
Review of the Literature and Surgeon’s Opinion: Pelvic Fractures in the Geriatric Population. To Fix or Not to Fix?
*Corresponding Author(s):
Kenneth W Graf JrDepartment Of Orthopaedic Surgery, Cooper University Hospital, 3 Cooper Plaza, Suite 408, Camden, NJ, 08103, United States
Email:Graf-Kenneth@CooperHealth.edu
Abstract
Pelvic fractures in the geriatric population are occurring with increasing frequency secondary to an aging population. These injuries most commonly occur via low energy traumatic mechanisms such as a fall from standing height. Historically, pelvic fractures resulting from low energy trauma in the geriatric population have been treated conservatively. Recent studies have demonstrated significant complication and poor survival rates for the geriatric pelvic fracture patients that are treated conservatively. One recent factor that has been identified as a cause of increased morbidity and mortality in the geriatric pelvic fracture population is the injury to the posterior pelvic ring. Initial evaluation of the geriatric pelvic fracture patient consists of obtaining an anteroposterior pelvic radiograph. This radiograph is critical in assessing pelvic symmetry, anterior pelvic ring injury, and sacroiliac joint alignment. For further evaluation, a CT scan with 2mm thin cuts and 3D reconstruction is the imaging modality of choice in these acute fractures. Physical examination should focus on clinical findings of pelvic instability. In the setting of a stable posterior pelvic ring, we will proceed with a trial of non-operative treatment. If the patient is failing to mobilize or is having increasing pain at 3days, then surgical intervention is considered at this time. Previously, our group demonstrated excellent results for patients that underwent percutaneous skeletal fixation of sacral fractures with 94.9% of independently functioning patients returning to independent living and 95.7% of patients regaining ambulation post-operatively. Our group is currently working on a prospective, randomized study of LC-1 geriatric pelvic fractures to critically evaluate if a more aggressive surgical approach will have a significant effect on the morbidities, mortalities, and cost of care associated with these common and challenging fractures.
Keywords
Elderly; Fracture; Fragility; Geriatric; Pelvis’ Sacral
Introduction
Pelvic fractures in the geriatric population are occurring with increasing frequency secondary to an aging population [1-5]. These injuries most commonly occur via low energy traumatic mechanisms such as a fall from standing height. They can also be encountered in the high-energy traumatic setting such as a motor vehicle crash. The most common fracture pattern observed in the elderly population is the Lateral Compression type 1 (LC-1) [6,7]. However, it is imperative to understand that pelvic fractures in the geriatric population are fundamentally different than those fractures observed in the younger population [8]. As a result of this, a comprehensive classification of fragility fractures of the pelvic ring has been devised to aid in the decision making process when treating patients with these types of injuries [9].
Historically, pelvic fractures resulting from low energy trauma in the geriatric population have been treated conservatively. Historical studies demonstrated reassuring functional outcomes, with many surviving patients returning to their pre-injury ambulatory and activity status one year after their initial injury. Currently, the aforementioned findings are thought to underestimate the morbidity and mortality associated with these injuries, specifically in the older geriatric population [6,7,10-12]. Recent studies have demonstrated the significant complication and poor long-term survival rates associated with conservative treatment of many geriatric pelvic fragility fractures. A prospective study comparing patients with pubic rami fractures to age-matched cohorts in the general population demonstrated significantly worse survival rates for the fracture patients [13]. The morbidity associated with pelvic fractures in the elderly population includes hemorrhage requiring angiography and transfusion, inability to return to pre-injury household functional status requiring transfer to nursing home, respiratory/urinary tract infections, decubitus ulcers, decreased quality of life, and death [6,8,11,14]. Consequently, the morbidity associated with geriatric pelvic fractures results in increased hospital Length of Stay (LOS), utilization of resources, and significant economic impact on healthcare [4]. Furthermore, the mortality rates in the geriatric pelvic fracture population range from 16.3% to 24.3% one-year post-injury [7,15-22], 30% two-years post-injury [23], 41% three-years post-injury [15], and 49% to 58.1% five-years post-injury [17,24].
One recent factor that has been identified as a cause of increased morbidity and mortality in the geriatric pelvic fracture population is the injury to the posterior pelvic ring. With the advent of CT scan, sacral fractures or crush injuries to the posterior pelvic ring in the setting of pubic rami fractures are being identified more frequently. These concomitant fractures are often associated with a clinically unstable pelvic ring [9]. Loggers et al., evaluated the outcomes of pubic rami fractures with or without concomitant posterior pelvic ring fracture and found that admission, complication, and hospital LOS rates were higher in patients with posterior pelvic ring disruption [19]. In light of the significant morbidity and mortality rates associated with these geriatric pelvic fractures, there has been an increase in literature investigating the outcomes associated with operative fixation of said injuries. We present to you a review of the current literature and current opinion of a high volume pelvis surgeon at a level one trauma center.
Surgeon’s Opinion
At our institution, the geriatric pelvic fracture patient is mainly encountered in the emergency department or trauma bay. On rare occasions, a geriatric pelvic fracture patient will be transferred from an outside hospital for escalation of care. Initial evaluation always includes an Anteroposterior (AP) pelvic radiograph. This radiograph is critical in assessing pelvic symmetry, anterior pelvic ring injury and sacroiliac joint alignment. The initial AP pelvis radiograph can, however, significantly underestimate the number of clinically unstable pelvic fractures and injuries in the geriatric patient population. In particular, posterior pelvic injuries are difficult to assess on plain radiographs as the bowel and tissue infront of the sacrum obscures osseous details. Figure 1 demonstrates an AP pelvis radiograph depicting an obscured posterior pelvic ring secondary to bowel gas and abdominal tissues. Moreover, the poor bone density found in patients with fragility fractures of the pelvis further adds to the challenge of properly evaluating the posterior pelvic ring. For these reasons, a CT scan with 2mm thin cuts and three-dimensional reconstruction is the imaging modality of choice in these acute fractures. Figures 2 and 3 demonstrate a 2mm cut coronal CT scan of the same pelvis demonstrating bilateral superior pubic rami fractures and a right-sided sacral fracture that were obscured on AP pelvic radiography.
 Figure 1: AP pelvis radiograph of a patient with bilateral superior pubic rami fractures and a right-sided sacral fracture obscured by bowel, abdominal gas, and soft tissue.
Figure 1: AP pelvis radiograph of a patient with bilateral superior pubic rami fractures and a right-sided sacral fracture obscured by bowel, abdominal gas, and soft tissue.
 Figure 2: 2mm coronal cut CT scan of the pelvis demonstrating bilateral superior pubic rami fractures previously obscured on radiograph.
Figure 2: 2mm coronal cut CT scan of the pelvis demonstrating bilateral superior pubic rami fractures previously obscured on radiograph.
 Figure 3: 2mm coronal cut CT scan of the pelvis demonstrating a right-sided sacral fracture previously obscured on radiograph.
Figure 3: 2mm coronal cut CT scan of the pelvis demonstrating a right-sided sacral fracture previously obscured on radiograph.
Physical examination should focus on clinical findings of pelvic instability. Assessment of pelvic instability on physical exam consists of gentle internal and external compression via the iliac wings. This testing is not to be vigorous on the geriatric population as it could result in vascular injury. The internal and external pelvic compression test is only to be performed once as the risks of performing the test more than once outweigh the benefits. Evaluation of leg positioning can help assist in determining the degree of rotational and vertical instability. Close attention is to be paid to sacral tenderness on palpation or compression.
In the setting of an intact posterior pelvic ring, we will proceed with a trial of non-operative treatment. The trial of non-operative treatment is initiated by obtaining a five view radiographic assessment of the pelvis consisting of an AP, inlet, outlet, obturator oblique, and iliac oblique views prior to having the patient mobilize. Once this has been obtained, we have the primary team implement an aggressive pain management protocol on the first day of admission. We have the patient begin weight-bearing trials with physiotherapists as soon as possible. This usually consists of having the patient get out of bed and stand at the bedside. The goal is to have the patient progress to walking with or without assistance by hospital day 3. We monitor the patient’s progress and speak to the physiotherapists on a daily basis. If the patient is failing to mobilize or is having increasing pain at 3 days, then surgical intervention is considered at this time. In our experience, the majority of patients with isolated anterior pelvic ring injuries who have difficulty mobilizing within the allotted time frame have sustained superior pubic root or low anterior column acetabular injuries.
Surgical intervention for pubic rami fractures consists of minimally invasive, percutaneous skeletal fixation via fluoroscopic guidance. Rarely, a geriatric patient may undergo open reduction and internal fixation with plate and screws. Percutaneous screw fixation can be performed in antegrade or retrograde fashion depending on the location of the fracture. Höch et al., demonstrated a 21% survival advantage at two-year follow-up for surgically treated patients when compared to patients that were treated in conservative fashion [23]. Winkelhagen et al., evaluated patients who underwent percutaneous screw fixation for isolated pubic ramus fractures and found that 50% of patients were pain free while the other 50% had reduced pain, 67% of patients regained mobility to pre-injury status while 33% demonstrated improvement in post-operative mobility, and nearly 70% of surgically treated patients were discharged to their original domicile [22]. Schmitz et al., found a 4% decrease in inpatient mortality rate and a 12% increase in survival rate at two-year follow-up in patients with pubic rami fractures that were treated surgically [8].
In the setting of an unstable pelvis with anterior and posterior pelvic ring disruption, we will recommend operative fixation of the injuries with percutaneous skeletal fixation. The most common LC-1 injury requiring surgical intervention is a complete sacral fracture (typically seen on CT scan) associated with superior and inferior pubic rami fractures. The anterior pelvic ring will be most commonly be addressed via antegrade/retrograde percutaneous screw fixation. The posterior pelvic ring is typically addressed via percutaneous iliosacral screw fixation or transiliac transsacral screw fixation. In the setting of sacroiliac joint diastasis, iliosacral screw fixation is preferred to be able to reduce the joint diastasis. In the setting of a sacral fracture, transiliac transsacral screw fixation is typically utilized for fracture stabilization when pelvic morphology allows. The increased screw length obtained with transiliac transsacral screw fixation provides improved stability in osteoporotic bone. Studies have demonstrated that operative fixation allows for immediate ambulation and high rates of return to independent living [25-27]. Furthermore, our group demonstrated excellent results for patients that underwent percutaneous skeletal fixation of sacral fractures with 94.9% of independently functioning patients returning to living independently and 95. 7% of patients regaining ambulation post-operatively [28]. Figure 4 demonstrates a post-operative AP pelvis radiograph of a patient who sustained a right-sided LC-1 pelvic fracture with an associated left superior pubic ramus fracture. The patient was having difficulty mobilizing, in addition to uncontrollable pain, and underwent percutaneous fixation of her injuries via antegrade, retrograde, and S1/S2 transiliac transsacral screw fixation. Notice antegrade anterior column screw fixation on the right and retrograde anterior column screw fixation on the left to stabilize the anterior pelvic ring. S1/S2 transiliac transsacral screw fixation was utilized to stabilize the posterior pelvic ring. The patient was mobilizing the subsequent day with very minimal pain.
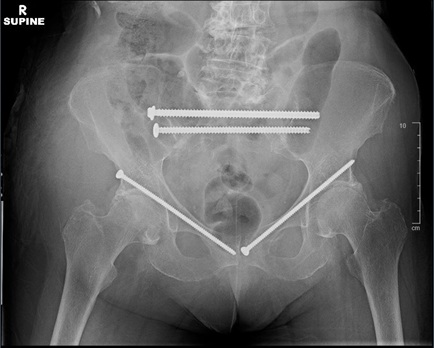 Figure 4: Post-operative AP pelvis radiograph demonstrating percutaneous fixation of bilateral superior pubic rami fractures and a right-sided complete sacral fracture. Notice antegrade anterior column screw fixation on the right and retrograde anterior column screw fixation on the left to stabilize the anterior pelvic ring. S1/S2 transiliac transsacral screw fixation was utilized to stabilize the posterior pelvic ring.
Figure 4: Post-operative AP pelvis radiograph demonstrating percutaneous fixation of bilateral superior pubic rami fractures and a right-sided complete sacral fracture. Notice antegrade anterior column screw fixation on the right and retrograde anterior column screw fixation on the left to stabilize the anterior pelvic ring. S1/S2 transiliac transsacral screw fixation was utilized to stabilize the posterior pelvic ring.
In our experience, a patient with a clinically stable pelvic fragility fracture will be able to mobilize within three days when a satisfactory analgesic protocol is utilized. Patients with clinically unstable pelvic fragility fractures are unable to mobilize within three days even with adequate analgesia. Examination under anesthesia will commonly demonstrate a grossly unstable pelvis. This results in prolonged bed rest, increased narcotic use, and rapid deconditioning. These subsets of patients are the ones that can most benefit from percutaneous pelvic fixation and immediate weight bearing.
When operative intervention is chosen, anesthesia insults should be minimized. Spinal anesthesia or local analgesia in conjunction with monitored anesthesia is preferred. The morbidity of the surgery is minimal in comparison to the complications that may arise secondary to prolonged immobilization. The surgery is minimally invasive and is performed through a small incision. Both surgical times and blood loss are minimal and the benefits of mobilization are immediately observable. Geriatric patients who have sustained pelvic fragility fractures and have undergone percutaneous stabilization have demonstrated a high rate of return to pre-injury ambulation and residential living status. These patients also have decreased LOS and narcotic use translating to less of an economic impact to the healthcare system. The vast majority of patients in this scenario are pain free and able to mobilize immediately after surgery with limited to no narcotic utilization.
Discussion
It is understood that a large portion of Isolated Anterior Pelvic Ring (iAPR) injuries in the geriatric population can be treated conservatively with multimodal pain control, early weight bearing, and physical therapy. Historically, this has been the treatment of choice for these injuries as iAPR injuries were thought to have limited impact on patient outcomes. However, it has been demonstrated that iAPR fractures can be extremely detrimental to the elderly resulting in immobilization, loss of autonomy, and increased mortality [21]. Achieving adequate analgesia in the geriatric patient with a pelvic fracture is vital. In order to accomplish this, the treating physician must overcome several barriers and exhibit careful supervision [29].
Elderly patients are more susceptible to the effects of narcotic medication. Furthermore, treatment of the cognitively impaired geriatric patient with opioid derivatives may result in oversedation resulting in more time spent in bed and less time spent working with physical therapy. In contrast, it is possible that the geriatric patient sustaining a pelvis fracture is undertreated from an analgesic standpoint secondary to fear of oversedation, resulting in an inability to mobilize and progress with physical therapy. Both of these scenarios may translate to an increase in hospital LOS, discharge to rehab facility as opposed to home, and an increased economic burden on the healthcare system. Therefore, an analgesic homeostasis must be achieved to avoid oversedation but allow for satisfactory pain control. We recommend standing acetaminophen for the patient that does not suffer from hepatic disease and a gabapentin or cyclobenzaprine as needed. Fluid resuscitation is also imperative in these patients as loss of volume is inevitable despite the low energy nature of these injuries. Henry et al., documented an increased rate of transfusion in the elderly patient who suffered a pelvic fracture and increased rate of angiographic embolization secondary to blood loss [6]. The authors hypothesized that a combination of atherosclerotic disease diminishing vessel vasospasm and lack of turgor in the skin and soft tissues resulted in increased, uncontrollable bleeding in the pelvis and retroperitoneum. O’Brien et al., also demonstrated a higher transfusion rate during the first 72 hours after injury in the geriatric population that suffered a pelvic fracture [30]. To provide the best treatment possible to the geriatric pelvic fracture population, the inciting event must be investigated thoroughly. In the setting of a low energy traumatic mechanism such as a fall from standing height, the reason for the fall must be identified via a multi-disciplinary approach. The patient may benefit from a geriatrician consultation and home medication reconciliation with the primary focus being to eliminate medications with sedative effects and identifying medications that may interact with one another resulting in unwanted secondary effects. If possible, surveillance of the home for potential fall risks and fall prevention education should be provided to the patient. If a trauma surgeon is managing the patient, internal medicine and/or cardiology consultation may be warranted. Atherosclerotic disease is common in the elderly population and acute cardiac dysfunction or ischemia may result secondary to decreases in circulatory blood volume. It is important to identify this prior to noticing a decrease in hemoglobin/hematocrit, hypotension, or tachycardia as cardiac dysfunction may result in a hypoperfusion injury from which the geriatric patient may not be able to recover. In light of this, more liberal transfusion and embolization protocols should be considered in the geriatric pelvic fracture population [6]. An overall orthogeriatric approach, similar to that used in the geriatric hip fracture population, should be implemented to avoid the common complications, such as respiratory/urinary tract infections, delirium, and pressure ulcers, observed in this patient population [31].
The role of the orthopaedic surgeon is not to be downplayed in the work up and management of the geriatric pelvic fracture. In our experience, the orthopaedic traumatologist is often the physician that is first consulted to see the geriatric pelvic fracture patient. It is the orthopaedic surgeon’s duty to identify this fracture as a fragility fracture and initiate the work up and management for osteoporosis [32]. Diagnostic work up should include obtaining baseline vitamin D, calcium, parathyroid hormone, and thyroid-stimulating hormone values. Medical treatment should be considered with the drug of choice being a bisphosphonate. Parathyroid hormone agonists have demonstrated encouraging results in consolidation of pelvic fragility fractures [33,34]. Vitamin D and calcium supplementation should be initiated as appropriate. Other aspects of management include lifestyle changes and fall prevention education. Lifestyle changes should include increase in weight bearing activities if the patient is able to tolerate. It is of utmost importance for the primary physician to ensure adequate follow up as low rates of follow-up for osteoporosis diagnostics after fragility fractures have been demonstrated in the past [35]. At our institution we implement the “Own the Bone” program, a national post-fracture, systems-based, multidisciplinary fragility fracture prevention initiative.
Besides identifying the nature of the fracture, initiating the diagnostic work up, and implementing medical management, the treating physician must identify whether or not the pelvic fracture is deemed stable or unstable. If the injury is determined to be stable, then conservative management may be pursued. Rommens et al., recommends initial bed rest for a few days up to 1 week with aggressive analgesia prior to beginning the weight bearing as tolerated rehabilitation protocol [36]. These authors recommended against forced mobilization prior to radiographic fracture consolidation referencing premature and aggressive mobilization as a risk factor for further fracture displacement and increased instability [9]. In contrast, we opt for aggressive pain control measures and mobilization as tolerated immediately after injury understanding that the patients will limit themselves based on the severity of the injury. This allows us to discern what patients would benefit from surgery in an earlier timeframe.
Disruption of the anterior pelvic ring is frequently associated with posterior pelvic ring fractures. This concept of anterior pelvic ring disruption having significant association with posterior pelvic ring disruption was initially introduced by Pennal et al., in 1980. The authors reported that pelvic ring disruption at one location often results in dissociation at another location [37]. Lau et al., evaluated patients for occult posterior pelvic ring fractures in the setting of pubic rami fractures and found that 59% of their cohort had posterior pelvic ring injuries [18]. Rommens et al., found that pubic rami fractures with posterior pelvic ring injuries make up 80% of fragility fractures of the pelvis [38].
Oftentimes, posterior pelvic ring fractures are difficult to detect on plain radiographic imaging secondary to overlying bowel gas, contrast fluid in the bladder, osteoporotic bone, and spontaneous reposition of fracture fragments. However, there are certain indicators that can be observed on plain radiographic imaging that may be suggestive of posterior pelvic ring fractures. Courtney et al., evaluated the association of inferior pubic rami fractures and posterior pelvic ring injuries. The authors found that 68% of inferior pubic rami fractures had concomitant posterior pelvic ring fractures and deemed 60% of these injuries to be unstable [39]. They also observed that combined superior/inferior pubic rami fractures, isolated parasymphyseal inferior pubic ramus fracture, and bilateral inferior pubic rami fractures were all significantly associated with posterior pelvic ring injuries and instability. The authors concluded that inferior pubic rami fractures serve as a marker for posterior pelvic ring instability. Furthermore, Lim et al., found that 75% of patients with pubic rami fractures had an associated posterior pelvic ring fracture. The authors also found that 96% of parasymphyseal pubic rami fractures and 84% of combined superior/inferior pubic rami fractures had a concomitant posterior pelvic ring fracture. They also observed that pubic rami fractures with more than 4.6mm of displacement were significantly associated with posterior pelvic ring injury. Lastly, 100% of patients in this study with isolated inferior pubic rami fractures also had a posterior pelvic ring fracture [40]. Therefore, identification of these fracture patterns on plain radiographic imaging warrants a detailed physical exam with focus on the posterior pelvis, advanced imaging consisting of CT scan, and possible evaluation under anesthesia.
The consequences of a missed posterior pelvic ring fracture can be devastating, resulting in chronic pain, malunion, instability, functional impairment and prolonged rehab [18,39]. Consequently, it is imperative to scrutinize the posterior pelvic ring. On physical examination, the presence of sacral pain and tenderness in patients with anterior pelvic ring injuries is highly suggestive of a posterior pelvic ring fracture [41]. The use of advanced imaging has also aided in identifying injuries to the posterior pelvic ring. Cosker et al., utilized MRI to help identify sacral fractures in the setting of pubic rami fractures and found that 90% of the patients had sacral fractures [42]. Scheyerer et al., evaluated 177 patients with pubic rami fractures and found that 96.8% of patients had injuries to the posterior pelvic ring on CT scan [43]. The authors suggested that high rate of detection of fractures of the posterior pelvic ring was secondary to the use of 1.6mm thin slice cuts on the CT scan of the pelvis.
Disruption of the anterior and posterior pelvic ring can result in an inherently unstable pelvis. When a pelvic injury is deemed to be unstable, the orthopaedic trauma surgeon should begin to consider operative treatment in these patients. In recent years, there has been a trend towards increased operative fixation of unstable geriatric pelvic fractures [9,23,25-27,44-46]. Rommens et al., recommended surgical fixation of unstable pelvic fractures in the geriatric population in his treatment algorithm [47]. The decision to operate on the geriatric pelvic fracture is based on several factors including pelvic instability, inability to adequately mobilize, pain control, quality of life, and prevention of complications associated with immobilization. The decision to proceed with operative fixation should be made relatively quickly because the risks of complications increase as each day elapses [48,49]. Fritz et al., demonstrated that there was a 10% increased daily risk for development of pressure ulcers in geriatric patients with pelvic fractures [50]. Similar findings have also been reported in the hip fracture literature [51]. Furthermore, Loggers et al., found that the strongest predictor for one-year mortality for geriatric patients admitted with pelvic fractures was inpatient complications [19]. The authors also found that 100% of patients that lived independently prior to their injury and developed inpatient complications were discharged to an institution as opposed to returning to their original domicile.
Overall, our experience demonstrates that stable geriatric pelvic fractures should be treated conservatively whenever possible. However, the threshold to pursue operative treatment should be relatively low if the patient has uncontrolled pain or is failing to mobilize within three days after the injury. The aforementioned can be a sign of a clinically unstable pelvis or a patient with a stable injury that may not tolerate conservative treatment. In this scenario, percutaneous screw fixation to stabilize the anterior and/or posterior ring should be highly considered as the literature is demonstrating excellent results that include early weight bearing, return to pre-injury ambulatory status, decreased LOS and decreased inpatient complications.
Conclusion
Low energy pelvic fractures in the geriatric population have traditionally been treated conservatively with little follow-up. Prolonged immobilization of these patients can lead to a loss of self-sufficiency, an increase in complications, and an overall increase in cost of care. Caring for geriatric pelvic fracture patients that were previously ambulatory requires high vigilance. Patients with a clinically stable pelvic fragility fracture are able to mobilize within three days when adequate analgesia is provided. Patients with a clinically unstable pelvic fragility fracture are unable to mobilize within three days. Operative fixation should be considered for this subset of patients. When operative fixation is chosen, anesthesia risks should be minimized. Spinal anesthesia or local analgesia in conjunction with monitored anesthesia care is preferred.
Timely fixation of geriatric hip fractures has definitively improved outcomes for these patients. Pelvic fragility fractures in the geriatric population have similar complication, morbidity, and mortality profiles as the geriatric hip fracture population. Our group is currently working on a prospective, randomized study of LC-1 geriatric pelvic fractures. This study is necessary to critically evaluate if a more aggressive surgical approach will have a significant effect on the morbidities, mortalities, and cost of care associated with these common and challenging fractures.
References
- Boufous S, Finch C, Lord S, Close J (2005) The increasing burden of pelvic fractures in older people, New South Wales, Australia. Injury 36: 1323-1329.
- Dodge G, Brison R (2010) Low-impact pelvic fractures in the emergency department. CJEM 12: 509-513.
- Holstein JH, Culemann U, Pohlemann T, Working Group Mortality in Pelvic Fracture Patients (2012) What are predictors of mortality in patients with pelvic fractures? Clin Orthop Relat Res 470: 2090-2097.
- Kannus P, Palvanen M, Niemi S, Parkkari J, Järvinen M (2000) Epidemiology of osteoporotic pelvic fractures in elderly people in Finland: sharp increase in 1970-1997 and alarming projections for the new millennium. Osteoporos Int 11: 443-448.
- Nanninga GL, de Leur K, Panneman MJ, van der Elst M, Hartholt KA (2014) Increasing rates of pelvic fractures among older adults: The Netherlands, 1986-2011. Age Ageing 43: 648-653.
- Henry SM, Pollak AN, Jones AL, Boswell S, Scalea TM (2002) Pelvic fracture in geriatric patients: A distinct clinical entity. J Trauma 53: 15-20.
- Ting B, Zurakowski D, Herder L, Wagner K, Appleton P, et al. (2014) Preinjury ambulatory status is associated with 1-year mortality following lateral compression Type I fractures in the geriatric population older than 80 years. J Trauma Acute Care Surg 76: 1306-1309.
- Schmitz P, Lüdeck S, Baumann F, Kretschmer R, Nerlich M, et al. (2019) Patient-related quality of life after pelvic ring fractures in elderly. Int Orthop 43: 261-267.
- Rommens PM, Hofmann A (2013) Comprehensive classification of fragility fractures of the pelvic ring: Recommendations for surgical treatment. Injury 44: 1733-1744.
- Ayoung-Chee P, McIntyre L, Ebel BE, Mack CD, McCormick W, et al. (2014) Long-term outcomes of ground-level falls in the elderly. J Trauma Acute Care Surg 76: 498-503.
- van Dijk WA, Poeze M, van Helden SH, Brink PR, Verbruggen JP (2010) Ten-year mortality among hospitalised patients with fractures of the pubic rami. Injury 41: 411-414.
- Verbeek DO, Ponsen KJ, Fiocco M, Amodio S, Leenen LPH, et al. (2018) Pelvic fractures in the Netherlands: epidemiology, characteristics and risk factors for in-hospital mortality in the older and younger population. Eur J Orthop Surg Traumatol 28: 197-205.
- Hill RM, Robinson CM, Keating JF (2001) Fractures of the pubic rami. Epidemiology and five-year survival. J Bone Joint Surg Br 83: 1141-1144.
- Soles GL, Ferguson TA (2012) Fragility fractures of the pelvis. Curr Rev Musculoskelet Med 5: 222-228.
- Banierink H, Ten Duis K, de Vries R, Wendt K, Heineman E, et al. (2019) Pelvic ring injury in the elderly: Fragile patients with substantial mortality rates and long-term physical impairment. PloS one 14: 0216809.
- Clement ND, Court-Brown CM (2014) Elderly pelvic fractures: the incidence is increasing and patient demographics can be used to predict the outcome. Eur J Orthop Surg Traumatol 24: 1431-1437.
- Hamilton CB, Harnett JD, Stone NC, Furey AJ (2019) Morbidity and mortality following pelvic ramus fractures in an older Atlantic Canadian cohort. Can J Surg 62: 270-274.
- Lau TW, Leung F (2010) Occult posterior pelvic ring fractures in elderly patients with osteoporotic pubic rami fractures. J Orthop Surg (Hong Kong) 18: 153-157.
- Loggers SAI, Joosse P, Jan Ponsen K (2019) Outcome of pubic rami fractures with or without concomitant involvement of the posterior ring in elderly patients. Eur J Trauma Emerg Surg 45: 1021-1029.
- Reito A, Kuoppala M, Pajulammi H, Hokkinen L, Kyrölä K, et al. (2019) Mortality and comorbidity after non-operatively managed, low-energy pelvic fracture in patients over age 70: A comparison with an age-matched femoral neck fracture cohort and general population. BMC Geriatr 19: 315.
- Rommens PM, Hopf JC, Herteleer M, Hofmann A, Wagner D (2000) isolated pubic ramus fractures are serious adverse events for elderly persons: An observational study on 138 patients with fragility fractures of the pelvis Type I (FFP Type I). J Clin Med.
- Winkelhagen J, van den Bekerom MP, Bolhuis HW, Hogervorst M (2012) Preliminary results of cannulated screw fixation for isolated pubic ramus fractures. Strategies in trauma and limb reconstruction 7: 87-91.
- Höch A, Özkurtul O, Pieroh P, Josten C, Böhme JJ (2017) Outcome and 2-year survival rate in elderly patients with lateral compression fractures of the pelvis. Geriatr Orthop Surg Rehabil 8: 3-9.
- Spencer JD, Lalanadham T (1985) The mortality of patients with minor fractures of the pelvis. Injury 16: 321-323.
- Eckardt H, Egger A, Hasler RM, Zech CJ, Vach W, et al. (2017) Good functional outcome in patients suffering fragility fractures of the pelvis treated with percutaneous screw stabilisation: Assessment of complications and factors influencing failure. Injury 48: 2717-2723.
- Pulley BR, Cotman SB, Fowler TT (2018) Surgical fixation of geriatric sacral u-type insufficiency fractures: A retrospective analysis. Journal of orthopaedic trauma 32: 617-622.
- Walker JB, Mitchell SM, Karr SD, Lowe JA, Jones CB, et al. (2018) Percutaneous transiliac-transsacral screw fixation of sacral fragility fractures improves pain, ambulation, and rate of disposition to home. Journal of orthopaedic trauma 32: 452-456.
- Ferry C, Kim V, Ostrander J, Gaughan J, Mashru, RP, et al. (2020) Surgical fixation of sacral fractures in the elderly population: Are there predictors of outcome? An analysis of return to ambulation and residential living status. Geriatric orthopaedic surgery & rehabilitation 11: 1-9.
- van Berkel D, Ong T, Drummond A, Hendrick P, Leighton P, et al. (2019) ASSERT (Acute Sacral inSufficiEncy fractuRe augmenTation) randomised controlled, feasibility in older people trial: A study protocol. BMJ open.
- O'Brien D P, Luchette FA, Pereira SJ, Lim E, Seeskin CS, et al. (2002) Pelvic fracture in the elderly is associated with increased mortality. Surgery 132: 710-714.
- Mears SC, Berry DJ (2011) Outcomes of displaced and nondisplaced pelvic and sacral fractures in elderly adults. J Am Geriatr Soc59: 1309-1312.
- Dell R, Greene D, Schelkun SR, Schelkun SR, Williams K (2008) Osteoporosis disease management: the role of the orthopaedic surgeon. J Bone Joint Surg Am 90:188-194.
- Bukata SV (2011) Systemic administration of pharmacological agents and bone repair: what can we expect. Injury 42: 605-608.
- Wu CC, Wei JC, Hsieh CP, Yu CT (2012) Enhanced healing of sacral and pubic insufficiency fractures by teriparatide. J Rheumatol 39: 1306-1307.
- Freedman KB, Kaplan FS, Bilker WB, Strom BL, Lowe RA (2000) Treatment of osteoporosis: are physicians missing an opportunity? J Bone Joint Surg Am 82: 1063-1070.
- Rommens PM, Wagner D, Hofmann A (2012) Surgical management of osteoporotic pelvic fractures: A new challenge. Eur J Trauma Emerg Surg 38:499-509.
- Pennal GF, Tile M, Waddell JP, Garside H (1980) Pelvic disruption: assessment and classification. Clin Orthop Relat Res.
- Rommens P, Wissing H, Serdarevic M (1987) [Significance of computerized tomography in the diagnosis and therapy of fractures of the posterior pelvic ring and hip joint]. Unfallchirurgie 13: 32-37.
- Courtney PM, Taylor R, Scolaro J, Donegan D, Mehta S (2014) Displaced inferior ramus fractures as a marker of posterior pelvic injury. Arch Orthop Trauma Surg 134: 935-939.
- Lim EJ, Kim JJ, Kim JW, Kim KH (2020) What characteristics indicate concomitant posterior pelvic injury in pubic ramus fractures in the elderly? Orthop Traumatol Surg Res 106: 849-853.
- Alnaib M, Waters S, Shanshal Y, Caplan S, Jones S, et al. (2012) Combined pubic rami and sacral osteoporotic fractures: A prospective study. J Orthop Traumatol 13: 97-103.
- Cosker TD, Ghandour A, Gupta SK, Tayton KJJ (2005) Pelvic ramus fractures in the elderly: 50 patients studied with MRI. Acta Orthop 76: 513-516.
- Scheyerer MJ, Osterhoff G, Wehrle S, Wanner GA, Simmen HP, et al. (2012) Detection of posterior pelvic injuries in fractures of the pubic rami. Injury 43: 1326-1329.
- Beckmann JT, Presson AP, Curtis SH, Haller JM, Stuart AR, et al. (2014) Operative agreement on lateral compression-1 pelvis fractures. A survey of 111 OTA members. Journal of orthopaedic trauma 28:681-685.
- Böhme J, Höch A, Josten C (2012) [Osteoporotic fractures of the pelvis]. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen 83: 875-881.
- Bruce B, Reilly M, Sims S. OTA (2011) OTA highlight paper predicting future displacement of nonoperatively managed lateral compression sacral fractures: Can it be done? Journal of orthopaedic trauma 25: 523-527.
- Rommens PM, Ossendorf C, Pairon P, Dietz SD, Wagner D, et al. (2015) Clinical pathways for fragility fractures of the pelvic ring: personal experience and review of the literature. J Orthop Sci 20: 1-11.
- Dittmer DK, Teasell R (1993) Complications of immobilization and bed rest. Part 1: Musculoskeletal and cardiovascular complications. Can Fam Physician 39: 1428-1432.
- Teasell R, Dittmer DK (1993) Complications of immobilization and bed rest. Part 2: Other complications. Can Fam Physician 39:1440-1442.
- Fritz A, Gericke L, Höch A, Josten C, Osterhoff G (2020) Time-to-treatment is a risk factor for the development of pressure ulcers in elderly patients with fractures of the pelvis and acetabulum. Injury 51: 352-356.
- Hommel A, Ulander K, Thorngren KG (2003) Improvements in pain relief, handling time and pressure ulcers through internal audits of hip fracture patients. Scandinavian journal of caring sciences 17:78-83.
Citation: Rodriguez JA Jr, Shahi A, Mashru RP, Graf KW Jr (2021) Review of the Literature and Surgeon’s Opinion: Pelvic Fractures in the Geriatric Population. To Fix or Not to Fix? J Gerontol Geriatr Med 7: 089.
Copyright: © 2021 Julio A Rodriguez Jr, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

