Journal of Medicine Study & Research Category: Medical
Type: Case Report
Reversal of Impaired Blood Flow of the Basal Ganglion from the Prior Focal Perfusion Defect in a Case of Ischemic Infarction: Observation during the Two Stages of Administration of Intravenous Laser Irradiation of Blood
*Corresponding Author(s):
Shin-Tsu ChangDepartment Of Physical Medicine And Rehabilitation, Tri-Service General Hospital, School Of Medicine, National Defense Medical Center, Chung Shan Medical University, No.161, Sec. 6, Minquan East Road, Neihu District, Taipei,Taichung, Taiwan, Province Of China
Tel:+886 423741350,
Fax:+886 945605523
Email:ccdivlaser1959@gmail.com
Received Date: Aug 21, 2019
Accepted Date: Aug 30, 2019
Published Date: Sep 06, 2019
Abstract
Cerebral infarction is a serious problem because of its prognosis and influence to rest of life of survivors. It may affect many aspects of patient’s daily function, such as movement, thinking, speech and cognitive function. Intravenous laser irradiation is a novel therapy in recent decades for stroke. Evidence has shown that it can improve rheological properties of blood so that can improve the blood flow of brain and enhance neurological recovery. It has also been proved positive effect for limbs movement after cerebral infarction. We present a case of left MCA cerebral infarction that limb movement as well as cognitive function improves after nine courses of intravenous laser irradiation of blood. Single Photon Emission Computed Tomography (SPECT) of brain was conducted before and twice after our administration. The local perfusion of right basal ganglion was found as impaired in the second brain SPECT, but the perfusion defect reversed vividly in the third SPECT. We believe that the phenomenon of initial decrease and later increase in the basal ganglion perfusion should be highly related to our ILIB administration.
Except for the theory of the rheological effect of ILIB therapy, we assume the redistribution of brain blood flow contribute the phenomenon of interval change of right basal ganglion. Based on the clinical pictures and our SPECT findings, we confirm that SPECT image is a very worthwhile tool in the field of scintigraphic rehabilitation for monitoring the neural recovery. ILIB is also a fabulous intervention to improve the circulation of ischemic brain and simultaneously enhance the neurological recovery, such as cognitive dysfunction.
Except for the theory of the rheological effect of ILIB therapy, we assume the redistribution of brain blood flow contribute the phenomenon of interval change of right basal ganglion. Based on the clinical pictures and our SPECT findings, we confirm that SPECT image is a very worthwhile tool in the field of scintigraphic rehabilitation for monitoring the neural recovery. ILIB is also a fabulous intervention to improve the circulation of ischemic brain and simultaneously enhance the neurological recovery, such as cognitive dysfunction.
Keywords
Basal ganglion; Blood flow; Cognitive impairment; Laser irradiation; Laser phototherapy; Single photon emission computed tomography
INTRODUCTION
Cognitive function has been known to be impaired by any cerebral events such as seizure, head injury or cerebral infarction. Impairment of cognition means a decline from previous level of function which interferes with daily life and independence that decrease quality of life and cause burden to caregiver and the whole society.
In recent decades, Intravenous Laser Irradiation of Blood (ILIB) has been established to be able to enhance rheological properties of the blood as well as improvement of microcirculation and reduction of the area of infarction [1]. In addition, nuclear medicine in neuroscience, primarily via tomography methods, for instance, Single Photon Emission Computed Tomography (SPECT), has been a significant function to monitor the hemodynamic and metabolic consequences of cerebrovascular diseases [2-5].
We will introduce a case of ischemic infarction whose cognitive function significantly improved corresponding to the changes on a series of brain SPECTs after the administration of ILIB.
In recent decades, Intravenous Laser Irradiation of Blood (ILIB) has been established to be able to enhance rheological properties of the blood as well as improvement of microcirculation and reduction of the area of infarction [1]. In addition, nuclear medicine in neuroscience, primarily via tomography methods, for instance, Single Photon Emission Computed Tomography (SPECT), has been a significant function to monitor the hemodynamic and metabolic consequences of cerebrovascular diseases [2-5].
We will introduce a case of ischemic infarction whose cognitive function significantly improved corresponding to the changes on a series of brain SPECTs after the administration of ILIB.
Case presentation
A 73-year-old man had history of smoking 1.5~2 PPD for more than 40 years, and newly diagnosed as type 2 diabetes mellitus and dyslipidemia in recent month. He was admitted to our hospital for dysphagia, global aphasia, right central facial palsy and right limbs weakness after ischemic infarction of left Middle Cerebral Artery (MCA) territory. He was just treated with r-TPA thrombolysis and underwent 1-month physical therapy, occupational therapy and speech therapy prior this hospitalization. Due to persisted dysphagia, aphasia and limbs weakness, as well as severe dysfunction of cognition, we provided him ILIB for further neurological recovery, which method of approach has been previously detailed [6].
His brain MRI in the acute phase of stroke revealed infarcts in left cerebral hemisphere, including left temporal-occipital lobe, left corona radiata and external capsule as well as some subacute to old lacunar infarcts at right frontal lobe, right corona radiata, right external capsule, bilateral anterior limb of internal capsules, bilateral putamen and bilateral thalamus (Figure 1). His first SPECT was performed on 2017/06/29 and showed hypoperfusion of left cerebral hemisphere, left striatum, left thalamus and right cerebellum, as well as uneven perfusion over the right parietal and right frontal regions (Figure 2).
His brain MRI in the acute phase of stroke revealed infarcts in left cerebral hemisphere, including left temporal-occipital lobe, left corona radiata and external capsule as well as some subacute to old lacunar infarcts at right frontal lobe, right corona radiata, right external capsule, bilateral anterior limb of internal capsules, bilateral putamen and bilateral thalamus (Figure 1). His first SPECT was performed on 2017/06/29 and showed hypoperfusion of left cerebral hemisphere, left striatum, left thalamus and right cerebellum, as well as uneven perfusion over the right parietal and right frontal regions (Figure 2).
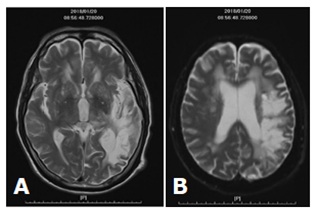
Figure 1:MRI findings of our case.
(A) Fluid-attenuated inversion recovery image demonstrates diffuse T2 hyperintensity throughout the left cerebral hemisphere.
(B) Diffusion-weighted image demonstrates diffusion hyperintensity throughout the left cerebral hemisphere.
(A) Fluid-attenuated inversion recovery image demonstrates diffuse T2 hyperintensity throughout the left cerebral hemisphere.
(B) Diffusion-weighted image demonstrates diffusion hyperintensity throughout the left cerebral hemisphere.
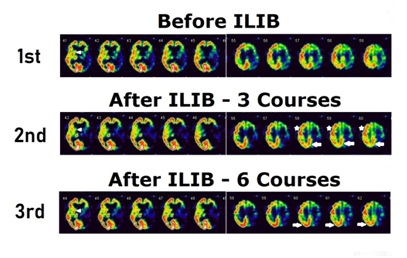
Figure 2:: Consecutive alterations of regional cerebral perfusion SPECTs.
(A) The 1st Brain SPECT tested on 2017/06/29. Right basal ganglion is obvious (arrowhead).
(B) The 2nd Brain SPECT tested on 2018/02/22. A relative hypoperfusion in the right basal ganglion/putamen was seen (arrowhead) when compared with the 1st SPECT. Prior uneven hypoperfusion in the right parietal region improved (arrow) and which in the right frontal region resolved (star*). Stable hypoperfusion in the left cerebral hemisphere, left striatum, and left thalamus persisted.
(C) The 3rd Brain SPECT tested on 2018/10/23. The perfusion in the right striatum and possible left caudate nucleus relatively improved, e.g. the circulatory defect of the right basal ganglion reversed (arrowhead). Hypoperfusion in the left cerebral hemisphere, left striatum, and left thalamus stably persisted. Prior hypoperfusion in the right parietal (arrow) and right frontal region improved as before.
(A) The 1st Brain SPECT tested on 2017/06/29. Right basal ganglion is obvious (arrowhead).
(B) The 2nd Brain SPECT tested on 2018/02/22. A relative hypoperfusion in the right basal ganglion/putamen was seen (arrowhead) when compared with the 1st SPECT. Prior uneven hypoperfusion in the right parietal region improved (arrow) and which in the right frontal region resolved (star*). Stable hypoperfusion in the left cerebral hemisphere, left striatum, and left thalamus persisted.
(C) The 3rd Brain SPECT tested on 2018/10/23. The perfusion in the right striatum and possible left caudate nucleus relatively improved, e.g. the circulatory defect of the right basal ganglion reversed (arrowhead). Hypoperfusion in the left cerebral hemisphere, left striatum, and left thalamus stably persisted. Prior hypoperfusion in the right parietal (arrow) and right frontal region improved as before.
After three courses of ILIB, we observed that his Wernicke's aphasia and dysphagia improved gradually. At outpatient visit, his muscle power of right limbs improved from 1 to 4 points. His cognitive function also improved remarkably. The second brain SPECT performed on 2018/02/22 showed uneven hypoperfusion in the right parietal region improved and which in the right frontal region resolved. Stable hypoperfusion in the left cerebral hemisphere, left striatum, left thalamus and right cerebellum. However, Improved unevenly decreased radioactivity in the right parietal region and resolved in the right frontal region. Surprisely, there was a relative hypoperfusion in the right putamen when compared with the previous study.
Patient requested for another six courses of ILIB, and after then, the third brain SPECT performed on 2018/10/23 showed, except stable hypoperfusion in the left cerebral hemisphere, left striatum, left thalamus and right cerebellum, relatively improved perfusion in the left occipital region, right striatum and possible left caudate nucleus occurred. Figure 3 showed the time interval in the two stage of ILIB. Table 1 summarized the changes in individual neural area observed from the three times SPECT.
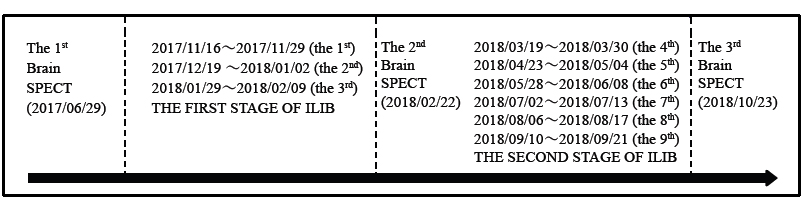 Figure 3: Time interval in the procedure of ILIB.
Figure 3: Time interval in the procedure of ILIB.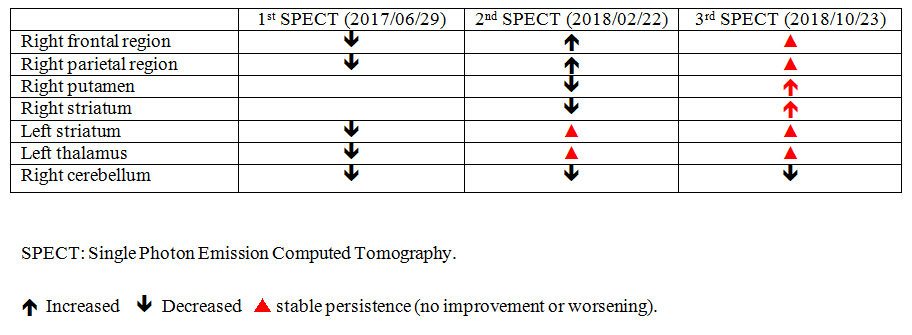
Table 1: : Perfusion changes of varying brain areas in three times of SPECT.
DISCUSSION
Based on the observation of the consecutive brain perfusion images, local perfusion of right basal ganglion was found as impaired in the second Brain SPECT, but the perfusion defect reversed vividly in the third SPECT. We believe that the phenomenon of initial decrease and later increase in the basal ganglion should be highly related to our ILIB administration.
In our case, initial symptoms were global aphasia, dysphagia, numbness and weakness of right limbs and unsteady gait. Limited improvement of his speech, comprehension, and limbs movement after 1 month of intensive physical therapy, occupational therapy and speech therapy, before ILIB was introduced. Brain SPECT showed hypoperfusion of left hemisphere, left striatum, left thalamus was found, which was compatible for his clinical symptoms. After three courses of ILIB, he can obey order and limbs movement as well as dysphagia improved gradually. Muscle power of left limbs improved from MRC grading 1 to 3. The second brain SPECT showed an improvement of prior perfusion deficit at right frontal and parietal regions, although a new deficit at right putamen region took place.
After the second stage of administration, e.g. the another six courses of ILIB, our case present a dramatic change of cognitive function, such as perceptual-motor function, language, executive function, and social cognition, which was compatible with the findings of third SPECT, e.g. increased uptake in right striatum.
Cognitive function refers to multiple neuropsychological issues, including attention, memory, calculation, communication, perception, self-awareness, problem solving, thinking flexibility, personality, stress coping and even interpersonal relationship. The basal ganglion has been known as crucial elements in the circuits of movement, learning and cognitive function. The striatum, one of the structures of basal ganglion divided into ventral and dorsal subdivision, based on function and connections. The ventral striatum is associated with limbic system and has been thought as an important part of the circuitry for decision making and reward-related behavior; the dorsal striatum is composed of the caudate nucleus and the putamen. The striatum is the major input region of basal ganglion and receives its major input from the cortex, while the globus pallidus and substantia nigra are the major output regions. The input and output regions are connected via direct and indirect pathways that have reciprocal effects on the basal ganglia output pathway, which control motor function. Cortical loops integrating the cortex and the basal ganglia are now accepted to play an important role in regulating behavioral, emotional and cognitive functions [7,8]. Impairment of those areas, including degeneration or hypoperfusion [9,10], may cause dysfunction of cognitive function, motivational salience, certain motor or executive functions that result in some neurologic or psychiatric disorders such as Parkinsonism diseases, Huntington's disease, bipolar disorder or dementia [11,12]. An observational study found that patients with putaminal stroke impaired motor imaginary, which result them unable to follow the instructions [13]. The fact of initial decrease and later increase in the blood flow of striatum was strongly correlated with the series of clinical pictures of our patient.
In recent decades, ILIB has been thought to improve rheological properties of the blood, to improve microcirculation, and reducing the area of infarction. It was developed for the treatment of cardiovascular diseases originally, but many studies showed various effects on many organs and on the hematologic and immunologic system [14], for instance, such as diminishing tendency of aggregation of thrombocytes [15-17], improved oxygen supply and wound healing, normalization of the metabolism of hypoxic tissue, positive effect on anti-inflammation and immunologic activity by modulation of cytokines and immune system [18,19]. ILIB has benefits in diaschisis reversal, motor cortex dysfunction, and reduction of homocysteine in our published case reports [6,20,21]. Regarding the risks involved with ILIB therapy, patients with history of seizure attack and ICH in recent 6 months should be prohibited.
The reason why local perfusion of right basal ganglion impaired in the second Brain SPECT, compared with reversal of the circulatory defect of the right basal ganglion in the third SPECT, is unknown. We assume that improvement of perfusion defect in right frontal and parietal region might be attributed to the rheological effect of ILIB, but the effect did not work in right putamen. The reason for that should be role of the redistribution of Cerebral Blood Flow (CBF), based on the fact that many studies of CBF assessment confirms that the flow redistribution does not jeopardize cerebral blood supply, and the redistribution of blood flow can cause particular vessels to undergo extra flow rate and hemodynamic stresses.
With respect to the redistribution in brain research, there have been many published articles in neuroscience. A study of the neuroprotective effects of vinpocetine, given intravenously in a 14-day regime, on the CBF in chronic ischemic stroke patients (n=13), Szilagyi et al., found that the vinpocetine can contribute effectively to the redistribution of CBF in the strokes, which effects are most pronounced in those brain regions with the highest uptake of the drug [22]. Another study regarding the staged endovascular embolization, a method for prevention of perioperative hemorrhagic complications during the management of brain AVMs, Orlov et al., found that simultaneous occlusion of more than 60% of AVM volume induces significant redistribution of local CBF [23].
In a study of therapeutic hypothermia and rewarming period in encephalopathic infants with long-term adverse neurological outcome, Montaldo et al., found that infants with hypoxic ischaemic encephalopathy who have adverse neurological outcome show a privileged CBF redistribution during the inervention [24]. Champagne et al., confirmed that redistribution of CBF across different brain regions, arising from the vasoactive nature of hypercapnia, can introduce errors when examining cerebrovascular reactivity response delays, and that combination of hypercapnic and hyperoxic delays can highlight CBF redistribution [25].
With respect to the redistribution in diabetic control, we reported an ischemic stroke patient with Complex Regional Pain Syndrome (CRPS), whose symptoms developed in coincidence with a corresponding rise of the contralateral thalamic CBF when the glycosylated hemoglobin values were high, twice seen as migration from the bottom to the top position of the thalamus. We concluded that poor glucose control cause redistribution of thalamic CBF and is associated with the persistence of CRPS [26]. Wiegers et al., confirmed that hypoglycemia may cause a redistribution of CBF towards the thalamus of both patients with normal awareness of hypoglycemia and healthy controls, consistent with activation of brain regions associated with the autonomic response to hypoglycemia [27].
We believe that redistribution might explain the change of blood flow of right striatum in our case. We need more studies to investigate the relationship of brain perfusion and cognitive function in the future.
In our case, initial symptoms were global aphasia, dysphagia, numbness and weakness of right limbs and unsteady gait. Limited improvement of his speech, comprehension, and limbs movement after 1 month of intensive physical therapy, occupational therapy and speech therapy, before ILIB was introduced. Brain SPECT showed hypoperfusion of left hemisphere, left striatum, left thalamus was found, which was compatible for his clinical symptoms. After three courses of ILIB, he can obey order and limbs movement as well as dysphagia improved gradually. Muscle power of left limbs improved from MRC grading 1 to 3. The second brain SPECT showed an improvement of prior perfusion deficit at right frontal and parietal regions, although a new deficit at right putamen region took place.
After the second stage of administration, e.g. the another six courses of ILIB, our case present a dramatic change of cognitive function, such as perceptual-motor function, language, executive function, and social cognition, which was compatible with the findings of third SPECT, e.g. increased uptake in right striatum.
Cognitive function refers to multiple neuropsychological issues, including attention, memory, calculation, communication, perception, self-awareness, problem solving, thinking flexibility, personality, stress coping and even interpersonal relationship. The basal ganglion has been known as crucial elements in the circuits of movement, learning and cognitive function. The striatum, one of the structures of basal ganglion divided into ventral and dorsal subdivision, based on function and connections. The ventral striatum is associated with limbic system and has been thought as an important part of the circuitry for decision making and reward-related behavior; the dorsal striatum is composed of the caudate nucleus and the putamen. The striatum is the major input region of basal ganglion and receives its major input from the cortex, while the globus pallidus and substantia nigra are the major output regions. The input and output regions are connected via direct and indirect pathways that have reciprocal effects on the basal ganglia output pathway, which control motor function. Cortical loops integrating the cortex and the basal ganglia are now accepted to play an important role in regulating behavioral, emotional and cognitive functions [7,8]. Impairment of those areas, including degeneration or hypoperfusion [9,10], may cause dysfunction of cognitive function, motivational salience, certain motor or executive functions that result in some neurologic or psychiatric disorders such as Parkinsonism diseases, Huntington's disease, bipolar disorder or dementia [11,12]. An observational study found that patients with putaminal stroke impaired motor imaginary, which result them unable to follow the instructions [13]. The fact of initial decrease and later increase in the blood flow of striatum was strongly correlated with the series of clinical pictures of our patient.
In recent decades, ILIB has been thought to improve rheological properties of the blood, to improve microcirculation, and reducing the area of infarction. It was developed for the treatment of cardiovascular diseases originally, but many studies showed various effects on many organs and on the hematologic and immunologic system [14], for instance, such as diminishing tendency of aggregation of thrombocytes [15-17], improved oxygen supply and wound healing, normalization of the metabolism of hypoxic tissue, positive effect on anti-inflammation and immunologic activity by modulation of cytokines and immune system [18,19]. ILIB has benefits in diaschisis reversal, motor cortex dysfunction, and reduction of homocysteine in our published case reports [6,20,21]. Regarding the risks involved with ILIB therapy, patients with history of seizure attack and ICH in recent 6 months should be prohibited.
The reason why local perfusion of right basal ganglion impaired in the second Brain SPECT, compared with reversal of the circulatory defect of the right basal ganglion in the third SPECT, is unknown. We assume that improvement of perfusion defect in right frontal and parietal region might be attributed to the rheological effect of ILIB, but the effect did not work in right putamen. The reason for that should be role of the redistribution of Cerebral Blood Flow (CBF), based on the fact that many studies of CBF assessment confirms that the flow redistribution does not jeopardize cerebral blood supply, and the redistribution of blood flow can cause particular vessels to undergo extra flow rate and hemodynamic stresses.
With respect to the redistribution in brain research, there have been many published articles in neuroscience. A study of the neuroprotective effects of vinpocetine, given intravenously in a 14-day regime, on the CBF in chronic ischemic stroke patients (n=13), Szilagyi et al., found that the vinpocetine can contribute effectively to the redistribution of CBF in the strokes, which effects are most pronounced in those brain regions with the highest uptake of the drug [22]. Another study regarding the staged endovascular embolization, a method for prevention of perioperative hemorrhagic complications during the management of brain AVMs, Orlov et al., found that simultaneous occlusion of more than 60% of AVM volume induces significant redistribution of local CBF [23].
In a study of therapeutic hypothermia and rewarming period in encephalopathic infants with long-term adverse neurological outcome, Montaldo et al., found that infants with hypoxic ischaemic encephalopathy who have adverse neurological outcome show a privileged CBF redistribution during the inervention [24]. Champagne et al., confirmed that redistribution of CBF across different brain regions, arising from the vasoactive nature of hypercapnia, can introduce errors when examining cerebrovascular reactivity response delays, and that combination of hypercapnic and hyperoxic delays can highlight CBF redistribution [25].
With respect to the redistribution in diabetic control, we reported an ischemic stroke patient with Complex Regional Pain Syndrome (CRPS), whose symptoms developed in coincidence with a corresponding rise of the contralateral thalamic CBF when the glycosylated hemoglobin values were high, twice seen as migration from the bottom to the top position of the thalamus. We concluded that poor glucose control cause redistribution of thalamic CBF and is associated with the persistence of CRPS [26]. Wiegers et al., confirmed that hypoglycemia may cause a redistribution of CBF towards the thalamus of both patients with normal awareness of hypoglycemia and healthy controls, consistent with activation of brain regions associated with the autonomic response to hypoglycemia [27].
We believe that redistribution might explain the change of blood flow of right striatum in our case. We need more studies to investigate the relationship of brain perfusion and cognitive function in the future.
CONCLUSION
Based on the clinical pictures and our SPECT findings, we confirm that SPECT image is a very worthwhile tool in the field of scintigraphic rehabilitation for monitoring the neural recovery. ILIB is also a fabulous intervention to improve the circulation of ischemic brain and simultaneously enhance the neurological recovery, such as cognitive dysfunction.
REFERENCES
- Momenzadeh S, Abbasi M, Ebadifar A, Aryani M, Bayrami J, et al. (2015) The intravenous laser blood irradiation in chronic pain and fibromyalgia. J Lasers Med Sci 6: 6-9.
- Mountz JM (2007) Nuclear medicine in the rehabilitative treatment evaluation in stroke recovery. Role of diaschisis resolution and cerebral reorganization. Eura Medicophys 43: 221-239.
- Wu YT, Lai MH, Lu SC, Chang ST (2011) Beneficial response to gabapentin portraying with interval change of brain SPECT imaging in a case with failed back surgery syndrome. J Clin Pharm Ther 36: 525-528.
- Wei TS, Hsu CS, Lee YC, Chang ST (2017) Degeneration of paramedian nuclei in the thalamus induces Holmes tremor in a case of artery of Percheron infarction. Medicine (Baltimore) 96: 8633.
- Chang CC, Ku CH, Chang ST (2017) Postural asymmetry correlated with lateralization of cerebellar perfusion in persons with chronic stroke: A role of crossed cerebellar diaschisis in left side. Brain Inj 31: 90-97.
- Yang WH, Lin SP, Chang ST (2017) Case report: Rapid improvement of crossed cerebellar diaschisis after intravascular laser irradiation of blood in a case of stroke. Medicine (Baltimore) 96: 5646.
- Leisman G, Braun-Benjamin O, Melillo R (2014) Cognitive-motor interactions of the basal ganglia in development. Front syst neurosci 8: 16.
- Robertson BD, Hiebert NM, Seergobin KN, Owen AM, MacDonald PA (2015) Dorsal striatum mediates cognitive control, not cognitive effort per se, in decision-making: An event-related fMRI study. Neuroimage 114: 170-184.
- Duncombe J, Kitamura A, Hase Y, Ihara M, Kalaria RN, et al. (2017) Chronic cerebral hypoperfusion: a key mechanism leading to vascular cognitive impairment and dementia. Closing the translational gap between rodent models and human vascular cognitive impairment and dementia. Clin Sci (Lond). 131: 2451-2468.
- Jing Z, Shi C, Zhu L, Xiang Y, Chen P, et al. (2015) Chronic cerebral hypoperfusion induces vascular plasticity and hemodynamics but also neuronal degeneration and cognitive impairment. J Cereb Blood Flow Metab 35: 1249-1259.
- Kübler D, Schroll H, Buchert R, Kühn AA (2017) Cognitive performance correlates with the degree of dopaminergic degeneration in the associative part of the striatum in non-demented Parkinson’s patients. J Neural Transm (Vienna) 124: 1073-1081.
- Willing AE, Jiang L, Nowicki P, Poulos S, Milliken M, et al. (2002) Effects of middle cerebral artery occlusion on spontaneous activity and cognitive function in rats. Int J Neurosci 112: 503-516.
- Li CR (2000) Impairment of motor imagery in putamen lesions in humans. Neurosci Lett 287: 13-16.
- Dmitriev AE, Iudin VA, Arapov NA, Martynov VA (1989) [Effect of intravascular laser irradiation of the blood on blood cells in pancreatitis]. Klin Med (Mosk) 67: 108-110.
- Boev SS, Selivonenko VG (1997) [The impact of the intravenous He-Ne laser therapy on the antioxidant system in patient with stable exertion angina and postinfarct cardiosclerosis]. Klin Med (Mosk) 75: 30-33.
- Fedoseeva GE, Smol'ianinova NK, Karu TI, Zelenin AV (1987) [Changes in the structure of lymphocyte chromatin after irradiation with He-Ne-laser]. Radiobiologiia 27: 605-609.
- Smol'yaninova NK, Karu TI, Fedoseeva GE, Zelenin AV (1991) Effects of He-Ne laser irradiation on chromatin properties and synthesis of nucleic acids in human peripheral blood lymphocytes. Biomed Sci 2: 121-126.
- Dube A, Bansal H, Gupta PK (2003) Modulation of macrophage structure and function by low level He-Ne laser irradiation. Photochem Photobiol Sci 2: 851-855.
- Funk JO, Kruse A, Neustock P, Kirchner H, et al. (1993) Helium-neon laser irradiation induces effects on cytokine production at the protein and the mRNA level. Exp Dermatol 2: 75-83.
- Liu EY, Chang ST (2019) Benefits of intravascular laser irradiation of blood on motor and sensory recovery viewing from brain function images: portrait of a case with chronic Sjögren's syndrome, transverse myelitis, and Guillain-Barré syndrome. Biomed J Sci & Tech Res 14: 10738-10741.
- Chang JY, Liu CC, Liu IT, Chang ST (2019) Effects of intravascular laser irradiation of blood on cognitive function in a stroke survivor with hyperhomocysteinemia: dual recuperations in thalamus and serum homocysteine. Biomed J Sci & Tech Res 16: 11864-11868.
- Szilágyi G, Nagy Z, Balkay L, Boros I, Emri M, et al. (2005) Effects of vinpocetine on the redistribution of cerebral blood flow and glucose metabolism in chronic ischemic stroke patients: a PET study. J Neurol Sci 15: 229-230:275-284.
- Orlov K, Panarin V, Krivoshapkin A, Kislitsin D, Berestov V, et al. (2015) Assessment of periprocedural hemodynamic changes in arteriovenous malformation vessels by endovascular dual-sensor guidewire. Interv Neuroradiol 21: 101-107.
- Montaldo P, Cuccaro P, Caredda E, Pugliese U, De Vivo M, et al. (2018) Electrocardiographic and echocardiographic changes during therapeutic hypothermia in encephalopathic infants with long-term adverse outcome. Resuscitation. 130: 99-104.
- Champagne AA, Bhogal AA, Coverdale NS, Mark CI, Cook DJ (2019) A novel perspective to calibrate temporal delays in cerebrovascular reactivity using hypercapnic and hyperoxic respiratory challenges. Neuroimage. 187: 154-165.
- Hsu KC, Chang ST (2013) Correlation of thalamic blood flow redistribution with persistent complex regional pain syndrome in a stroke patient with poor diabetic control. J Diabetes Investig 4: 676-678.
- Wiegers EC, Becker KM, Rooijackers HM, von Samson-Himmelstjerna FC, Tack CJ, et al. (2017) Cerebral blood flow response to hypoglycemia is altered in patients with type 1 diabetes and impaired awareness of hypoglycemia. J Cereb Blood Flow Metab 37: 1994-2001.
Citation: Sung JH, Chang ST (2019) Reversal of Impaired Blood Flow of the Basal Ganglion from the Prior Focal Perfusion Defect in a Case of Ischemic Infarction: Observation during the Two Stages of Administration of Intravenous Laser Irradiation of Blood. J Med Stud Res 2: 011.
Copyright: © 2019 Shin-Tsu Chang, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
© 2026, Copyrights Herald Scholarly Open Access. All Rights Reserved!