
Resection of Laterocervical Schwannoma through a Robot-Assisted Axillary Approach: A Case Report
*Corresponding Author(s):
Laus MelissaFatebenefratelli San Giovanni Calibita Hospital, Roma, Italy
Tel:+39 3492691956,
Email:melissa.laus@hotmail.it
Abstract
Schwannoma is a benign tumor arising from schwann cells in peripheral, cranial, and autonomic nerve sheaths. It is rarely found in the head and neck. It is usually asymptomatic, biochemically non-secretory and functionally inactive. In this study, a 23-year-old woman patient presenting with a nodule (12x13x20 mm) outside the thyroidal tissue and diagnosed as a schwannoma after total excision was presented.
Keywords
INTRODUCTION
Usually the patient requires medical ENT specialist advice for the appearance of a laterocervical swelling with-out referring to particular disturbance. Ultrasound as a first level examination, possibly accompanied by a CT scan of the neck, allows an appropriate study of the neoformation [2].
Open surgery of the neck to date has represented the therapeutic option of choice for the excision of these neoplasms [3]; in recent times, robotic surgery has given the possibility of guaranteeing complete surgical excision in the face of less extensive surgical accesses with a gain in postoperative recovery and aesthetic result, very important especially in younger patients [4].
PATIENT AND METHOD
Patient
The initial diagnostic hypothesis, in relation to the anatomical site of the neoformation and to the haematochemical tests performed in the endocrinological controls was of suspected parathyroid adenoma. For this reason no further second level radiolgic examinations were performed. In the hypothesis of a neoformation originating from the cranial nerves we would have required an MRI that shows specific signs of neural sheath neoplasms. In the suspicion of a parathyroid adenoma, an ultrasound-guided needle aspiration was performed; the result of the cytological examination did not highlight the presence of epithelial cellular elements and negative for neoplastic cells. The lack of a certain histological diagnosis in addition to the patient's desire to carry the mass, led us to the decision to perform a robot assisted excision to minimize the surgical trauma, even considering the young age of the patient.
SURGICAL PROCEDURE

Figure 1: Drawing of the skin incision at the level of the lateral margin of the right pectoralis major muscle.
Through this dissection plane a tunnel was sculpted until the sternocleidomastoid muscle was visualized; at this point, the clavicular and sternal heads are isolated and the dissection continued in the vascular triangle between the two muscular heads. The positioning of a Chung's retractor increased visual exposure on the thyroid and laterocervical space.
The Da Vinci Surgical System Xi (Intuitive Surgical Sunnyvale, CA, USA) was introduced; the 30° endoscope, left and right robotic arm were inserted through the axillary incision. Chung's retractor, elevating the skin flap, allows obtaining a wide viewing and maneuvering space, avoiding that the robotic arms can come into conflict during surgical maneuvers.
The neoplasm has been progressively detached from the surrounding planes and removed; extemporaneous histological examination at the freezer did not show the presence of epithelial cells. The macroscopic aspect deposited for a schwannoma (Figure 2); in this regard, a rosary aspect of the omolateral recurrent laryngeal nerve was also reported (Figure 3).
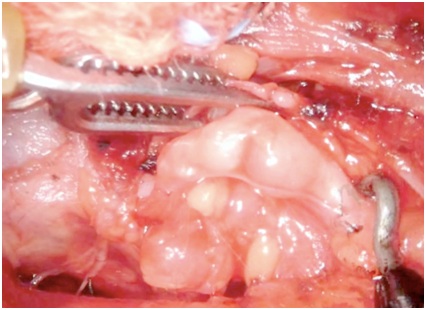
Figure 2: Characteristic rosary conformation of the schwannoma of the right recurrent laryngeal nerve.
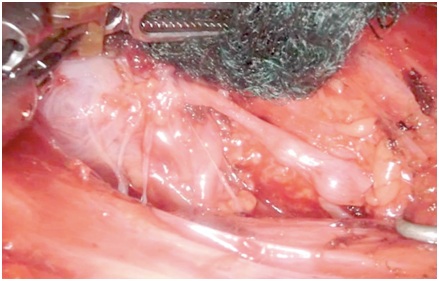
Figure 3: Identification of the right recurrent laryngeal nerve upon its entry into the larynx.
Effected an accurate hemostasis with the bipolar forceps of the left robotic arm, a suction drainage was placed in the surgical space. The suture was performed for layers with detached Vicryl 3/0 points for the subcutaneous tissue and Vicryl R 4/0 intradermal for the skin.
RESULTS
DISCUSSION
The robotic surgery, even if performed in a narrower operative field, allows a wide vision of the laterocervical anatomical spaces, with an enlargement and a contrast of colors that makes evident anatomical details otherwise not recognized to the naked eye; for this reason a correct execution and orientation of the subcutaneous tunnel previously described is indispensable.
Our patient, a young woman of 23, was discharged on the second postoperative day without any visible wound at the laterocervical level and without any noticeable discomfort.
To say that the aesthetic factor is the only advantage of robotic surgery appears to be quite reductive, especially considering the faster recovery times compared to open surgery, due to the lower invasiveness and greater surgical precision that this method also allows at the neck level.
The most frequent postoperative complications are super imposable between the two accesses: paresis-paralysis of the vocal cords (2.6 of cases, definitive in 13.8% of these cases and transient in 86.2%), hematomas, seromas, infection of the surgical site 3% of cases had transient brachial nerve paralyses due to overstretching of the lesion side arm which resolved with conservative treatment. Only nine studies reported the discharge time, with a mean of 2.4 ± 1.2 days after surgery. The postoperative cosmetic results were good. The small incision scar in the axilla was completely covered when the patient's arm in natural position. Most of the subjective parameters (hypoesthesia or paraesthesia in the neck or anterior chest wall and difficulty swallowing) improved within 6 months.
CONCLUSION
REFERENCES
- Rohaizam J, Tang IP, Jong DE, Tan TY, Narihan MZ (2012 ) Cervical schwannoma: Report of four cases. Med J Malaysia 67: 345-348.
- Chiofalo MG, Longo F, Marone U, Franco R, Petrillo A, et al. (2009) Cervicalvagalschwannoma. A case report. Acta Otorhinolaryngol Ital 29: 33-35.
- Kim SH, Kim NH, Kim KR, Lee JH, Choi HS (2010) Schwannoma in head and neck: Preoperative im-aging study and intracapsular enucleation for functional nerve preservation. Yonsei Med J 51: 938-942.
- Ishikawa N, Kawaguchi M, Moriyama H, Oda M, Watanabe G (2012) Robot-assisted resection of multiple schwannomas of the neck and mediastinum through an axillary approach. Artif Organs 36: 647-648.
- Mierzwi?ski J, Wrukowska I, Tyra J, Paczkowski D, Szcze?niak T, et al. (2018) Diagnosis and manage-ment of pediatric cervical vagal schwannoma. Int J PediatrOtorhinolaryngol 114: 9-14.
Citation: Guido PC, Simone B, Melissa L, Luca F (2019) Resection of Laterocervical Schwannoma through a Robot-Assisted Axillary Approach: A Case Report. J Otolaryng Head Neck Surg 5: 027.
Copyright: © 2019 Ciabatti Pier Guido, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

