Vitamin D
Abbreviations
25 hydroxyvitamin D (25(OH)-D)
Gestational diabetes mellitus (GDM)
Small for gestational age (SGA)
Preterm Birth (PTB)
Caesarean section (CS)
Introduction
Two forms of vitamin D can be readily measured, i.e., 25-hydroxyvitamin-D [25(OH)-D] and 1, 25-dihydroxyvitamin-D [1,25(OH)2D] (also known as calcitriol). The serum concentration of 25(OH) D is used to evaluate the nutritional state of persons regarding their vitamin D levels. Conversely, 1, 25(OH) 2D is the active form of vitamin D; its short half-life limits its measurement in serum [1].
Vitamin D can convert from 25-hydroxyvitamin D to 1, 25-dihydroxyvitamin D in response to the status of vitamin D in placenta, and this conversion is important for immunoregulation [2]. Deficiency of vitamin D during pregnancy correlates with gestational diabetes mellitus (GDM), preeclampsia, preterm birth, small babies, and other maternal or fetal outcomes [3]. However, it is not clear whether vitamin D deficiency is only a biomarker or whether the deficiency contributes directly to those pathologies and what may be the causative mechanism(s) [4].
A principal cause of perinatal morbidity and mortality is premature birth, which affects maternal health and the emotional and economic wellbeing of the family. Inflammation and/or infection in the placenta is associated with preterm birth [5]. Vitamin D is an important factor that is involved in the suppression or inhibition of such inflammation and infection [6]. For instance, from a meta-analysis, Qin et al. suggested that vitamin D deficiency during pregnancy was linked to an increased risk of preterm birth [7]. However, the results are of this study were inconclusive and controversial because of shortcomings such as limited diversity of the study participants. Thus, the exact effect of vitamin D deficiency in preterm birth is unresolved.
Hypertensive disorders during pregnancy are another leading cause for maternal and perinatal mortality. For example, preeclampsia accounts for 2-8% of pregnancy related complications worldwide. In Latin America and the Caribbean, 26% of maternal deaths are due to the hypertensive disorders, and hypertensive disorders account for 9% of maternal deaths in Africa and Asia [8]. Woo et al., used meta-analyses to examine the association between maternal vitamin D deficiency and preeclampsia; the results were mixed [9]. Overall, the evidence suggested that vitamin D supplementation reduced the risk of developing pre-eclampsia compared with placebos or no vitamin D supplementation [10].
Gestational diabetes mellitus is the manifestation of carbohydrate intolerance during pregnancy. The incidence of GDM is not rare [11]. The Center of Disease Control (CDC) estimates that the incidence of GDM in the United States (US) is about 10% [12]. Several studies show that Asians have the highest GDM rates [13]. By analyzing the 34-year prevalence trend of gestational diabetes in China, the results show that GDM prevalence based on the International Association of Diabetes and Pregnancy Study Groups (IADPSG) criteria was 2 to 3 times higher (15.6%, [95% CI 14.9-16.2%]) in pregnant women post-2010, compared to other criteria (e.g., World Health Organization: 7.1%, [95%CI 4.1-10.0%]) [14]. In a recent systematic review found that low blood vitamin D concentration increased the risk of GDM, and vitamin D supplementation during pregnancy could prevent GDM [15]. However, the World Health Organization still views as low quality the evidence of a positive effect of vitamin D plus calcium on GDM [10]. Therefore, the aim of the present study was to investigate association between serum vitamin D concentration and adverse pregnancy outcomes in Mainland China.
Material And Methods
Patients
This cross-sectional study was conducted between February 2017 and January 2019 at the Anzhen Hospital, a comprehensive tertiary hospital in Beijing, China. The inclusion criteria were the following: (1) women aged 18-50 years at the expected date of delivery; (2) singleton pregnancy; (3) regular prenatal care and delivery planned in Anzhen Hospital; (4) signed informed consent. We excluded women with pre-pregnant diabetes, multiple pregnancies, chronic hypertension, calcium or vitamin D metabolism disorders, active thyroid disease, eating disorders (anorexia, bulimia), emotional disorders (depression, bipolar disorder, anxiety), or drug addiction (Figure 1). All data were extracted from the hospital’s patient information system. The Research and Ethics Committee of Anzhen Hospital approved the study (Anzhen 18029X). The investigators ensured strict confidentiality of participant information by delinking patient identifiers and by using study codes. Preterm birth was defined as delivery before 37 weeks of pregnancy.
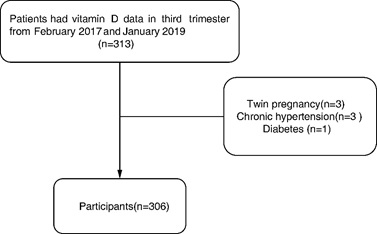 Figure 1: Recruitment of records for study participants.
Figure 1: Recruitment of records for study participants.
Recruitment of records for study participants, Preterm birth was defined as delivery before 37 weeks of pregnancy.
Vitamin D measurement
A venous blood sample (5 mL) was collected during prenatal examination after 36 weeks or immediately after delivery. The concentration of 25(OH)-D was measured by ChemiLuminescence (DiaSorin Inc., Saluggia, Italy). Total serum 25(OH)-D concentration between 20 and 30 ng/ml and concentration less than 20 ng/ml were considered as vitamin D insufficiency and deficiency, respectively [16].
Statistical analysis
Data analysis was performed with SPSS 23 and Empower software (X&Y Solutions, Inc. Boston, USA). Descriptive statistics were conducted for relevant data. One way analysis of variances (ANOVA) and Kruskal Wallis test were used for quantitative data. Either the independent sample t-test or Mann–Whitney U test was used to compare continuous variables. The χ2 test was used to analyze the association between categorical variables and maternal and neonatal health outcomes. Linear regression was used to analyze the association between birth week and vitamin D concentration. A value of P < 0.05 was considered to represent statistical significance.
Results
Among the 313 records that were initially examined for this study, 306 (97.7%) were included in the analysis. Table 1 lists the characteristics of the participants. Most of the expectant women (176, 57.5%) had vitamin D deficiency with about a quarter of them (79, 25.8%) displaying vitamin D insufficiency. There was a significant difference in the BMI of the women stratified according to their vitamin D concentrations. The mean BMI in vitamin D sufficiency group was 21.82kg/m2, while the mean BMI in vitamin D deficiency was 22.96 kg/m2 and insufficiency group was 22.23 kg/m2.
|
Characteristics |
All participants |
Vitamin D deficiency |
Vitamin D insufficiency |
Vitamin D sufficiency |
P value |
|
|
- |
N=306 |
N=176 (57.51%) |
N=79 (25.82%) |
N=51 (16.67%) |
- |
|
|
Age (yr) * |
31.02 ± 3.85 |
31.00 ± 3.86 |
31.22 ± 4.24 |
30.78 ± 3.13 |
0.82 |
|
|
BMI (kg/m2) * |
22.58 ± 3.56 |
22.96 ± 3.49 |
22.23 ± 3.78 |
21.82 ± 3.34 |
0.038 |
|
|
GWG (kg) * |
14.05 ± 4.91 |
13.85 ± 4.80 |
14.45 ± 5.13 |
14.08 ± 4.99 |
0.67 |
|
|
GDM** |
81 (26.47%) |
46 (26.14%) |
21 (26.58%) |
14 (27.45%) |
0.982 |
|
|
HD** |
29 (9.48%) |
14 (7.95%) |
12 (15.19%) |
3 (5.88%) |
0.119 |
|
|
PE** |
3 (0.98%) |
1 (0.57%) |
2 (2.53%) |
0 (0.00%) |
0.25 |
|
|
PB** |
13 (4.25%) |
9 (5.1%) |
3 (3.8%) |
1 (2.0%) |
0.601 |
|
|
Newborn weight (g) * |
3378.73± 450.50 |
3372.39 ± 477.40 |
3411.52 ± 414.45 |
3349.80 ± 411.90 |
0.719 |
|
|
Serum 25(OH)-D (ng/ml) * |
20.65 ± 12.23 |
12.84 ±4.25 |
23.84± 2.73 |
42.63 ± 10.70 |
- |
Table 1: Baseline characteristics of the participants.
Note: * Data are mean ± SD. ** Data presented as n (%). One way analysis of variances or Kruskal Wallis test. BMI: Body Mass Index; GWG: Gestational Weight Gain; GDM: Gestational Diabetes Mellitus; HD: Heart Disease; PE: Preeclampsia; VD: Vaginal Delivery; PB: preterm birth.
|
Characteristics |
< 37 weeks |
≥ 37 weeks |
p-value |
< 39 weeks |
≥ 39 weeks |
P-value |
|
|
N=3 |
N=149 |
|
N=38 |
N=114 |
|
|
Age*a |
27.67 ± 5.51 |
30.38 ± 3.76 |
0.222 |
30.84 ± 4.20 |
30.15 ± 3.65 |
0.331 |
|
BMI* a |
27.50 ± 5.55 |
22.18 ± 3.57 |
0.012 |
23.17 ± 4.06 |
21.99 ± 3.50 |
0.062 |
|
GWG* a |
11.67 ± 2.89 |
13.90 ± 4.38 |
0.259 |
12.72 ± 3.79 |
14.24 ± 4.49 |
0.024 |
|
GDM**b |
1 (33.33%) |
29 (19.46%) |
0.485 |
8 (21.05%) |
22 (19.30%) |
0.814 |
|
PE** b |
1(33.33%) |
0 (0.00%) |
< 0.001 |
1 (2.63%) |
0 (0.00%) |
0.082 |
|
Serum 25(OH)-D*a |
15.17 ± 7.18 |
21.55 ± 13.17 |
0.4 |
17.23 ± 6.65 |
22.83 ± 14.38 |
0.022 |
Table 2: Baseline characteristics of participants with vaginal delivery.
Note: * Data are mean ± SD. ** Data present as n (%). a: T-test; b: χ2 test. BMI: Body Mass Index; GWG: Gestational Weight Gain; GDM: Gestational Diabetes Mellitus; PE: Preeclampsia
Significant linear correlations were noticeable between the maternal vitamin D status and either the gestational period (Figure 2) or the BMI. However, there was no correlation between the maternal vitamin D status and either the gestational weight gain, method of delivery, newborn weight, or GDM (Table 1).
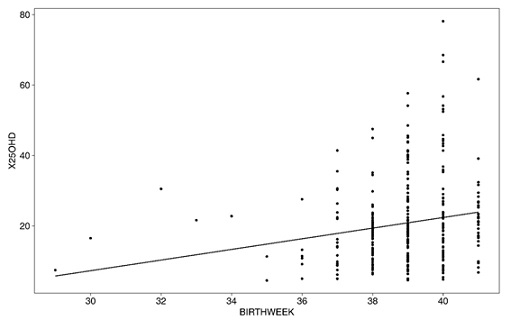 Figure 2: Linear relationship between serum 25(OH)-D and birth week.
Figure 2: Linear relationship between serum 25(OH)-D and birth week.
Significant linear correlations were noticeable between the maternal vitamin D status and the gestational period. (Correlation=0.1907(0.0803,0.2965); P=0.0008).
No participant who had an adequate concentration of vitamin D had preeclampsia. However, one and two individuals incurred preeclampsia among women with vitamin D deficiency and insufficiency, respectively. Adjusted by age, BMI and gestational weight gain, there was no significant aOR for maternal vitamin D status with pregnancy complications including gestational diabetes mellitus, preterm birth and Caesarean section (Table 3).
|
Serum 25(OH)-D |
GDM |
PB |
CS |
||||
|
n(%) |
aoR |
n(%) |
aoR |
n(%) |
aOR |
||
|
Deficiency |
176 (57.52%) |
46 (56.79%) |
0.74 (0.35, 1.56) |
9 (5.11%) |
2.14 (0.26, 17.76) |
91 (51.7%) |
1.07 (0.56, 2.02) |
|
Insufficiency |
79 (25.82%) |
21 (25.93%) |
0.87 (0.37, 2.01) |
3 (3.80%) |
1.64(0.16, 16.99) |
38 (48.1%) |
0.93(0.45, 1.92) |
|
Sufficiency |
51 (16.67%) |
14 (17.28%) |
1 |
1 (1.96%) |
1 |
25 (49.0%) |
1 |
Table 3: Adjusted relative risks for pregnancy complications*.
Note: Data presented as n (%). χ2 test analysis of variances. * Adjusted for age, BMI and GWG. BMI: Body Mass Index; GWG: Gestational Weight Gain; GDM: Gestational Diabetes Mellitus; PB: preterm birth; CS: Cesarean section. There was no significant aOR for maternal vitamin D status with pregnancy complications including gestational diabetes mellitus (GDM), preterm birth (PB) and Caesarean section (CS).
Discussion
Vitamin D is a fat-soluble vitamin well known for its function in maintaining calcium homeostasis. Vitamin D has been implicated in modulation of other critical functions such as immune response, metabolism, and cell growth [17,18].
Except exposure to lack of sunlight, such as live in northern latitudes, wear long robes or head coverings for religious reasons et al, several factors are known to cause vitamin D deficiency, including age, kidney failure, malabsorption in the intestine, liver failure, and chronic inflammatory disease [19]. In addition, polypharmacy, the use of multiple medications in the management of diseases, can increase the risk of developing vitamin D deficiency. The prevalence of vitamin D deficiency is higher during pregnancy [20,21], and according to a systematic literature review, this prevalence is 54% worldwide [22]. Our study findings concur with this observation because more than half (57.5%) of pregnant women were found to have vitamin D deficiency. There is a large variation in the prevalence of vitamin D deficiency in pregnant women according to geographical location. The prevalence of deficiency in the UK is 20% [23], 78% in Iran [24], 86% in northern India [25], 28% in Australia and New Zealand [26], and 60–84% of pregnant non-Western women in the Netherlands [27].
Studies of vitamin D status (maternal serum 25(OH) D concentration) in pregnancy have mostly focused on the later stages of pregnancy and the associated adverse events such as preterm birth, gestational diabetes, and preeclampsia [28]. In a recent critical review, Woo et al. reported a positive correlation between vitamin D deficiency and preterm births [9]. However, the findings of the relationship between vitamin D deficiency and preeclampsia were inconclusive [9]. In an observational cohort study, Vivanti et al., found that a significant decrease in the risk of preeclampsia was associated with maternal vitamin D concentration ≥ 30 ng/mL in the third trimester (OR=0.34; 95% CI: 0.13-0.86. P=0.023) [29]. In our study, we found there was no preeclampsia in the vitamin D sufficiency group compared with two occurrences of preeclampsia in the vitamin D insufficiency group and one in the deficiency group. There was no significant difference for maternal vitamin D status with pregnancy complications including gestational diabetes mellitus, preterm birth, and Caesarean section.
However, we found an interesting phenomenon in our study. The maternal vitamin D concentrations in the group of mothers who delivered before the 39th gestational week were significantly lower than in the group of mothers who delivered after 39 weeks of gestation. And significant linear correlations were noticeable between the maternal vitamin D status and the gestational period in the vaginal delivery group. These findings suggest that vitamin D concentration may be related to the onset of labor.
The fact that CYP27B1 and VDR are expressed in placenta at early stages indicates the importance of vitamin D for placenta function and physiology. In addition to its potential antimicrobial and inflammatory activities, vitamin D might have a much broader functional spectrum in placenta. A study by Ganguly et al., performed trophoblast cells, ex vivo and in vitro, supports this concept [30].
Wagner et al. found that maternal vitamin D status in the third trimester was most significantly associated with preterm birth, thereby proposing that later intervention could be a rescue treatment to decrease the risk of preterm deliveries [31]. Vitamin D and its receptors may have an important function in the maintenance of pregnancy or the initiation of labor.
Our study was an observational design; thus, it was not possible to demonstrate causal relationships. We will increase the sample size in our next study and measure vitamin D concentration throughout the pregnancy with maternal and neonatal health outcomes and labor initiation.
Conclusion
Our study demonstrates that vitamin D deficiency is common among pregnant Chinese women and that the concentration of vitamin D may correlate with the advancement in pregnancy. Thus, Vitamin D and its receptor may have an important function in the initiation of labor, a proposal that requires further investigation.
Acknowledgment
The authors thank AiMi Academic Services (www.aimieditor.com) for English language editing and review services.
Funding
None.
Disclosure Statement
The authors whose names are listed certify that they have no affiliations with, or involvement in, any organization or entity with a financial interest or nonfinancial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials presented in this manuscript.
Ethical Consideration
This cross-sectional study was conducted between February 2017 and January 2019 at the Anzhen Hospital, China. All data were extracted from the hospital’s patient information system. The Research and Ethics Committee of Anzhen Hospital approved this study (Anzhen 18029X), and all study participants provided required informed consent. The investigators ensured strict confidentiality of participant information by delinking patient identifiers and by using study codes.
References
- Xu KQ (2014) Clinical biochemical examination. People's Medical Publishing House, China.
- Wacker M, Holick MF (2013) Vitamin D - effects on skeletal and extraskeletal health and the need for supplementation. Nutrients 5: 111-148.
- Agarwal S, Kovilam O, Agrawal DK (2018) Vitamin D and its impact on maternal-fetal outcomes in pregnancy: A critical review. Crit Rev Food Sci Nutr 58: 755-769.
- Yin K, Agrawal DK (2014) Vitamin D and inflammatory diseases. J Inflamm Res 7: 69-87.
- Boyle AK, Rinaldi SF, Norman JE, Stock SJ (2017) Preterm birth: Inflammation, fetal injury and treatment strategies. J Reprod Immunol 119: 62-66.
- Fabri M, Stenger S, Shin DM, Yuk JM, Liu PT, et al. (2011) Vitamin D is required for IFN-gamma-mediated antimicrobial activity of human macrophages. Sci Transl Med 3: 104.
- Qin LL, Lu FG, Yang SH, Xu HL, Luo BA (2016) Does Maternal Vitamin D Deficiency Increase the Risk of Preterm Birth: A Meta-Analysis of Observational Studies. Nutrients 8: 301.
- Obstet Gynecol (2020) Gestational Hypertension and Preeclampsia: ACOG Practice Bulletin. Obstet Gynecol 135: 237-260.
- Woo J, Giurgescu C, Wagner CL (2019) Evidence of an Association Between Vitamin D Deficiency and Preterm Birth and Preeclampsia: A Critical Review. J Midwifery Womens Health 64: 613-629.
- WHO (2020) WHO antenatal care recommendations for a positive pregnancy experience: Nutritional interventions update: Multiple micronutrient supplements during pregnancy. World Health Organization, Geneva, Switzerland.
- Mpondo BC, Ernest A, Dee HE (2015) Gestational diabetes mellitus: challenges in diagnosis and management. J Diabetes Metab Disord 14: 42.
- Lende M, Rijhsinghani A (2020) Gestational Diabetes: Overview with Emphasis on Medical Management. Int J Environ Res Public Health 17: 9573.
- Pan S, Huang C, Cheng H (2024) Risk Factors and Prevention Strategies for Gestational Diabetes in Asian Populations. JACC: Asia 4: 853-856.
- Wu X, Tiemeier H, Xu T (2025) Trends in gestational diabetes prevalence in China from 1990 to 2024: a systematic review and meta-analysis. Rev Endocr Metab Disord 26: 1009-1021.
- Zhang Y, Gong Y, Xue H, Xiong J, Cheng G (2018) Vitamin D and gestational diabetes mellitus: a systematic review based on data free of Hawthorne effect. Bjog 125: 784-793.
- Schoor N, Lips P (2017) Global Overview of Vitamin D Status. Endocrinol Metab Clin North Am 46: 845-870.
- Holick MF (2012) Evidence-based D-bate on health benefits of vitamin D revisited. Dermatoendocrinol 4: 183-190.
- Hewison M (2012) Vitamin D and the immune system: new perspectives on an old theme. Rheum Dis Clin North Am 38: 125-139.
- Ren C, Wang J, Niu G (2012) Modern clinical disease prevention and treatment. Zhengzhou University Press, China.
- Figueiredo ACC, Cocate PG, Adegboye ARA, Franco-Sena AB, Farias DR, et al. (2018) Changes in plasma concentrations of 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D during pregnancy: a Brazilian cohort. Eur J Nutr 57: 1059-1072.
- Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, et al. (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96: 1911-1930.
- Saraf R, Morton SM, Camargo CA, Grant CC (2016) Global summary of maternal and newborn vitamin D status-a systematic review. Matern Child Nutr 12: 647-68.
- Javaid MK, Crozier SR, Harvey NC, Gale CR, Dennison EM, et al. (2006) Maternal vitamin D status during pregnancy and childhood bone mass at age 9 years: a longitudinal study. Lancet 367: 36-43.
- Pirdehghan A, Vakili M, Dehghan R, et al. (2016) High Prevalence of Vitamin D Deficiency and Adverse Pregnancy Outcomes in Yazd, a Central Province of Iran. J Reprod Infertil 17: 34-38.
- Arora S, Goel P, Chawla D, Huria A, Arya A (2018) Vitamin D Status in Mothers and Their Newborns and Its Association with Pregnancy Outcomes: Experience from a Tertiary Care Center in Northern India. J Obstet Gynaecol India 68: 389-393.
- Wilson RL, Leviton AJ, Leemaqz SY, Anderson PH, Grieger JA, et al. (2018) Vitamin D levels in an Australian and New Zealand cohort and the association with pregnancy outcome. BMC Pregnancy Childbirth 18: 251.
- Meer IM, Karamali NS, Boeke AJ, Lips P, Middelkoop BJ, et al. (2006) High prevalence of vitamin D deficiency in pregnant non-Western women in The Hague, Netherlands. Am J Clinl Nutr 84: 350-353.
- Amegah AK, Klevor MK, Wagner CL (2017) Maternal vitamin D insufficiency and risk of adverse pregnancy and birth outcomes: A systematic review and meta-analysis of longitudinal studies. PLoS One 12: 0173605.
- Vivanti AJ, Monier I, Salakos E, Elie C, Tsatsaris V, et al. (2020) Vitamin D and pregnancy outcomes: Overall results of the FEPED study. J Gynecol Obstet Hum Reprod 49: 101883.
- Ganguly A, Tamblyn JA, Finn-Sell S, Chan SY, Westwood M, et al. (2018) Vitamin D, the placenta and early pregnancy: effects on trophoblast function. J Endocrinol 236: 93-103.
- Wagner CL, Baggerly C, McDonnell SL, Baggerly L, Hamilton SA, et al. (2015) Post-hoc comparison of vitamin D status at three timepoints during pregnancy demonstrates lower risk of preterm birth with higher vitamin D closer to delivery. J Steroid Biochem Mol Biol 148: 256-260.
Citation: Luo L, Shen F, Ye J, Yang D, Zhang J (2025) Relation between Maternal Vitamin D Concentration during Third Trimester and Maternal and Neonatal Health Outcomes: A Cross-Sectional Study in China. HSOA J Altern Complement Integr Med 11: 657.
Copyright: © 2025 Lianmei Luo, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

