
Robotic Neurorehabilitation in Neuro-COVID with Presentation of Clinical Cases
*Corresponding Author(s):
Ivet B KolevaMedical University Of Sofia, Bulgaria
Email:dr.yvette.5@gmail.com
Abstract
Ultimately, contemporary Information and Communication Technologies (ICT) were introduced in the rehabilitation practice. We use Exoskeletons, virtual reality, robotic rehabilitation with Locomat (Hocoma system for balance and gait training) and ThyroMotion system (for grasp training).
Our purpose was to emphasize the impact of robotic rehabilitation in the process of recovery of patients with neurological complications of COVID-19, as follows: cerebral vascular accidents, spinal ischemic stroke, relapses of multiple sclerosis, Guillain-Barre syndrome, development of rare diseases (as cerebellar ataxia or amyotrophic lateral sclerosis /motor neuron disease), etc.
We present typical and rare clinical cases (consequences and complications of COVID-19), treated by robotic neurorehabilitation.
Our results demonstrated positive effects of ICT-application on the neuroplasticity, functional recovery and quality of life of neurological patients.
We consider introduction of robotics as necessary tool in the process of neurorehabilitation.
Keywords
Information and communication technologies (ICT); Neurological complications of COVID-19; Neuroplasticity; Neurorehabilitation; Neuro-COVID; Robotics; Virtual reality
List of Abbreviations
ADL Activities of Daily Living
CA Cerebellar Ataxia
CFS Chronic Fatigue Syndrome
CNS Central Nervous System
CoP Center of Pressure
COVID-19 Corona-virus (induced) disease 2019
CT Computer Tomography
EMG Electromyography
ET Ergotherapy
GBS Guillain - Barré syndrome
ICT Information and Communication Technologies
KT Kinesitherapy
ME Myalgic encephalomyelitis
MMT Manual Muscle Test
MRI Magnetic Resonance Imagery
NR Neurorehabilitation
PAHO Pan-American Health Organization
PIR Post-isometric relaxation
PNS Peripheral Nervous System
PRM Physical and Rehabilitation Medicine
RT-PCR Real-time reverse transcriptase Polymerase-chain-reaction
SARS-CoV-2 Severe acute Respiratory Syndrome, (provoked by) corona-virus-2
UK United Kingdom
WHO World Health Organization
COVID-19 And Neurological Complications
COVID-19
Corona-Virus Disease 2019 (COVID-19), caused by the newly emerged corona-virus, or severe acute respiratory syndrome - corona-virus 2 (SARS-CoV-2), affected public health in many countries, including Bulgaria.
Clinical manifestations include fever, cough, shortness of breath, headache, fatigue, myalgia and arthralgia, in some cases - anorexia, ageusia and anosmia (loss of taste and smell). Consequences of severe and critical forms of COVID include Respiratory insufficiency, Deconditioning, Dysphagia, Joint stiffness and pain, critical-illness related Myopathy and Neuropathy, and complications of the central and peripheral nervous system [1].
Ultimately post-COVID or long COVID-19 syndrome was described, including: Fatigue, Difficulty breathing; Shortness of breath, Cough; Joint pain; Chest pain; Severe Acute Respiratory Syndrome (SARS); Fast or pounding heartbeat; Muscle pain or headache; Loss of taste and/or smell; Rash or hair loss.
Clinical spectrum of corona-virus induced disease include the continuum from oligo- and pauci-symptomatic forms to different degrees of respiratory insufficiency and multi-systemic dysfunction until multi-organ failure. Extra pulmonary manifestations are: hematologic, cardio-vascular, renal, gastro-intestinal and neurological.
Neurological complications of COVID-19
Neurological manifestations of corona-virus are considered as public health emergency of international concern [2].
First data on the topic neurologic complications of COVID-19 were from Wuhan, China [3]. Prof. Ling Mao (from the Department of Neurology of Union Hospital Tongji medical college, Huazhong University of Sciences and Technology) and collaborators divided neurological manifestations of hospitalized patients with COVID-19 in symptoms and diseases of the Central Nervous System (CNS), of peripheral nervous system (PNS) and skeletal muscular symptoms. Only cases, confirmed by a positive result to real-time Reverse Transcriptase polymerase-Chain-Reaction (RT-PCR) assay, were included. 41 % of patients were with severe COVID-infection, and 59 % - with non-severe infection. Authors classified most patients (36%) in the group “CNS symptoms and diseases” with: headache, dizziness, impaired consciousness, ataxia, epilepsy and acute cerebrovascular disease (ischaemic stroke or cerebral haemorrhage, diagnosed by head CT). The rest of patients were in the groups “PNS symptoms” (hypogeusia, hyposmia, hypopsia and neuralgia) and “Skeletal muscular symptoms” (myalgia, elevated serum creatin-kinase level above 200 U/L).
In a UK-surveillance study of hospitalized patients [4], Varatharaj and collaborators (2020) identified the most common neurological and psychiatric conditions: anosmia, stroke (ischemic, thrombotic and haemorrhagic), delirium, brain inflammation, encephalopathy, primary psychiatric syndromes, and peripheral nerve syndromes. They explain neurological and neuropsychiatric complications of acute COVID-19 with immune activation and inflammation within the central nervous system. Vascular dysfunction and thrombotic microangiopathy in the brain explain stroke incidence. Authors’ opinion is that cerebrovascular events during acute COVID-19 often occur in patients with vulnerabilities to vascular disease (e.g. advanced age and cardiac disease) with potential to develop endothelial inflammation and coagulopathy.
Observations of neuroinflammation and neuronal injury in acute COVID-19 have raised the possibility that infection may accelerate or trigger future development on neurodegenerative diseases [2,5].
In long-COVID authors describe: difficulty with memory, concentration, and ability to accomplish everyday tasks; frequent headache, alterations in skin sensation; autonomic dysfunction; intractable fatigue, and, in severe cases, delusions and paranoia [4]. Serena Spudich and Avindra Nath (2022) made a parallel between long-COVID and another post-infectious syndrome - the myalgic encephalomyelitis / chronic fatigue syndrome (ME/CFS) [5].
Liu et al. classified neurological manifestations of corona-virus in four groups: acute cerebrovascular disease related symptoms (with high D-dimer levels and hypercoagulable state); intracranial infection related symptoms (as headache, epilepsy, disturbance of consciousness, and encephalitis), peripheral nervous system related symptoms (hypogeusia, hyposmia, visual deficits, neuralgia), and neuromuscular symptoms (muscle inflammation, fatigue, and muscle soreness) [6].
Zhao et al. (2020) discussed the first described case of Guillain-Barré syndrome associated with SARS-CoV-2 infection as causality or as a coincidence [7]. The first confirmed case of Guillain - Barré syndrome, established with antibodies against SARS-CoV-2 [8], was described by Helbok, et al.
Nowadays the monograph of Marco Cascella and Elvio de Blasio. “Features and Management of acute and chronic Neuro-COVID” summarizes the information on the topic neurological consequences of COVID-19 [9]. Authors divide Neuro-Covid in acute conditions and long-term effects of Neuro-COVID. In the group of acute Neuro-COVID they include signs and symptoms of the Central Nervous System (CNS), Peripheral Nervous System (PNS), skeletal muscle manifestations; psychological and psychiatric acute problems. CNS manifestations comprise: Headache (tension-type or migraine); Dizziness (combined with headache and tinnitus); Acute encephalopathy (delirium or decreased level of consciousness up to coma); Posterior reversible encephalopathy (altered consciousness, seizures, headaches and visual disturbances); Seizures (focal motor, tonic-clonic, convulsive and non-convulsive status epilepticus); Acute cerebrovascular diseases (ischemic stroke, cerebral hemorrhage, cerebral venous thrombosis); Meningitis and encephalitis (tension-type or migraine); Acute myelitis (mostly transverse myelitis, with different degrees of paresis, up to quadriplegia or paraplegia, plus sensitive and sphincter dysfunction). PNS manifestations are: Smell and taste impairment (hyposmia, anosmia, parosmia, olfactory hallucinations); Guillain - Barré syndrome (ascending flaccid paralysis with areflexia / hyporeflexia, sensory deficits); Pain (headache, muscle / joint pain, chest and abdominal pain); Cranial nerve injuries (ophtalmoparesis, facial nerve palsy - unilaterally or bilaterally). Skeletal muscles manifestations include: Asthenia and Myalgia (muscle pain, joint pain / arthralgia); Skeletal muscle injury (myalgia combined with increased serum creatinine kinase levels) - up to rhabdomyolysis. Long-term effects contain neurological sequelae (fatigue, muscle weakness, sequelae of stroke and demyelinating polyneuropathies); psychological effects (anxiety, depression, affective disorders, sleep issues, post-traumatic stress syndrome), and neurocognitive issues (e.g. brain fog).
Basic paths of neuro-toxicity are: demyelination, neurodegeneration and cellular senescence with results: acceleration of brain aging and exacerbation of neurodegenerative conditions. Mechanisms include: Immune activation and inflammation within the central nervous system; Vascular dysfunction and thrombotic microangiopathy; Neural injury; Neuro-inflammation; Endothelial inflammation and coagulopathy; Alteration of the Blood - Brain -Barrier [9].
Role of physical and rehabilitation medicine
Physical and Rehabilitation Medicine (PRM) has an important role along the care continuum of patients with COVID-19 - in the acute, post-acute and long-term stage [10]. For ambulatory cases [11], the emphasis is on breathlessness, oxidation, exercises, and management of Activities of Daily Living (ADL).
According recommendations of World Health Organization (WHO) and Pan-American Health organization (PAHO) key messages include the role of rehabilitation in the management of COVID-patients, and the continuity of rehabilitation for non-COVID-19-patients [12-14].
Elements of PRM-algorithm or NR-algorithm include (Figure 1): kinesitherapy (KT: exercises, massage), preformed physical modalities (electric currents, magnetic field, light), ergotherapy (ET: activities of daily living), thermo/balneo/peloido-therapy (paraffin, mineral waters, therapeutic mud, fango), patient education (medicaments, physical activity, diet, control of risk factors).
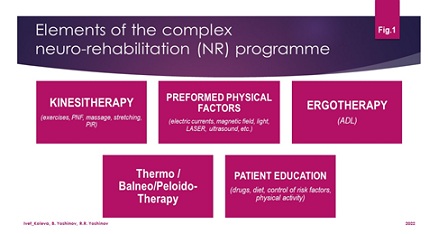 Figure 1: Elements of the complex NR-programme.
Figure 1: Elements of the complex NR-programme.
ICT
Ultimately, contemporary information and Communication Technologies (ICT) were introduced in the rehabilitation practice. Actually, we use telerehabilitation consultations and procedures, Exoskeletons, virtual reality, robotic rehabilitation with Locomat (Hocoma system for balance and gait training) and ThyroMotion system (for grasp training).
Goal of the Study
Our purpose was to emphasize the impact of robotic rehabilitation in the process of recovery of patients with neurological complications of COVID-19, e.g., cerebral vascular accidents (stroke and cerebral venous sinus thrombosis), transversal myelitis, Guillain-Barre syndrome, development of rare diseases (as cerebellar ataxia), etc. [15].
Presentation Of Clinical Cases
We present typical and rare clinical cases (consequences and complications of COVID-19), treated by robotic neurorehabilitation.
Post-stroke hemiparesis
We can present many neuro-COVID post-stroke patients. At the figure 2, we present potential of Tyro-station for training of different types of grasp: cylindrical, precise and interdigital.
 Figure 2: Grasp and grip training of post-stroke patients.
Figure 2: Grasp and grip training of post-stroke patients.
Tyro-system has the capacity to realize quantitative evaluation of the grasp recovery during consecutive sessions (Figure 3). We observe amelioration of the joints’ range of motion and of muscle force.
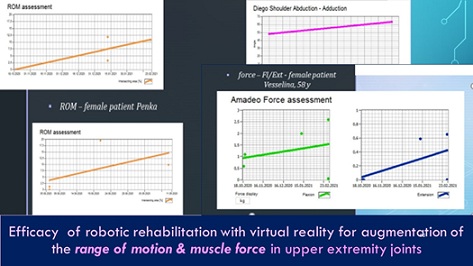 Figure 3: Efficacy of robotic NR on the range of motion and muscle force in upper extremity.
Figure 3: Efficacy of robotic NR on the range of motion and muscle force in upper extremity.
Ataxia
Cerebellar degeneration and subsequent Cerebellar Ataxia (CA) include a group of disorders, affecting coordination, balance and speech. The outlook for ataxia vary considerably, but most adult onset ataxias will get progressively worse over many years. A multidisciplinary approach is necessary in CA [16].
We present a case of a woman of 51 years, with CA, developed progressively for a period of 7-8 months; the onset was 25 days after a Corona-virus disease (fever up to 38oC, headache, fatigue, myalgia and arthralgia, without pneumonia). At the entry in our department, she presented vertigo, balance and gait instability, dysmetria and dysdiadochokinesia, muscular cramps in both legs, ataxic dysarthria. During the TYMO Balance test (TyroMotion system), we obtained oscillations of the Center of Pressure (CoP) and extended sway area, with considerable anterior-posterior displacement. The instability increases on instable surface and after eyes’ closure. Romberg index 0.74 (Figure 4).
 Figure 4: Balance assessment on the Tymo-stable and unstable platform and Balance test report - [oscillations of the CoP - with open eyes and closed eyes, on stable and unstable platform].
Figure 4: Balance assessment on the Tymo-stable and unstable platform and Balance test report - [oscillations of the CoP - with open eyes and closed eyes, on stable and unstable platform].
The detailed digitalized evaluation of the equilibrium was the base for elaboration of a complex rehabilitation programme, emphasizing on balance, gait and coordination training; adapted to the clinical specificity of the concrete patient. We included balance training in sitting and in straight position; exercises on weight distribution with alternative weight transfer between both legs, balance training on stable and unstable platforms; coordination exercises with small, medical balls and different gadgets.
Continuous exercise programs have shown positive results. Many studies provide Class III evidence that coordination training improves motor performance and reduces ataxia symptoms in patients with progressive Cerebellar Ataxia [17].
Transversal myelitis
We present the case of a young man of 25 years. Two weeks after COVID, he received weakness of the left leg and progressively (for 1 week) he developed left hemiparesis. The urgent Magnetic Resonance Imagery (MRI) of the brain and cervical medulla demonstrated post-inflammatory and degenerative-dystrophic changes, described as a lesion - band from medulla oblongata to the level C6, without changes after contrast; suspected transverse myelitis with viral genesis (Figure 5). Somatosensory evoked potentials were effectuated with data of altered somatosensory afferentation of demyelinating type in the sections of ‘plexus brachialis - proximal myelon’ and ‘plexus brachialis - cerebral cortex’.
At the entry he presented quadri-pyramidal syndrome with Babinski bilaterally, left central hemiparesis and central monoparesis of the right leg, spasticity +++; static and locomotory ataxia. We applied complex NR-program, including: KT, ET, electrical stimulations for feet extensors, gait training with Lokomat - Hocoma system. After four months we obtained reduction of muscle weakness, increase of the active range of motion of extremities’ joints, balance and gait stabilization (Figure 5). Actually, the patient has an independent gait without assistance or technical aids.
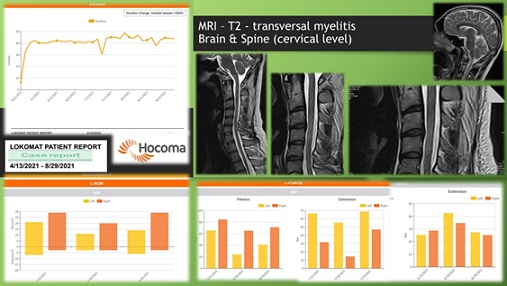 Figure 5: Case with Transversal myelitis: MRI and Lokomat results.
Figure 5: Case with Transversal myelitis: MRI and Lokomat results.
Guillain - Barré Syndrome (GBS)
We present a case of a man, 44 years old. One month (35 days) after COVID, he developed GBS (inflammatory immune neuropathy). During the clinical exam at the entry, we observed inferior flaccid paraplegia. Results of the Manual Muscle Test (MMT) were 1+/2- for flexors and extensors of hip, knee and ankle joints. EMG-data demonstrated severe segmentary demyelination and axonal dysfunction of peripheral nerves of lower extremities. Comorbidities: Visceral obesity, metabolic syndrome, arterial hypertension, non-insulino-dependent diabetes mellitus.
We applied a complex NR course of three months, including KT, ET, Nivalin iontophoresis, functional electrostimulations for the feet extensors, robotic NR with Lokomat. At the end of the NR-course: we observed inferior flaccid paraparesis, MMT 3+; the gait was possible with two canes (Figure 6).
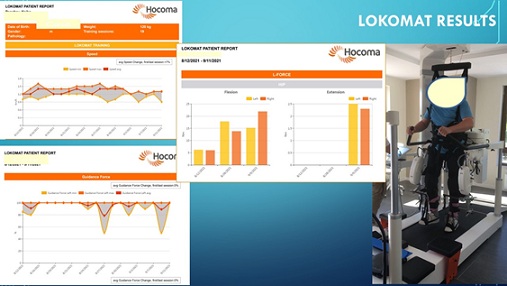 Figure 6: Case with GBS: Lokomat training and results.
Figure 6: Case with GBS: Lokomat training and results.
Discussion - Neuroplasticity
Neuroplasticity is considered as: the adult brain’s ability to adapt. According the medical dictionaries: “neuroplasticity is the brain’s capacity to reorganize itself by forming new neural connections throughout life”. The “aim” of neuroplasticity is to optimize neural networks during phylogenesis, ontogenesis and physiological learning, and in case of a brain disease [18]. Neuroplasticity allows the neurons to compensate the injury or disease and to adjust their activities in response to new situations or to changes in their environment. Principal mechanisms of brain repair are based on brain plasticity (spontaneous recovery, input of “axonal sprouting” and “mirror-neurons”, use-dependent plasticity, synaptic or grey matter plasticity, white matter plasticity).
The goal of NR is the patient’s adaptation to the “new” situation (of neuronal alteration). For this, we use two types of modulation techniques: stimulation of some functions (e.g. motor and sensory functions) and inhibition of other (e.g. pain reduction). For stimulation, we apply training of the altered motor function (through movements and activities - use-dependent plasticity) and some compensatory mechanisms (bypass strategies, replacement of functions by aiding devices, adaptation of the environment to patient’s needs). For inhibition, we apply pain management mechanisms: blocking the nociception and the neurotransmission, peripheral sympaticolysis, input of the gate-control, peripheral and central desensitization, influence on the descending systems for pain control and activation of the encephalic blocking system of the central nervous system, activation of reflectory connections.
Neuroplasticity is the pathophysiological basis for treatment of the cerebral lesions through physical training and rehabilitation, including goal-directed activities. Rehabilitation is a functional therapy, based on a detailed functional assessment [19]. Practically, every rehabilitation process is founded on neuroplasticity (training or use-dependent plasticity).
Based on our modest clinical practice (of 30 years) in the NR-field and our own results, we emphasize on the capacity of physical modalities for stimulation of neuroplasticity (especially on activity-induced plasticity), on the potential for functional recovery and amelioration of independence in everyday life of neurological patients [20,21].
Conclusion
The complex NR-programme is effective for stimulation of activity-dependent neuroplasticity. Our results demonstrated positive effects of ICT-application on the neuroplasticity, functional recovery, autonomy and quality of life of neuro-COVID-patients.
A multidisciplinary approach is necessary in cases with neurological consequences of COVID-19. We consider introduction of robotics as a necessary tool in the process of neurorehabilitation. The digitalized evaluation is useful for the elaboration of a complex NR-programme, adapted to the individual patient with neurological consequences of COVID-19.
Acknowledgement
No competing interests. No ethical issues. Requirements of the Declaration of Helsinki (1964) were respected. The correspondent institutional committee did ethical approval. All patients signed written informed consent for participation in the study and for publication.
References
- Li YC, Bai WZ, Hashikawa T (2020) The neuro-invasive potential of SARS-CoV-2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol 92: 552-555.
- Wan D, Du T, Hong W, Chen L, Que H, et al. (2021) Neurological complications and infection mechanism of SARS-CoV-2. Signal Transduction and Targeted Therapy 6: 406.
- Mao L, Jin H, Wang M, Hu Y, Chen S, et al. (2020) Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China, China. JAMA Neurology 77: 683-
- Varatharaj A, Thomas N, Ellul MA, Davies NWS, Pollak TA, et al. (2020) Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry, 10: 875-882.
- Spudich S, Nath A (2022) Nervous system consequences of COVID-19. Science 375: 6578.
- Liu K, Pan M, Xiao Z, Xu X (2020) Neurological manifestations of the coronavirus (SARS-CoV-2) pandemic 2019-2020. J Neurol Neurosurg Psychiatry 91: 669-670.
- Zhao H, Shen D, Zhou H, Liu J, Chen S (2020) Guillain-Barre syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol 19: 383-384.
- Helbok R, Beer R, Loscher W, Boesch S, Reindl M, et al. (2020) Guillain-Barre syndrome in a patient with antibodies against SARS-CoV-2. Eur J Neurol 27: 1754-1756.
- Cascella M, De Blasio E (2022) Features and Management of Acute and Chronic Neuro-Covid. - Cham: Springer Nature Switzerland Page no: 172.
- Kiekens C, Boldrini P, Andreoli A, Avesani R, Gamna F, et al. (2020) Rehabilitation and respiratory management in the acute and early post-acute phase. "Instant paper from the field" on rehabilitation answers to the Covid-19 emergency. Eur J Phys Rehabil Med 56: 323-326.
- Bury T, Clague-Baker N, Deutsch J, Finucane L, Hobbelen H, et al. (2020) World Physiotherapy response to COVID-19. Briefing paper 2. Rehabilitation and the vital role of physiotherapy. Page no: 15.
- WHO (2020) Coronavirus disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update. WHO, Geneva, Switzerland.
- WHO (2020) Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: WHO Interim Guidance. WHO, Geneva, Switzerland.
- Pan American Health Organization and WHO (2020) Rehabilitation considerations during the COVID-19 outbreak. PAHO, Washington DC, USA, Page no: 22.
- Aprile, I, Germanotta, M, Cruciani, A, Loreti S, Pecchioli C, et al. (2020) Upper Limb Robotic Rehabilitation after Stroke: A Multicenter, Randomized Clinical Trial. J Neurol Phys Ther 44: 3-14.
- Benussi, A, Cantoni, V, Manes, M, Libri I, Dell’Era V, et al. (2021) Motor and cognitive outcomes of cerebello-spinal stimulation in neurodegenerative ataxia. Brain 144: 2310-2321.
- Ilg W, Synofzik M, Brötz D, Burkard S, Giese MA, et al. (2009) Intensive coordinative training improves motor performance in degenerative cerebellar disease. Neurology 73: 1823-1830.
- Didier J (2004) La plasticité de la fonction motrice. Collection de l’Académie Européenne de Médecine de Réadaptation. Springer Verlag, Paris, France. Page no: 476.
- Koleva IB, Yoshinov BR, Yoshinov RR (2020) Balance and gait Neurorehabilitation in multiple sclerosis with significant fatigue and spasticity. Neurophysiol Res 2: 1-4.
- Koleva IB, Ioshinov B, Ioshinov R (2019) Clinical Neurorehabilitation (electronic monograph). SIMEL Press, Sofia, Bulgaria. Page no: 678.
- European Physical and Rehabilitation Medicine Bodies Alliance (2018) White Book on Physical and Rehabilitation Medicine in Europe. Introductions, Executive Summary, and Methodology. Eur J Phys Rehabil Med 54: 125-155.
Citation: Koleva IB, Yoshinov BR, Yoshinov RR (2022) Robotic Neurorehabilitation in Neuro-COVID with Presentation of Clinical Cases. J Clin Stud Med Case Rep 9: 0143.
Copyright: © 2022 Ivet B Koleva, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

