
Risk of Post-Operative Stroke in Asymptomatic Patients with Known Extra-Cranial Carotid Artery Disease Undergoing Non-Cardiac Surgery
*Corresponding Author(s):
Mehrdad Mac FaridCleveland Clinic Lerner College Of Medicine, Department Of Vascular Medicine, Heart & Vascular Institute, Cleveland Clinic Florida, Case Western Reserve University, Weston, FL, United States
Tel:+1 9546595230,
Email:faridm@ccf.org
Abstract
Post-operative patients may carry a higher risk for stroke compared to non-surgical patients. Patients with advanced age, hypertension, atrial fibrillation and prior history of stroke are considered to have higher propensity for post-operative stroke. However, information on post-operative risk of stroke in patients with asymptomatic carotid disease is scant. From a single center vascular laboratory data base we retrospectively identified 1844 carotid arteries in 922 patients who had carotid artery ultrasonography examination and underwent a non-cardiac surgery from 2011 to 2015.
944 carotids corresponding to 472 patients were selected after process of exclusion. A total of 364 carotid arteries identified to have less than 19% stenosis serving as normal control arm. 308 carotids had mild intimal plaques or calcifications falling in category of 20-39% stenosis, 124 carotids had 40-59%, 117 carotids had 60-79%, 7 had critical stenosis of over 80% and 8 had total carotid occlusion. Stenosis in each carotid artery was considered an independent variable as a risk for an ipsilateral brain stroke or Transient Ischemic Attack (TIA).
All participants post operatively were observed for signs and symptoms of adverse neurological event. No stroke or TIA was observed postoperatively in either arm.
Keywords
Carotid artery; Embolism; Occlusion; Post-operative; Post-procedure; Stenosis; Thrombosis
INTRODUCTION
Few information regarding the risk of stroke in patients with preexisting extra-cranial carotid occlusive disease undergoing non-cardiac surgery is available in literature, however, preoperative assessment is a common reason for referral to a vascular specialist. Stroke is a devastating complication after surgical procedures, associated with a post-operative mortality rate up to 26%, compared to 12.6% in non-surgical patients [1,2]. The incidence after cardiac surgery ranges from 1.4% to 4.3%, with the most widely accepted mechanism related to embolization of aortic athermanous debris or calcified plaques [3]. Cardiothoracic, carotid and major vascular surgeries, especially if performed in emergency setting are associated with a higher risk of cerebrovascular events compared to non-vascular and less extensive elective surgeries [4-6]. Higher age, prior stroke, atrial fibrillation and HTN were associated with higher perioperative and post-operative stroke risk [5,7].
Data regarding post-operative stroke following abdominal, urogenital, gynecological and orthopedic surgeries or procedures is limited. In a retrospective study, Ng et al., reported a stroke incidence ranging from 0.05 to 7.4% following a variety of non-carotid, non-cardiac surgeries, in a non-homogenous population with variable cardiovascular risk [8].
METHOD
Our study aimed to examine the incidence of post-operative cerebrovascular events in patients with asymptomatic extra-cranial carotid artery stenosis undergoing non-cardiac surgery. After Institutional Review Board approval was obtained, an Electronic Medical Records search was performed looking at hospital admissions and discharges and Vascular Laboratory Registry using ICD 10 codes (165.29, 165.23, 165.21, S15.009A) to identify individuals who had carotid disease and subsequently underwent a non-cardiac surgery or procedure within 2 years.
All carotid artery studies were performed with IU 22 Philips Ultrasound units (Bothell, WA) in a laboratory accredited by the Intersectional Accreditation Commission (IAC) [9].All exams were performed by a certified Radiology Vascular Technologist using IAC recommended protocols. Carotid stenosis was classified and documented using University of Washington criteria ranging from < 19% up to 100% stenosis [10].
Patients were included only if they required general anesthesia for surgery or a procedure. Surgical procedures were classified as low, intermediate or high risk as defined in preoperative clearance literature [11]. The Electronic Medical Record was used to obtain demographic, clinical, operative information. Postoperative follow-up evaluation was conducted within 2 weeks with attention to neurological events including Transient Ischemic Attack (TIA) or stroke, validated based on the American Stroke Association diagnostic criteria [12]. Additional risk factors for neurological event including age, presence of atrial fibrillation, hypertension, diabetes, body mass index or previous TIA or stoke were recorded in control and in individuals with significant carotid stenosis of over 60%.
Each carotid artery was enrolled as an independent variable and only a stroke or TIA in an ipsilateral cerebrum corresponding to same side stenotic carotid artery was recorded as an adverse neurological event after excluding for non-carotid related etiological factors for stroke. In the event that postoperative neurological events were noted, contributing factors such as hemodynamic instability, resuscitation or re-intubation were assessed.
STATISTICAL ANALYSIS
We looked at selected individuals with associated demographics (Table 1).
|
|
Right Side Stenosis |
Left Side Stenosis |
||||
|
Variable |
<20% stenosis (n=177) |
>60% stenosis (n=73) |
P Value |
<20% stenosis (n=187) |
>60% stenosis (n=75) |
P Value |
|
Gender |
||||||
|
Male |
99 (55%) |
38 (52%) |
0.6742 |
108 (57.7%) |
40 (53%) |
0.6072 |
|
Female |
78 (44%) |
35 (47%) |
79 (42.2%) |
35 (46%) |
||
|
Age |
68.84±10.6 |
72.6±9.2 |
<0.011 |
69±10.54 |
74.9±8.4 |
<0.011 |
|
BMI |
26.51±3.2 |
26.8±4.8 |
0.921 |
26.7±3.84 |
25.6±3.6 |
0.041 |
|
Comorbidities |
||||||
|
Hypertension |
114 (64.4%) |
51 (69%) |
NS |
115 (61.4%) |
54 (72%) |
0.12 |
|
Hyperlipidemia |
115 (87.5%) |
47 (64%) |
NS |
119 (63.6%) |
49 (65%) |
NS |
|
Diabetes |
68 (38.4%) |
20 (73%) |
0.12 |
70 (37.4%) |
25 (33%) |
0.52 |
|
Melitus |
||||||
|
Atrial |
13 (7%) |
7 (9%) |
0.72 |
12 (6%) |
6 (8%) |
0.82 |
|
Fibrillation |
||||||
Table1: Baseline patient characteristics. Group comparisons were made using student t-test for continuous variable and Chi square or Fisher’s test for categorical variables.
BMI: Body Mass Index
Standard statistical analysis was performed using Windows version 3.3.2 software. Group comparisons were made using student t-test for continuous variable and Chi square or Fisher’s test for categorical variables. Prevalence of carotid stenosis of over 60% was significantly higher in older age, an increased BMI was associated with more frequent carotid stenosis reaching a statistical significance in left carotid artery.
RESULT
Our study demonstrated no stroke or TIA in 580 carotids with variable degree of stenosis undergoing non cardiac surgery. This included 117 carotids with stenosis of over 60% and 6 carotids with critical stenosis of 80-99 and 8 carotids with total occlusion with variable degree of stenosis in other carotid arteries.
DISCUSSION
Nine-hundred and twenty-two patients were identified. After exclusions for prior TIA or stroke, missing demographic information, suboptimal carotid ultrasound studies and inadequate postoperative documentation or neurological status, 472 patients were included in the study corresponding to 944 carotid arteries (Figure 1). From this group, 380 carotids which had <19% stenosis served as control group and 580 carotids had variable degree of occlusive disease (Figure 2).
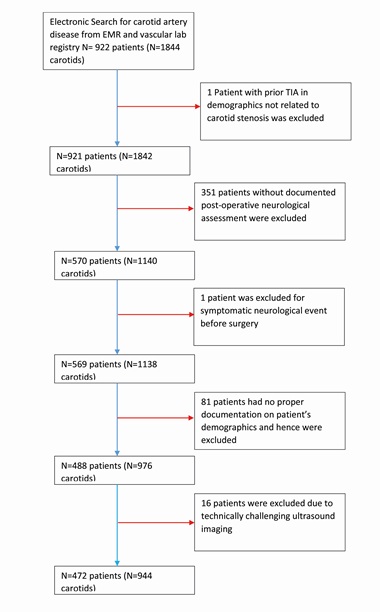 Figure 1: Patient selection flow diagram.
Figure 1: Patient selection flow diagram.
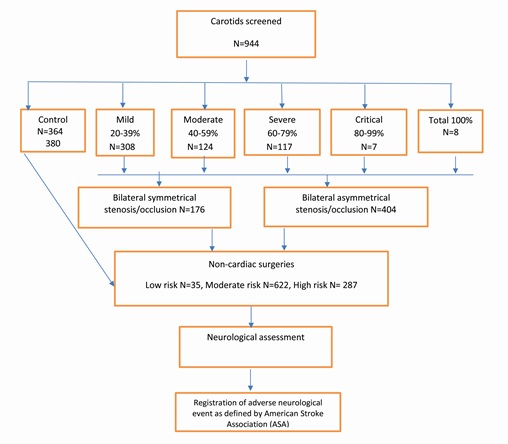 Figure 2: Algorithm of study design and recruitment of carotid arteries without and with various degree of stenosis undergoing non-cardiac surgery.
Figure 2: Algorithm of study design and recruitment of carotid arteries without and with various degree of stenosis undergoing non-cardiac surgery.
Among the carotids with significant occlusive features 8 had total occlusion and 7 had critical stenosis (Tables 2 and 3) undergoing low, intermediate and high risk surgical procedure. All individuals had clinical follow-up in two weeks and there were no neurological events (TIA or stroke) were reported.
|
ICA |
Contralateral ICA |
High Risk |
Intermediate |
Low |
|
100% |
80-99% (n=1)* |
· Hernia repair |
|
|
|
100% |
60-79% (n=1) |
· Spine surgery |
|
|
|
100% |
40-59% (n=2) |
· Colon surgery · Hernia repair |
|
|
|
100% |
20-39% (n=3) |
· Knee arthroplasty · Spine surgery |
· Hernia repair |
|
|
100% |
0-19% (n=1) |
· Hernia repair |
|
Table 2: Characteristic of surgeries in patients with total occlusion of carotids and with various degree of stenosis in contralateral carotid artery.
ICA: Internal Carotid Artery.
|
ICA |
Contralateral ICA |
High Risk |
Intermediate |
Low Risk |
|
80-99% |
80-99% (n=2) |
· Hernia procedure · Bariatric procedure |
||
|
80-99% |
60-79% (n=1) |
· ENT surgery |
||
|
80-99% |
40-59% (n=2) |
· Nephrectomy |
· Pilonidal abscess removal |
|
|
80-99% |
20-39% (n=1) |
· Eye procedure |
Table 3: Characteristic of surgeries in patients with critically stenotic carotids (80-99%) with various degree of stenosis in contralateral carotid artery.
ICA: Internal Carotid Artery.
LIMITATION
Limitations to our study include the retrospective nature of investigation and the small sample size of patients with critical stenosis or total occlusion undergoing surgeries. Although still a small sample size to determine the risk of an infrequent event, this study provides some reassurance to the expectation that TIA or stroke following non-carotid, non-cardiac surgery is rare, in part due to differing pathophysiology.
CONCLUSION
No TIA or stroke was observed in asymptomatic patients with known extracranial carotid artery stenosis undergoing a variety of non-cardiac surgeries suggesting that no intervention is required during preoperative assessment by a vascular specialist.
CONFLICT OF INTEREST STATEMENT
There are 5 authors involved in producing this article. All authors contributed in designing, data collection and writing of the article. All authors had direct access to data which was collected in Redcap a secure web application to manage surreys and database. There has been no industry found to use for the preparation of our manuscript. There has been no financial or personal interest that may affect objectivity and therefore outcome of the study (A separate COI letter was signed previously and attached to publisher web already).
FUNDING
The study was supported by research fund from Vascular Medicine Department at Cleveland Clinic Florida.
REFERENCES
- Parikh S, Cohen JR (1993) Perioperative stroke after general surgical procedures. NY State J Med 93: 162-165.
- El-Saed A, Kuller LH, Newman AB, Lopez O, Costantino J, et al. (2006) Geographic variations in stroke incidence and mortality among older populations in four US communities. Stroke 37: 1975-1979.
- Hilker M, Arlt M, Keyser A, Schopka S, Klose A, et al. (2010) Minimizing the risk of perioperative stroke by clampless off-pump bypass surgery: A retrospective observational analysis. J Cardiothorac Surg 5: 14.
- Hart R, Hindman B (1982) Mechanisms of perioperative cerebral infarction. Stroke 13: 766-773.
- Wong GY, Warner DO, Schroeder DR, Offord KP, Warner MA, et al. (2000) Risk of surgery and anesthesia for ischemic stroke. Anesthesiology 92: 425-432.
- Bucerius J, Gummert JF, Borger MA, Walther T, Doll N, et al. (2003) Stroke after cardiac surgery: A risk factor analysis of 16,184 consecutive adult patients. Ann Thorac Surg 75: 472-478.
- Menon U, Kenner M, Kelley RE (2007) Perioperative stroke. Expert Rev Neurother 7: 1003-1011.
- Ng JL, Chan MT, Gelb AW (2011) Perioperative Stroke in Noncardiac, Nonneurosurgical Surgery. Anesthesiology 115: 879-890.
- IAC Vascular Testing. Sample Protocol for Performing Extracranial Cerebrovascular Duplex Examination. IAC Vascular Testing, UK.
- Zierler R, Stardness D (1987) “Noninvasive dynamic and real-time assessment of extracranial cerebrovasculature”. In: Wood JH (ed.). Cerebral Blood Flow: Physiologic and Clinical Aspects. McGraw-Hill, New York, UAA.
- Brown TA (2013) Surgical Risk Stratification system. Medical University of South Carolina, South Carolina, USA.
- Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, et al. (2013) An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44: 2064-2089.
Citation: Farid MM, Rammohan R, Mountjoy-Cross T, Asher C (2020) Risk of Post-Operative Stroke in Asymptomatic Patients with Known Extra-Cranial Carotid Artery Disease Undergoing Non-Cardiac Surgery. J Non Invasive Vasc Invest 5: 020.
Copyright: © 2020 Mehrdad Mac Farid, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

