
Journal of Physical Medicine Rehabilitation & Disabilities Category: Medical
Type: Case Report
Rheumatoid Arthritis Concomitant with Brucellosis: Case Report in Addition to Clinical and Rehabilitation Outcomes
*Corresponding Author(s):
Tarek M El-goharyDepartment Of Physical Therapy, College Of Medical Rehabilitation Sciences, Taibah University, Saudi Arabia
Tel:+966-0545007025,
Email:dr.elgoharyt@yahoo.com
Received Date: Jan 11, 2019
Accepted Date: Feb 12, 2019
Published Date: Feb 26, 2019
Abstract
Introduction
Symptoms control and physical capacity are fundamentals in patients with Rheumatoid Arthritis, but when concomitant with Brucellosis it becomes another challenge. Case Report: A 48- year old Saudi male patient presented with bilateral swollen knees and ankles, bilateral adductors’ tendinitis, and left shoulder tendinitis, generalized body ache in addition to physical functional decline. The patient was diagnosed with Rheumatoid arthritis 40 months ago and since then he has been on medications. The patient was also diagnosed with brucellosis five months ago and was on medications but he has been suffering from exacerbation of many symptoms since. The patient was slowly but steadily responding to physical therapy interventions but since he had developed Brucellosis, controlling symptoms become more difficult and necessitates ongoing physical therapy management and follow up with the designated medical doctors.
Conclusion
It is not uncommon to have a flare up of the current Rheumatoid arthritis in addition to acquiring Brucellosis especially in the endemic areas; therefore physical therapists and rehabilitation clinicians should consider presence of more than one disease which needs thorough evaluation and prudent rehabilitation program.
Symptoms control and physical capacity are fundamentals in patients with Rheumatoid Arthritis, but when concomitant with Brucellosis it becomes another challenge. Case Report: A 48- year old Saudi male patient presented with bilateral swollen knees and ankles, bilateral adductors’ tendinitis, and left shoulder tendinitis, generalized body ache in addition to physical functional decline. The patient was diagnosed with Rheumatoid arthritis 40 months ago and since then he has been on medications. The patient was also diagnosed with brucellosis five months ago and was on medications but he has been suffering from exacerbation of many symptoms since. The patient was slowly but steadily responding to physical therapy interventions but since he had developed Brucellosis, controlling symptoms become more difficult and necessitates ongoing physical therapy management and follow up with the designated medical doctors.
Conclusion
It is not uncommon to have a flare up of the current Rheumatoid arthritis in addition to acquiring Brucellosis especially in the endemic areas; therefore physical therapists and rehabilitation clinicians should consider presence of more than one disease which needs thorough evaluation and prudent rehabilitation program.
Keywords
Brucellosis; Clinical outcome; Knee swelling; Rheumatoid arthritis; Tendinitis
INTRODUCTION
Rheumatoid Arthritis (RA) is very common to result in persistent joint inflammation, synovitis, tendinitis, general body ache and functional decline [1]. Patients with RA must be carefully monitored as they experience cycles of remission and relapse that necessitate close medical supervision to adjust medications accordingly [2]. RA needs multidisciplinary management by team of professionals [3]. The medical doctor has to control symptoms using medications and the physical therapists control symptoms and improve functional capacity using rehabilitation measures.While the patient is under physical rehabilitation, it is not uncommon to suffer a relapse but the clinical pictures are more likely to confuse clinicians between being a flare up of the RA itself andbeing a new disease [2]. Clinicians should be aware of the possibility of Brucellosis in endemic areas among patients with a known diagnosis of RA [4]. To the best of my knowledge, there is no previously published case report describing clinical presentation and clinical progression during physical therapy rehabilitation. The present report describes a rare case presenting in a male patient formerly diagnosed with Rheumatoid Arthritis and who developed flare up of symptoms along with muscular and osteoarticular complications due to Brucellosis. The patient was referred out by the medical doctor for physical therapy and rehabilitation.
CASE REPORT
A 48- year old Saudi male patient with a 40 months history of Rheumatoid Arthritis (RA) presented with a 2 week history of generalized body ache, deconditioning, worsening left knee stiffness along with heat and swelling. The patient was under physical therapy and medical care. He complained of fever, fatigue, profuse sweating and lack of appetite for the past month. He had a history of direct contact with domestic animals and consumption of unpasteurized milk. The physical therapist junior consulted the physical therapy consultant regarding the flare up of symptoms. The physical therapy examination revealed grossly restricted mobility of knees and ankles, particularly left knee which had marked swelling and increased heat. The patient did not report any recent history of trauma. The physical therapy consultant immediately referred the patient to his medical doctor to monitor and control the flare up and exclude any new systemic diseases. The medical doctor conducted all necessary investigations and confirmed the new diagnosis of Brucellosis. Brucella micro agglutination test was used to confirm the diagnosis of Brucellosis. The first serum sample was taken on the first week of being sick while the second serum sample was taken after 3 weeks of being sick. Agglutination tests proved to be very sensitive, specific and positive in all patients with Brucellosis [5]. After 4 weeks of being diagnosed with Brucellosis, the patient resumed physical therapy and rehabilitation program. A new physical therapy examination was conducted. Patient reported that he has generalized body ache, decreased mobility and agility, and functional decline. Patient had poor posture in terms of forward head posture and mild kyphosis. Patient had dull ache of 3-4/10 at neck and shoulder blades which is getting worse. Pain is 2/10 at best and 7/10 at worst. Pain slowing down the patient during most of activity of daily living and affects his quality of life. Objective physical examination revealed marked restricted movement of hips, knees and ankles in conjunction with increased heat. There was significant effusion of left kneeas shown in figure 1 in addition to swelling of periarticular structures as shown in figure 2. Swelling of the knee joint was assessed using midpatellar girth measurements. The knee was milked from distally to proximally in an attempt to move the swelling from the knee joint area. The left knee had grade 3+ since the effusion was large enough not to respond to the milking manoeuver. Right knee had grade 2+ and both ankles had grade 1+. Patient managed to demonstrate full spinal and upper extremities mobility but of poor quality. Manual muscle test showed good to good-/normal grade for lower limbs and fair to good-/normal for trunk muscles. Patient had difficulties to balance on one leg especially when eyes are closed. Patient had difficulties to walk on line with tandem feet. Observational gait analysis revealed mild unsteadiness and slow gait. Neurological examination did not show any apparent deficits. Special testing confirmed left shoulder supraspinatus tendinitis and bilateral hip adductors tendinitis. Patient could not manage to transit between standing and full squat position. Patient managed to finish 5x sit- to- stand in 31 seconds. Physical therapy and rehabilitation program immediately restarted aiming to control symptoms, restore mobility, improve muscle strength and improve physical& functional capacity. The therapist applied small amplitude oscillatory mobilization to restore the knee and ankle mobility. Neck retraction with overpressure was used to correct forward neck posture. Patient was demonstrated with gradual automobilization of lower limbs from on all four- position. Patient had to slowly and gradually move his hips in an attempt to touch his heels with his buttocks to restore full mobility of the restricted joints. Patient was also instructed to balance on one hand and knee using cross crawl and rotational stability balance exercises as tolerated. Patient was instructed to breathe normally and tuck his stomach and feel the core muscles. This study was approved by the Ethics Committee of College of Medical Rehabilitation Sciences, Taibah University (approval No. CMR-PT-2018-08). The study conforms to the declaration of Helsinki. Informed consent was obtained from the patient to publish this case report.
 Figure 1: Swollen left knee of a 48-year-old Saudi male diagnosed with rheumatoid arthritis & brucellosis.
Figure 1: Swollen left knee of a 48-year-old Saudi male diagnosed with rheumatoid arthritis & brucellosis.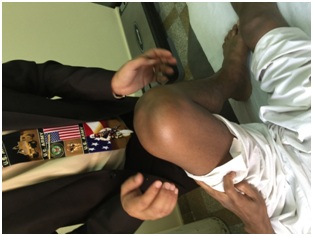
Figure 2: Puffy left knee of a 48-year-old Saudi male with swollen periarticular structures.
DISCUSSION
To the best of knowledge extracted from thorough literature review, this is the first case to be reported in medical literature describing clinical progression and physical rehabilitation outcomes of complex case of Rheumatoid Arthritis concomitant with brucellosis. Furst reported that patients with RA have shown a heightened risk of serious infections. Brucellosis is one of the infections that could happen in patients with RA [4,6]. Colmenero et al., and Turan et al., stated that osteoarticular complications of the locomotive system are disabling and have high prevalence [7-9]. Authors added that persistent arthritis being the main feature. Duyur et al., reported a case of knee arthritis due to Brucellosis in a patient with rheumatoid arthritis [4]. The authors discussed the medical treatment for the knee arthritis but did not mention any physical therapy rehabilitation. The present patient has chief complaint of knees and ankles synovitis, cervical pain, hip adductor tendinitis, shoulder tendinitis and progressive loss of flexibility. Patient’s age, gender, and polyarthritis concur with what have been reported by Geyik et al., [10] regarding Brucellosis. The osteoarticular complications of the knees and spine are in harmony with what have been reported in literature as the most commonly affected anatomical regions and body sites in Brucellosis with osteoarticular involvement [9-11]. The patient has also mentioned consuming un-pasteurized milk in addition to being in direct contact with animals which have been the culprit of transmission of Brucellosis [9]. Saudi Arabia is highly endemic for Brucellosis and needs to eradicate the disease or control it such as in developed countries [12]. The patient complaints correspond with the musculoskeletal involvement reported by many researchers except of not reporting the sacroiliitis and lumbar pain as chief complaints [9,10].
After 4 weeks of physical therapy, patient has better posture, good/normal right knee strength, grade 1+ of right knee effusion, good/ normal trunk balance and stability, better quality of shoulders’ mobility, steadier and faster gait pattern. Patient is showing more mobility to transit between standing and squatting but could not managed to fully squat. Patient also managed to execute 5x sit-to- stand test in 21 seconds. Patient has shown fair progress but still far from age matched community ambulant group who had 6.2 ± 1.3 seconds [13]. Left knee swelling did not show any improvement; it has grade 3+ effusion, periarticular swelling and feels hot. Both ankles still have grade 1+ joint effusion. Clinically, grade 3+ is more serious reaction to the disease or the activity. Moreover, effusion causes capsular distension, diminishes the quadriceps efficiency and leads to pathomechanical consequences. Physical therapists should primarily emphasize on controlling the joint swelling to proceed with different rehabilitation techniques [1].
Moreover, hip adductors tendinitis and shoulder tendinitis showed slow and minimal improvement. Patient was educated to use cold applications, hydrotherapy and assistive technology to provide symptomatic relief. Aerobic exercises should be tailored to fit patient’s interim functional capacity aiming to combat the destructive disease effect [1]. The patient raised the concern of keep losing his body weight despite finishing the medications being taken for brucellosis. The physician prescribed doxycycline and gentamicinantibiotics in addition to corticosteroids for treating Brucellosis. Patient stated that he received the treatment for 3 month and since then is being carefully monitored [9]. He has been told that he still has the antibodies of the disease. It always takes up to 12 month to be out of the bone [10,14].
After 4 weeks of physical therapy, patient has better posture, good/normal right knee strength, grade 1+ of right knee effusion, good/ normal trunk balance and stability, better quality of shoulders’ mobility, steadier and faster gait pattern. Patient is showing more mobility to transit between standing and squatting but could not managed to fully squat. Patient also managed to execute 5x sit-to- stand test in 21 seconds. Patient has shown fair progress but still far from age matched community ambulant group who had 6.2 ± 1.3 seconds [13]. Left knee swelling did not show any improvement; it has grade 3+ effusion, periarticular swelling and feels hot. Both ankles still have grade 1+ joint effusion. Clinically, grade 3+ is more serious reaction to the disease or the activity. Moreover, effusion causes capsular distension, diminishes the quadriceps efficiency and leads to pathomechanical consequences. Physical therapists should primarily emphasize on controlling the joint swelling to proceed with different rehabilitation techniques [1].
Moreover, hip adductors tendinitis and shoulder tendinitis showed slow and minimal improvement. Patient was educated to use cold applications, hydrotherapy and assistive technology to provide symptomatic relief. Aerobic exercises should be tailored to fit patient’s interim functional capacity aiming to combat the destructive disease effect [1]. The patient raised the concern of keep losing his body weight despite finishing the medications being taken for brucellosis. The physician prescribed doxycycline and gentamicinantibiotics in addition to corticosteroids for treating Brucellosis. Patient stated that he received the treatment for 3 month and since then is being carefully monitored [9]. He has been told that he still has the antibodies of the disease. It always takes up to 12 month to be out of the bone [10,14].
CONCLUSION
Physical therapists and rehabilitation clinicians should put the possibility of Brucellosis in their list of differential diagnosis in endemic areas, even among patients formerly diagnosed with RA. Comprehensive objective physical examination should be continuously conducted to differentiate the flare up of RA from the possibility being affected by Brucellosis in addition to modify the rehabilitation program accordingly. Population education, medical precautions, early diagnosis and management are essential to minimize the harmful effects of Brucella and its deleterious complications. The clinical and physical picture should be fully discussed with the treating physician since the steroids and other medications may have the potential of masking symptoms.
ACKNOWLEDGMENT
The authors would like to thank deanship of scientific research at Taibah University for facilitating the research work.
CONFLICT OF INTEREST
The authors have no financial conflicts of interest.
AUTHOR’S CONTRIBUTION
TME conceived and designed the study, and conducted the data collection. TME and SMA analyzed and interpreted the data in addition to the final review of the results. TME and SMAwrote the initial and final draft of the report and send it for publication. All authors are responsible for the findings and have critically reviewed and approved the final draft.
REFERENCES
- Luqmani R, Hennell S, Estrach C, Birrell F, Bosworth A, et al. (2009) British Society for Rheumatology and British Health Professionals in Rheumatology Guideline for the Management of Rheumatoid Arthritis (the first two years). Rheumatology 48: 436-439.
- Brocq O, Millasseau E, Albert C, Grisot C, Flory P, et al. (2009) Effect of discontinuing TNFalpha antagonist therapy in patients with remission of rheumatoid arthritis. Joint Bone Spine 76: 350-355.
- Verhoef J, Toussaint PJ, Zwetsloot-Schonk JHM, Breedveld FC, Putter H, et al. (2007) Effectiveness of the introduction of an International Classification of Functioning, Disability and Health-based rehabilitation tool in multidisciplinary team care in patients with rheumatoid arthritis. Arthritis Rheum 57: 240-248.
- Duyur B, Erdem HR, Ozgocmen S (2001) Paravertebral abscess formation and knee arthritis due to Brucellosis in a patient with rheumatoid arthritis. Spinal Cord 39: 554-556.
- Mert A, Ozaras R, Tabak F, Bilir M, Yilmaz M, et al. (2003) The sensitivity and specificity of Brucella agglutination tests. Diagn Microbiol Infect Dis 46: 241-243.
- Furst DE (2010) The risk of infections with biologic therapies for rheumatoid arthritis. Seminars in Arthritis and Rheumatism 39: 327-346.
- Colmenero JD, Reguera JM, Martos F, Sánchez-de-Mora D, Delgado M, et al. (1996) Complications associated with Brucella melitensis infection: a study of 530 cases. Medicine 75: 195-211.
- Colmenero JD, Reguera JM, Fernandez-Nebro A, Cabrera-Franquelo F (1991) Osteoarticular complications of brucellosis. Ann Rheum Dis 50: 23-26.
- Turan H, Serefhanoglu K, Karadeli E, Togan T, Arslan H (2011) Osteoarthritis involvement among 202 Brucellosis cases identified in central Anatolia region of Turkey. Intern Med 50: 421-428.
- Geyik MF, Gür A, Nas K, ?evik R, Sarac J, et al. (2002) Musculoskeletal involvement in brucellosis in different age groups: a study of 195 cases. Swiss Med Wkly 132: 98-105.
- Aydin M, Fuat Y, Savas L, Reyhan M, Pourbagher A, et al. (2005) Scintigraphic findings in osteoarticular brucellosis. Nuc Med Commun 26: 639-647.
- Memish ZA (2001) Brucellosis control in Saudi Arabia: prospects and challenges. J Chemother 13: 11-17.
- Bohannon RW, Shove ME, Barreca SR, Masters LM, Sigouin C (2007) Five-repetition sit-to-stand test performance by community-dwelling adults: A preliminary investigation of times, determinants, and relationship with self-reported physical performance. Isokinetics and Exercise Science 15: 77-81.
- Güzey FK, Emel E, Sel B, Bas NS, Özkan N, et al. (2007) Cervical spinal Brucellosis causing epidural and paravertebral abscesses and spinal cord compression: a case report. Spine J 7: 240-244.
Citation: El-gohary TM, Abd Elkader SM (2019) Rheumatoid Arthritis Concomitant with Brucellosis: Case Report in Addition to Clinical and Rehabilitation Outcomes. J Phys Med Rehabil Disabil 5: 031.
Copyright: © 2019 Tarek M El-gohary, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

Journal Highlights
© 2026, Copyrights Herald Scholarly Open Access. All Rights Reserved!
