
Relation of Affective Disorders in the Cognitive Decline of Disease Parkinson’s Patients
*Corresponding Author(s):
Madson Alan Maximiano-BarretoDepartamento De Gerontologia, Universidade Federal De São Calos, Rodovia Washington Luís, São Carlos, Brazil
Tel:+55 82999208149,
Email:mmaximianopsi@gmail.com
Abstract
Objective: To analyze the relation between affective disorders (Anxiety and Depression) and cognitive decline in Parkinson’s patients.
Methods: This is a cross-sectional non-probabilistic and intentional sampling study. We selected individuals diagnosed with Parkinson’s Disease (PD) aged 60 years or older treated in two outpatient clinics for movement disorders in the city of Maceió - AL. Sixty-two elderly were selected, 40 with depression, 22 without depression, 27 with anxiety and 35 without anxiety. We used a sociodemographic questionnaire, Geriatric Depression Scale (GDS-15 reduced version), Geriatric Anxiety Inventory (GAI), Rey’s Ear-Verbal Learning Test (RAVLT) and Montreal’s Cognitive Assessment (MoCA).
Results: In front of the sample composed of 62 elderly people, there was a high prevalence of female elderly people 64.5%, with a mean age of 62.51 years (±9.26). There was no statistically significant difference in the comparison between the groups (p>0.05). However, there was a significant relation between groups in RAVLT (p<0.001) in MoCA (p=0.018), in the areas of abstraction (p=044) and executive function (p=021). Regarding the relation between depressive symptoms and episodic memory impairment a moderate inverse correlation was identified (r=-282, p=0.027) and regarding the relation between anxiety and episodic memory impairment a statistically significant inverse relation was identified (r=-268, p=0.035).
Conclusion: The results point to a relation between a more severe episodic memory impairment in patients with PD who have affective disorders.
Keywords
Anxiety; Episodic memory; Depression, Parkinson's disease.
INTRODUCTION
Parkinson’s Disease (PD) is a neurodegenerative clinical condition, which influences the regulation of movements and emotions, occurring due to the loss of dopamine-producing neurons [1]. PD is, after Alzheimer’s disease, the second most common neurodegenerative disease, affecting about 1% of adults over 60 years [2]. Clinically, PD is defined by the presence of bradykinesia in combination with one or more of the following manifestations: muscle stiffness, resting tremor or postural instability [3]. These motor symptoms usually begin unilaterally and asymmetry persists throughout the course of the disease [4]. Among the non-motor manifestations that lead to greater impairment of independence and quality of life of individuals with PD are depression and anxiety, comorbidities that may contribute to cognitive decline [5]. Anxiety and depression are conditions commonly observed in patients with PD and are associated with a great loss of quality of life, regardless of the severity of motor symptoms [6].
According to D’Iorio [7], anxiety in PD patients is a risk factor for decreased attention, planning capacity, organization, cognition and consequently patients' perception of their quality of life. Depression is the most common non-motor manifestation of PD and is related to more severe neurological symptoms compared to patients with PD but without depression, which could indicate an advanced and generalized neurodegenerative process [8,9]. The World Health Organization estimates that depression will become the second most common disease in society by 2020, behind only cardiovascular diseases [10,11]. According to Pfeiffer [12] the progression of PD can worsen depression, which would be demonstrated by the loss of effectiveness of antidepressants used at the beginning of the disease.
There is no consensus whether the etiology of PD associated depression is organic or reactive, or both, but it is known that there is greater degeneration of dopaminergic neurons in the ventral mesencephalon in patients with PD who are depressed than those who are not [13,14]. In addition, serotonergic projections of the nuclei of the brainstem raffle suffer degeneration on PD, which can be an important abnormality in the etiology of depression associated with PD [15]. According to Wen [16], symptoms of apathy, depression and anxiety in PD present the fronto-stiatal circuits as a shared pathway in their pathogens. These circuits are responsible for processes such as emotion, executive functions and motivation, including scenario change, work memory and decision making [17,18]. In view of what was described above, the main objective of the present study is to analyze the relation between affective disorders and cognitive decline in Parkinson’s patients.
METHODS
A descriptive and cross-sectional study was carried out with individuals from 60 years of age with Parkinson’s disease attended at the movement disorder clinic of Hospital Universitário Professor Alberto Antunes - HUPAA/AL and at a Pestalozzi health unit in Maceió-AL.
PARTICIPANTS
The study was carried out with 62 elderly people of both sexes and on a voluntary basis, 44 female and 18 male participants, who were willing to participate in all stages of the research, as governed by the Term of Free and Informed Consent (TFIC).
INSTRUMENTS AND PROCEDURE
To collect the data, an interview with the participants was initially carried out through the application of a semi-structured questionnaire developed by the researchers with the objective of obtaining information such as gender, race, socioeconomic class, level of education, profession and other characteristics of the individual. Then, the following instruments were applied.
Rey Auditory-Verbal Learning Test (RAVLT)
The is an instrument developed by Rey in 1958, but for the present study the model adapted for Brazilian Portuguese developed by Malloy-Diniz [19] was used. This instrument contains a list of 15 nouns (List A) read clearly for 5 consecutive times, each time the examiner was asked to remember as many words as possible. At the end of this step another list of nouns (List B) was read only once and once again the volunteer was asked to repeat as many words as he or she could remember. After this step the participant was asked to remember the nouns that were presented in List A, without repeating the list again. In the last step, a list of 50 words was read so that the participant could recognize the words that were read on the A List.
Geriatric Anxiety Inventory (GAI)
The GAI is an instrument used to assess anxiety symptoms. It was developed by Pachana et al., [20]. In the preset study, the Brazilian version adapted by Martiny et al., [21] was used. It consists of 20 questions with the following answers: I agree or disagree. The sum of the answers agrees >10 characterize the individual with the anxiety symptoms.
Geriatric Depression Scale (GDS-15)
The GDS is a 30-question scale with dichotomous answers (yes/no) developed by Yesavage [22] for depression screening in the elderly. The GDS-15 has 15 questions with a 5/6 (no case/case) score. The validation of the GDS-15 performed in a geriatric outpatient clinic showed that the scale is self-applicable and presents a significant sensitivity [23].
Montreal Cognitive Assessment (MoCA)
The instrument that allows the identification of a decline in cognition and mainly aims at screening for Light Cognitive Compromise (MCC). It was developed by Nasreddine e colaboradores [24]. In the present study, the Brazilian version adapted by Sarmento [25] was used, such instrument allows to evaluate aspects such as: trail alternation, viso-constructive abilities, nomination, memory, attention, sentence replication, verbal fluency, abstraction, late evocation and orientation. The total value of points of MoCA is equal to 30 and the value of its score is >26. Lower values may indicate mild cognitive impairment. Individuals with less than 12 years of schooling add 1 point to the score value.
STATISTICAL ANALYSIS
After filling the instruments of the research, the statistical analysis was performed through the Statistical Package for the Social Sciences (SPSS) version 23.0 program in a descriptive way by relative frequency (percentage), standard deviation and, afterwards, inductive tests like the Chi-square will also be used to demonstrate if there is or not a relation between variables and the Pearson correlation test to define if variables are directly or inversely proportional.
RESULTS
Sixty-two patients were interviewed, 33 of them in the Movement Disorders Clinic of the University Hospital and 29 in the Pestalozzi Association of Maceió. The mean age of the participants is 62.51 years (SD = ±9.26). Of the 62 patients, 64.5% (n=40) presented depressive symptoms, with a prevalence in female individuals of 65% (n=26) and 43.5% (n=27) presented anxiogenic symptoms. No static differences were identified between the groups, regarding gender (p=0.166), education (p=0.357) and ethnicity (p=0.458). The general characterization of the sample is presented in table 1.
|
Variables |
N |
% |
|
Age |
62.51 (±9.26) |
|
|
Gender |
||
|
F |
44 |
7.0% |
|
M |
18 |
29.0% |
|
Ethnicity |
||
|
White |
21 |
33.9% |
|
Black |
9 |
14.5% |
|
Yellow |
1 |
1.6% |
|
Brown |
31 |
50.0% |
|
Education |
6.43 (±5.28) |
|
Table 1: Sociodemographic characterization of patients with Parkinson’s disease, Maceió-AL, 2019.
Regarding the clinical analysis through MOcA and RALVT, it is observed that the depressive symptomatology presents a statistically significant relation in the cognitive damage, mainly in the domains of executive function and abstraction, as well as in the damage of the episodic memory, as shown in table 2.
|
Variables |
Total (n = 62) |
P |
|
|
|
Depression |
Anxiety |
|
|
RAVLT |
9.12 (±3.89) |
0.001** |
0.001** |
|
MOcA |
17.22 (±5.79) |
0.027* |
0.035* |
|
Executive function |
2.03 (±1.69) |
0.003** |
0.181 |
|
Fluency |
2.22 (±0.79) |
0.538 |
0.265 |
|
Orientation |
0.96 (±0.84) |
0.149 |
0.272 |
|
Calculation |
0.69 (±0.46) |
0.16 |
0.444 |
|
Abstraction |
2.00 (±1.00) |
0.079 |
0.404 |
|
Evocation late |
0.91 (±0.79) |
0.282 |
0.333 |
|
Visual perception |
0.46 (±0.50) |
0.062 |
0.244 |
|
Nomination |
1.08 (±0.85) |
0.393 |
0.038* |
|
Attention |
0.82 (±1.18) |
0.981 |
0.072 |
|
Design test |
5.32 (±1.25) |
0.246 |
0.326 |
Table 2: Relation of affective disorders and cognitive decline in patients with Parkinson’s disease, Maceió-AL, 2019.
*Significance level p<0.005; **Significance level p<0.00
In order to correlate the prevalence of depressive symptoms and the loss of episodic memory, figure 1 demonstrates a statistically significant inverse (r=-282, p=0.027) correlation that identifies the relation of depression with the decline of this memory.
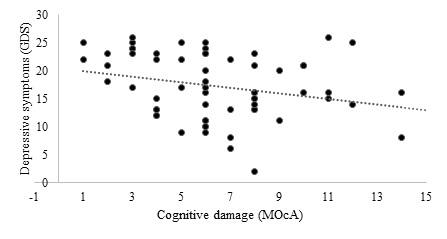 Figure 1: Relation between depressive symptoms and episodic memory among patients with Parkinson’s disease, Maceió-AL, 2019.
Figure 1: Relation between depressive symptoms and episodic memory among patients with Parkinson’s disease, Maceió-AL, 2019.
In order to verify the relation between anxiogenic symptomatology and cognitive impairment relative to episodic memory, figure 2 demonstrates a statistically significant inverse (r=-268, p=0.035) relation in which a relation between impairment of episodic memory and anxiety is detected.
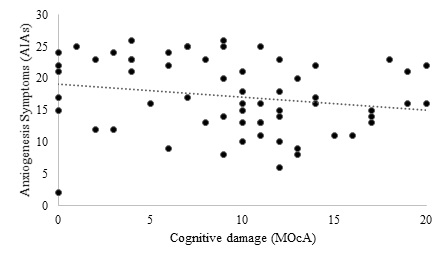 Figure 2: Relation between anxiogenic symptoms and episodic memory among patients with Parkinson’s disease, Maceió-AL, 2019.
Figure 2: Relation between anxiogenic symptoms and episodic memory among patients with Parkinson’s disease, Maceió-AL, 2019.
DISCUSSION
The impairment of episodic memory is an expected phenomenon in aging, especially in the elderly with low schooling, in those who do not perform control activities or in those with neurodegenerative pathologies such as Parkinson’s disease [26]. Among the non-motor manifestations that lead to greater impairment of independence and quality of life of individuals with PD are depression and anxiety, comorbidities that may contribute to cognitive decline [5]. A literature review by Nakabayashi et al., [27] demonstrated a prevalence of 1.8% to 68.1% of depression in patients with PD, a variation that can be explained by the methodology employed in each study. Regarding the occurrence of PD and anxiety, the study conducted by Richard et al., [28] demonstrated prevalence higher than 40%.
There is still no consensus regarding the etiology of depression associated with PD, whether it is organic, reactive or presents a mixed etiology, but it is known that there is a greater degeneration of dopaminergic neurons in the ventral mesencephalon in patients with PD who are depressed than in those who are not [12,13]. Moreover, it was found that patients diagnosed with PD and Depression present with more severe neurological symptoms, indicating an advanced and generalized neurodegenerative process [9]. According to the systematic review of neuroimaging studies by Wen et al., [16], symptoms of apathy, depression and anxiety in patients with PD present the fronto-stratrial circuits as a shared pathway in their pathogens. These circuits are responsible for processes such as emotion, executive functions and motivation, including scenario change, work memory and decision making [17,18].
The present study analyzed 62 patients with PD, showing a higher prevalence of the disease in females. Among the participants we found a number of 44 female and 18 male patients affected by PD. Parallel to this study, discussions on the conflicting results regarding the epidemiology of affective disorders involved in PD were evidenced in review studies [29,30]. Such reviews demonstrated the male gender as the most affected by PD while in clinical trials the female gender seemed to be the most affected, something demonstrated by Gda?ska et al., [31], which explained their results based on the cutout made in the population study. Hammen [32], in his review, listed risk factors for the development of affective disorders such as bereavement, family history, sedentariness, low socioeconomic and school level, daily stress and being female, data that corroborate to explain the epidemiological divergence found in this study. Besides these factors, there is an epidemiological association with the pathophysiology of PD, which involves nigrostriatal degeneration, one of the sites with wide connections to the limbic system (center responsible for emotional control) and the process of feminization, which may contribute to explain the higher proportion of women found in the current study [33,34].
Although this study contains specific validated instruments for the elderly, it also presents limitations because it is a cross-sectional study, which implies difficulty in identifying which comorbidity, anxiety or depression was first presented in the analyzed PD patient, besides the temporal loss between such comorbidities and the onset of PD presentation itself. Additionally, this study has a small heterogeneous sample to be analyzed, which contributes to less generalized results.
CONCLUSION
It is noted that patients diagnosed with PD and affective disorders present with more severe cognitive impairment, especially of episodic memory, when compared to patients diagnosed with PD only. It was noticed that the occurrence of depression and anxiety is directly proportional to episodic memory loss. Furthermore, it was noted that there is an epidemiological difference in cases of PD in the city of Maceió - AL regarding the prevalence between the sexes, being the disease more present in females, while other studies show a higher overall prevalence of involvement in males. Due to the wide finding of depression and anxiety in patients with PD and the clinical importance that the relation between these diseases represents for the patient it was expected to find a greater number of studies aiming at correlating PD, affective disorders and episodic memory in the literature. Thus, the development of more scientific production in this area of research should be stimulated to improve the epidemiological and pathophysiological accuracy of the relation between PD and the comorbidities worked on in this study.
DISCLOSURE
No conflicts of interest declared concerning the publication of this article.
REFERENCES
- Bhat S, Acharya UR, Hagiwara Y, Dadmehr N, Adeli H (2018) Parkinson’s disease: Cause factors, measurable indicators, and early diagnosis. Comput Biol Med 102: 234-241.
- Hirtz D, Thurman DJ, Gwinn-Hardy K, Mohamed M, Chaudhuri AR, et al. (2007) How common are the "common" neurologic disorders? Neurology 68: 326-337.
- van der Hoek TC, Bus BA, Matui P, van der Marck MA, Esselink RA, et al. (2011) Prevalence of depression in Parkinson’s disease: Effects of disease stage, motor subtype and gender. J Neurol Sci 310: 220-224.
- Hughes AJ, Daniel SE, Kilford L, Lees AJ (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: A clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55: 181-184.
- Randver R (2018) Repetitive transcranial magnetic stimulation of the dorsolateral prefrontal cortex to alleviate depression and cognitive impairment associated with Parkinson’s disease: A review and clinical implications. J Neurol Sci 393: 88-99.
- Yamanishi T, Tachibana H, Oguru M, Matsui K, Toda K, et al. (2013) Anxiety and depression in patients with Parkinson’s disease. Intern Med 52: 539-545.
- D'Iorio A, Vitale C, Piscopo F, Baiano C, Falanga AP, et al. (2017) Impact of anxiety, apathy and reduced functional autonomy on perceived quality of life in Parkinson’s disease. Parkinsonism Relat Disord 43: 114-117.
- Radhakrishnan DM, Goyal V (2018) Parkinson’s disease: A review. Neurol India 66: 26-35.
- Chen PH, Cheng SJ (2008) Depression in Parkinson Disease: Current Understanding and Treatment. International Journal of Gerontology 2: 172-182.
- Pålhagen SE, Carlsson M, Curman E, Wålinder J, Granérus AK (2008) Depressive illness in Parkinson’s disease--indication of a more advanced and widespread neurodegenerative process? Acta Neurol Scand 117: 295-304.
- Murray CJ, Lopez AD (1997) Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet 1997: 1498-1504.
- Pfeiffer HC, Løkkegaard A, Zoetmulder M, Friberg L, Werdelin L (2014) Cognitive impairment in early-stage non-demented Parkinson’s disease patients. Acta Neurol Scand 129: 307-318.
- Leentjens AF (2004) Depression in Parkinson’s disease: Conceptual issues and clinical challenges. J Geriatr Psychiatry Neurol 17: 120-126.
- Mann JJ, Kapur S (1995) A dopaminergic hypothesis of major depression. Clinical Neuropharmacolog 18: 57-65.
- Okun MS, Watts RL (2002) Depression associated with Parkinson’s disease: clinical features and treatment. Neurology 58: 63-70.
- Wen MC, Chan LL, Tan LCS, Tan EK (1001) Depression, anxiety, and apathy in Parkinson’s disease: Insights from neuroimaging studies. Eur J Neurol 23: 1001-1019.
- Puig MV, Antzoulatos EG, Miller EK (2014) Prefrontal dopamine in associative learning and memory. Neuroscience 282: 217-229.
- Paulo DLV, Yassuda MS (2010) Queixas de memória de idosos e sua relação com escolaridade, desempenho cognitivo e sintomas de depressão e ansiedade. Revista de Psiquiatria Clínica 37: 23-26.
- Malloy-Diniz LF, Fuentes D, Abrantes SSC, Lasmar VAP, Salgado JV (2003) O Teste de Aprendizagem Auditivo-Verbal de Rey (RAVLT) normas para uma população brasileira. Revista Brasileira de Neurologia 36: 79-83.
- Pachana NA, Byrne GJ, Siddle H, Koloski N, Harley E, et al. (2007) Development and validation of the Geriatric Anxiety Inventory. Int Psychogeriatr 19: 103-114.
- Martiny C, e Silva ACO, Nardi AE, Pachana NA (2011) Tradução e adaptação transcultural da versão brasileira do Inventário de Ansiedade Geriátrica (GAI). Archives of Clinical Psychiatry (São Paulo) 38.
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, et al. (1982) Development and validation of a geriatric depression screening scale: A preliminary report. J Psychiatr Res 17: 37-49.
- Paradela EMP, Lourenço RA, Veras RP (2005) Validação da escala de depressão geriátrica em um ambulatório geral. Revista de Saúde Pública 39: 918-923.
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, et al. (2005) The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53: 695-699.
- Sarmento ALR (2009) Apresentação e aplicabilidade da versão brasileira da MoCA (Montreal Cognitive Assessment) para rastreio de Comprometimento Cognitivo Leve. Trabalho de Conclusão de Curso, Dissertação (Mestrado), Universidade Federal de São Paulo, São Paulo, Brazil.
- Maass A, Lockhart SN, Harrison TM, Bell RK, Mellinger T, et al. (2018) Entorhinal Tau Pathology, Episodic Memory Decline, and Neurodegeneration in Aging. J Neurosci 38: 530-543.
- Nakabayashi TIK, Chagas MHN, Corrêa ACL, Tumas V, Loureiro SR, el al. (2008) Prevalência de depressão na doença de Parkinson. Archives of Clinical Psychiatry 35: 219-227.
- Richard IH, Schiffer RB, Kurlan R (1996) Anxiety and Parkinson’s disease. The Journal of Neuropsychiatry and Clinical Neurosciences 8: 383-392.
- Schrag A, Taddei RN (2017) Depression and Anxiety in Parkinson’s Disease. Int Rev Neurobiol 133: 623-655.
- Abbas MM, Xu Z, Tan LCS (2018) Epidemiology of Parkinson’s Disease-East Versus West. Mov Disord Clin Pract 5: 14-28.
- Gda?ska P, Drozdowicz-Jastrz?bska E, Grzechoci?ska B, Radziwon-Zaleska M, W?grzyn P, et al. (2017) Anxiety and depression in women undergoing infertility treatment. Ginekol Pol 88: 109-112.
- Hammen C (2018) Risk Factors for Depression: An Autobiographical Review. Annu Rev Clin Psychol 14: 1-28.
- Kalia LV, Lang AE (2015) Parkinson’s disease. Lancet 386: 896-912.
- Bezerra ALA, Bezerra DS, Pinto DS, Bonzi ARB, de Pontes RMN, et al. (2018) Perfil epidemiológico de idosos hipertensos no Brasil: Uma revisão integrativa. Revista de Medicina 97: 103-107.
Citation: Aguiar IM, Costa CFPA, Neto JAR, dos Santos JB, de Farias WM, et al. (2020) Relation of Affective Disorders in the Cognitive Decline of Disease Parkinson’s Patients. J Gerontol Geriatr Med 6: 045.
Copyright: © 2020 Iago Moura Aguiar, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

