
Role of 3D Ultrasonography and Hysteroscpy in Detecting Uterine Cavity Pathologies
*Corresponding Author(s):
Rohina AggarwalDepartment Of Obstetrics & Gynecology, Institute Of Kidney Disease & Research Centre, Civil Hospital, India
Tel:+91 9428025744,
Email:drrohinaaggarwal@gmail.com
Abstract
Background: Evaluation of Uterine cavity can be done using Hysterosalpingography (HSG), Trans Vaginal Ultrasonography (TVS), Sonohysterography (SHG) and Hysteroscopy. Uterine cavity abnormalities, e.g., endometrial polyps, submucous myomas, intra- uterine adhesions, endometritis and uterine septum may result in Abnormal Uterine Bleeding (AUB) in the form of menorrhagia or metrorrhagiaor or failure to conceive. Hence exclusion of intrauterine pathology is important for abnormal uterine bleeding and infertility treatment.
Objective: To compare diagnostic accuracy and efficacy of three dimensional transvaginal ultrasound (3D-TVS) and hysteroscopy in detecting uterine cavity abnormalities, in patients with abnormal uterine bleeding and infertility.
Design and setting: An Observational Prospective Study in the Department Of Obstetrics & Gynecology in the Institute of Kidney disease & Research Centre, Civil Hospital, Ahmedabad, India from January 2018 to February 2019 was conducted.
Materials and methods: Two hundred patients with abnormal uterine bleeding and infertility were studied prospectively. 100 patients had Abnormal Uterine Bleeding as chief complaint and 100 patients had Infertility as chief complaint. 2Dimensional (2D) Transvaginal Ultrasonography followed by 3Dimensional (3D) Ultrasonography and hysteroscopy were performed in the mid to late follicular phase of menstrual cycle. Uterine cavity characteristics and abnormalities were noted.
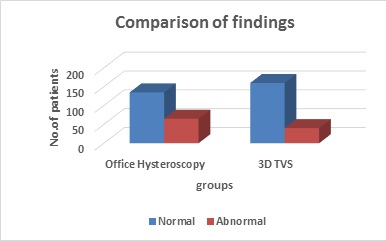
Results: Qualitative data were presented as number and percentage. Comparisons between groups were estimated by chi-square test. Abnormal findings were detected in 32.5% patients by hysteroscopy and in 20% patients by 3D ultrasonography. A probability value (p value) < 0.01 was considered significant. Endometrial Polyp was detected in 14% of patients on hysteroscopy as compared to 7.5% patients by 3D ultrasonography with p-value
Conclusion: Hysteroscopy is a safe and reliable procedure to evaluate benign endometrial lesion, direct visualization of uterine cavity with high diagnostic accuracy. It has the advantage of simultaneous treatment or biopsy procedures in few cases while 3D USG is non invasive and good tool for basic evaluation of uterus and adnexa.
Keywords
Abnormal uterine bleeding (AUB); Hysteroscopy; Infertility; Trans vaginal ultrasonography (TVS); Uterine cavity
Introduction
Uterine cavity evaluation can be done using Hysterosalpingography (HSG), Trans Vaginal Ultrasonography (TVS), Sonohysterography (SHG) and Hysteroscopy [1]. Hysteroscopy is the gold standard for evaluation of the uterine cavity because it permits direct visualization of the uterine cavity, showing characteristics of lesions, including nature, size, shape, location and vascular pattern. Unsuspected uterine cavity abnormalities, such as uterine septum, endometrial adhesions, endometrial polyps ,endometritis and small submucous myomas, which may cause abnormal uterine bleeding or reduce the chances of success in ART by interfering with implantation or causing spontaneous abortion [2]. Intrauterine pathologies were found in 11-40% of infertile patients [3]. Therefore, exclusion of intrauterine pathology is an important step before starting ART and treatment of any discovered lesion may improve ART outcome [2]. 3D-Trans-Vaginal Sonography examines three planes simultaneously, producing a 3D rendering and reconstruction of the coronal plane, which is not visible in 2D-US [3]. Three D images are developed from data obtained with a single sweep of the Ultra Sound beam across the uterus; a factor that may decrease interobserver variability. So 3D-TVS can adequately overcome the limitations of 2D ultrasound and improves the diagnostic accuracy for detecting uterine cavity abnormalities [4]. Pitfalls with 3 D-TVS may have limitations in detection of submucous fibroids in the presence of multiple fibroids, intrauterine adhesion, distinguishing hyperplastic endometrium from polyp, and distinguishing arcuate from septate uterus [5]. Although hysteroscopy has very few associated complications, perforation, cervical laceration, bleeding and vasovagal reaction may occur. Hysteroscopy may also achieve only limited access in cases of cervical stenosis.
The aim of this study was to determine the diagnostic accuracy of 3D-Trans Vaginal Sonography compared with hysteroscopy in detecting uterine cavity abnormalities in women with various different uterine pathologies.
Materials and Methods
This prospective observational cross-sectional study was conducted in the Department of Obstetrics and Gynecology, of Kidney disease & Research Centre, Civil Hospital, Ahmedabad, India after getting approval from Institutional Review Board. From January 2018 to February 2019. Total 200 patients with different gynecological complaints; 100 patients had abnormal uterine bleeding and 100 patients had infertility as main complaint were recruited.
Inclusion criteria
- Women between 20-45 Years
- No history of medical disorder like cardiac disease, haematological and thyroid disorder
- No history of active Sexually Transmitted Disease or Pelvic Inflammatory Disease
- No active vaginal bleeding and
- No pregnancy
Probable causes of infertility and description of Abnormal Uterine Bleeding (AUB) were also noted. Written informed consent was taken. Ultrasound and hysteroscopy were performed in the mid to late proliferative phase of the menstrual cycle so as to prevent abortion of an early pregnancy and to minimize confusion of a thickened secretory endometrium of the second half of the cycle.
2D Transvaginal Ultrasonography (TVS) followed by 3D Transvaginal Ultrasonography (TVS) was performed by a single operator using a Voluson E10 Expert 3D-US system (GE Healthcare ) with a RIC5- 9H microconvex intracavity ultrasound transducer in a standardized manner at a maximum sweep angle of 180°. The transducer was held steady by the investigator, and the patient was instructed to hold her breath and refrain from moving. At 9 MHz probe frequency setting, a mid-sagittal view of the uterus filling 75% of the screen and three-dimensional box size including the uterine fundus to the cervix, a 3D volume was obtained through the uterus by an automated system. The image was then presented in a multiplanar display, showing three perpendicular planes through the volume: the sagittal, transverse, and reconstructed coronal views. By scrolling through the reconstructed coronal view, multiple images were obtained by the sonographer. All cases were performed on the same machine by the same operator. Images were saved.
3D Trans Vaginal Sonography findings were recorded as follows:
- Mullerian Anomalies in the form of unicornuate, bicornuate. septate, subseptate or arcuate uterus. Diagnosis of an Intra uterine septum was made, if the central point of indentation was at an acute angle (< 90°), along with no fundal myometrial indentation while if the central point of indentation was at obtuse angle (> 90°) along with significant fundal myometrial indentation the diagnosis of bicornuate uterus was made (Figures 1-3)
- Intrauterine adhesions seen as irregularities and calcification of endometrium (Figure 4)
- Endometrial polyp seen as hyperechoic thickening of the endometrial mucosa (Figure 5)
- Submucous leiomyoma (a solid, whorled, and mixed echogenic tumor disrupting and Affecting the endometrial interfaces) Size, grade and location of polyps and submucous leiomyoma were documented (Figure 6)
- Foreign body in uterine cavity (Figure 7)
- Normal Uterine Cavity (Figure 8)
Hysteroscopy was performed as an office procedure without anaesthesia, after putting the patient in the dorsal lithotomy position. Premedication with injection Atropine to prevent vasovagal attack and injection Buscopan was given. Tab Misoprostal 400 microgram was kept in vagina early morning so as to fascilitate hysteroscope insertion. Vagina was cleaned with povidone-iodine. Hysteroscopy was performed using 2.9 mm, 30 degree rigid Bittochi hysteroscope using vaginoscopic approach with advancement inside the cervical canal and uterine cavity was done under vision. Continuous irrigation of the uterine cavity was done using Normal saline maintaining an intrauterine pressure of 100 mm Hg. The standard sequence of inspecting vagina, ectocervix, endocervical canal, uterine cavity, endometrium and tubal ostia was followed. The fundus was visualized between the two ostia and the scope was withdrawn slowly to see all the four walls of the uterus, by turning light cable to 360 degrees for this purpose.
Hysteroscopic findings were allocated either to “the uterine cavity lesions” or “the endometrial aspect characterization”. The uterine cavity lesions [6] that were found including: endometrial polyp, cervical polyp, myoma, endometrial adhesions, congenital malformation, Lost Intrauterine Device (IUD). In the endometrial aspect characterization, differentiation between functional, atrophic or thin endometrium, dysfunctional, endometritis, cystic atrophy, hyperplasia, polypoidal and carcinoma was done. The mean time required for the procedure was about 10 minutes. Video recording of hysterscopy was done.
Statistical methods- Data acquired included 3D TVS and hysteroscopy
Data were recorded and statistically analyzed by Statistical Package for the Social Sciences (SPSS) version 20. Qualitative data were presented as number and percentage. Comparisons between groups were estimated by chi-square test. Probability values (p value) less than 0.01 and 0.04 were considered significant.
Results
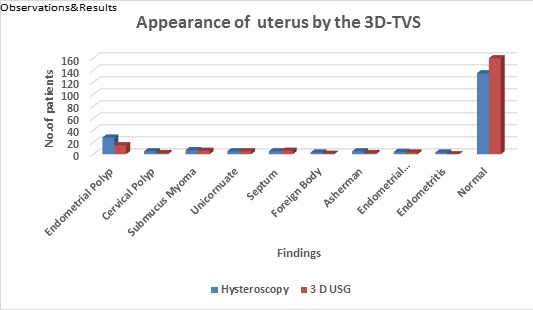
Two hundred women were recruited for the study. 3D transvaginal ultrasonography and hysteroscopy were successfully performed in all women. Among the studied population, 100 (50%) women complained of infertility (Group A) whereas abnormal uterine bleeding (Group B) was the main complaint of the other 100 (50%) women (Table 1). Out of Infertile women 35 (70%) had primary infertility while 15 (30%) had secondary infertility (Table 1). Mean age of subjects was 33±3.6 years in Group A and 37±4.3 in Group Bas shown in table 2 by hysteroscopy 67.5% normal uterine cavities were diagnosed as compared to 80% by 3D USG (Table 3), which is also statistically significant (p-value <0.01). Ultrasonographic and hysteroscopic findings are shown in table 4. Hysteroscopy showed 65 cases of positive findings, including endometrial polyp in 28 patients, submucous myomas in 7 patients, 5 cases of intrauterine adhesions and 10 case of mullerian anomalies and 3D-TVS showed pathological findings in 40 cases with 15 cases of endometrial polyps and missed the diagnosis of endometrial polyps in 13 cases, which is also statistically significant (p-value <0.04). On USG endometrial polyp's appearance was like hyperplastic endometrium as depicted by Figure 9. Hence it was misinterpretated as endometrial hyperplasia. Commonest lesion detected was endometrial polyp (14.0% cases) in 32.5% of abnormal hysteroscopic findings and in 7.5% cases of 20%cases of abnormal USG findings (Table 5).
Observations & results
|
|
Infertility (Group A) |
Menorrhagia (Group B) |
Total Number of cases |
|
|
|
Primary Infertility |
Secondary Infertility |
|
|
|
Number of Cases |
70 |
30 |
100 |
200 |
|
Percentage (%) |
35% |
15% |
50% |
100% |
Table 1: Distribution of patients according to chief complaints.
|
|
Infertility (Group A) Mean±SD |
Range |
Menorrhagia (Group B) Mean±SD |
Range |
|
Parity |
2.67±0.90 |
0-5 |
2.60±0.88 |
01-Jun |
|
Mean Duration (Years) of Complaints |
4.9±3.9 |
2-18 (Years) |
4.8±2.6 |
1-4 (Years) |
|
Mean Age (Years) |
33±3.6 |
22-43 (Years) |
37±4.3 |
34-45 (Years) |
Table 2: Demography.
|
|
Office Hysteroscopy |
3D TVS |
Chi-square value |
P value |
|
Normal |
135 (67.5%) |
160 (80%) |
8.07 |
<0.01* |
|
Abnormal |
65 (32.5%) |
40 (20%) |
||
|
Total |
200 |
200 |
|
|
Table 3: Findings.
*Represents significant difference between 2 groups.
|
Findings
|
Hysteroscopy |
3 d USG
|
p-value |
|
Endometrial Polyp |
28 (14%) |
15 (7.5%) |
0.04* |
|
Cervical Polyp |
5 (2.5%) |
2 (1%) |
0.45 (NS) |
|
Submucus Myoma |
7 (3.5%) |
6 (3%) |
0.78 (NS) |
|
Unicornuate Uterus |
5 (2.5%) |
5 (2.5%) |
1.00 (NS)
|
|
Uterine Septum |
5 (2.5%) |
6 (3%) |
0.76 (NS) |
|
Foreign Body in Uterus |
3 (1.5%) |
1 (0.5%) |
0.62 (NS) |
|
Asherman Syndrome |
5 (2.5%) |
2 (1%) |
0.45 (NS) |
|
Endometrial Hyperplasia |
4 (2%) |
3 (1.5%) |
1.00 (NS) |
|
Endometritis |
3 (1.5%) |
0 (0%) |
0.25 (NS) |
|
Normal |
135 (67.5%) |
160 (80%) |
<0.01* |
Table 4: Appearance of the Uterus by the Three Dimensional TVS.
*Represents significant difference between 2 groups
|
Complications |
Hysteroscopy (N=200) |
3 d USG (N=200) |
|
Vasovagal Reaction |
2 (1%) |
Nil |
|
Uterine Perforation |
2 (1%) |
Nil |
|
Cervical Laceration |
4 (2%) |
Nil |
|
Haemorrhage
|
8(4%) |
Nil |
|
Abdominal Cramps |
20 (10%) |
Nil |
|
Vaginal Spotting |
36 (18%) |
Nil |
|
Infection |
2 (1%) |
Nil |
Table 5: Complications during Procedure. 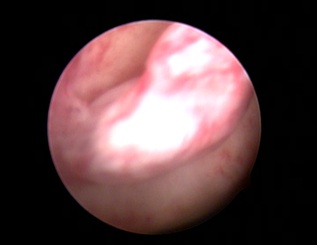
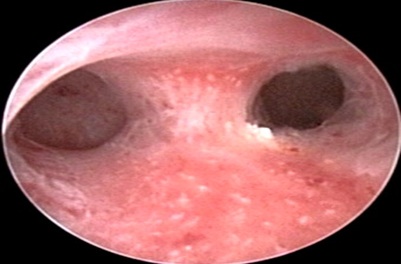
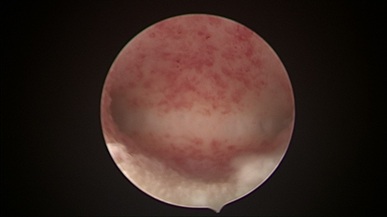
Hysteroscopy showing Polyp in Uterine Cavity.
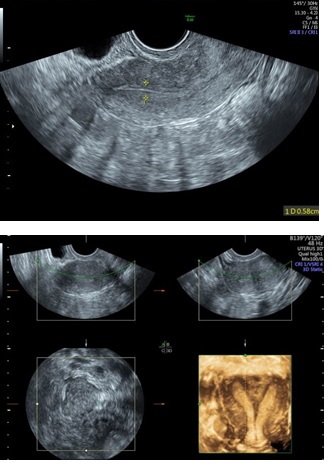 Figure 1: 2D & 3D USG showing Septum in Uterine Cavity.
Figure 1: 2D & 3D USG showing Septum in Uterine Cavity.
 Hysteroscopy showing Septate Uterus.
Hysteroscopy showing Septate Uterus. 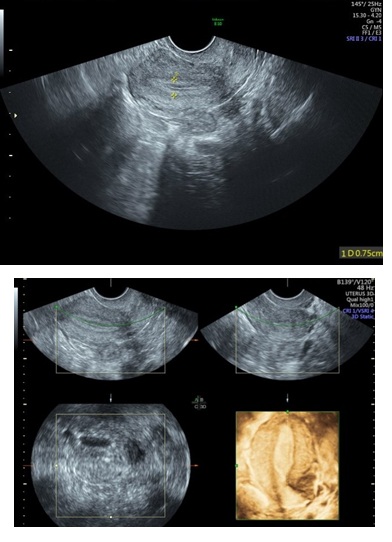
Figure 2: 2D & 3D USG showing Unicornuate Uterus.
 Hysteroscopy showing Unicornuate Uterus.
Hysteroscopy showing Unicornuate Uterus.
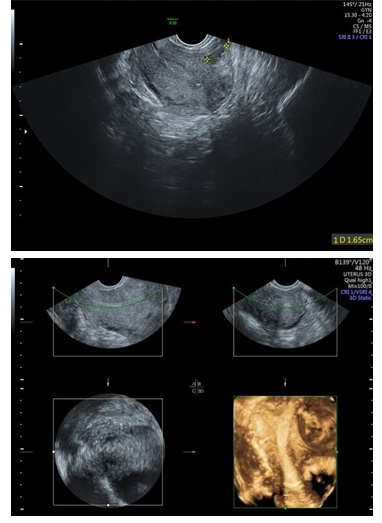 Figure 3: 2D & 3D USG showing Subseptate Uterus.
Figure 3: 2D & 3D USG showing Subseptate Uterus.
 Hysteroscopy showing Submucus Fibroid in Uteruine Cavity.
Hysteroscopy showing Submucus Fibroid in Uteruine Cavity.
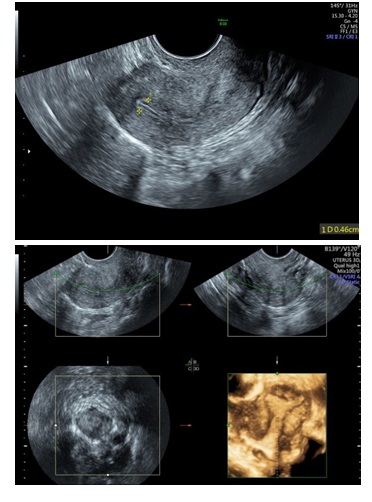 Figure 4: 2D & 3D USG showing Adhesions in Left Cornua of Uterine Cavity (Asherman Syndrome).
Figure 4: 2D & 3D USG showing Adhesions in Left Cornua of Uterine Cavity (Asherman Syndrome).
 Hysteroscopy showing CuT in side Uterine Cavity.
Hysteroscopy showing CuT in side Uterine Cavity.
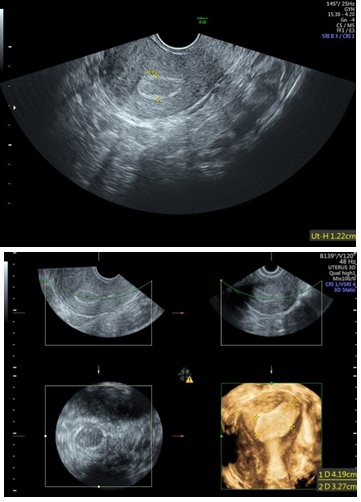 Figure 5: 2D & 3D USG showing Polyp in Uterine Cavity.
Figure 5: 2D & 3D USG showing Polyp in Uterine Cavity.
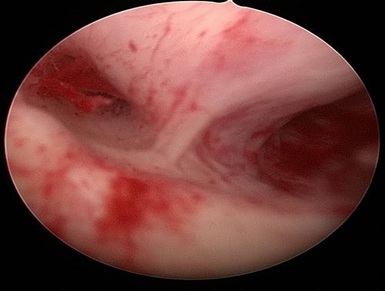 Hysteroscopy showing Subseptate Uterus.
Hysteroscopy showing Subseptate Uterus.
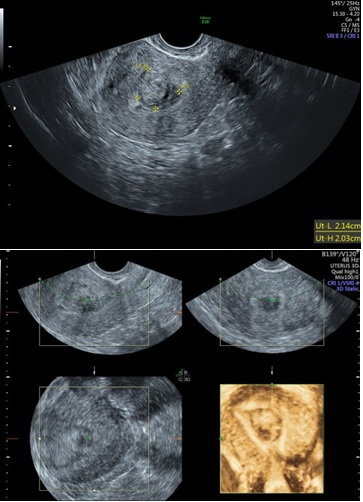 Figure 6: 2D & 3D USG showing Submucus Fibroid in Uterine Cavity.
Figure 6: 2D & 3D USG showing Submucus Fibroid in Uterine Cavity.
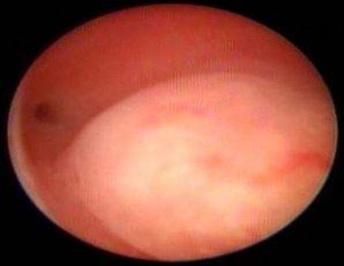
 Hysteroscopy showing Nomal Uterine Cavity.
Hysteroscopy showing Nomal Uterine Cavity.
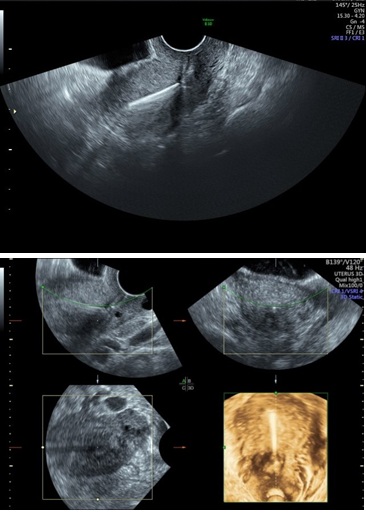 Figure 7: 2D & 3D USG showing CuT in side Uterine Cavity.
Figure 7: 2D & 3D USG showing CuT in side Uterine Cavity. 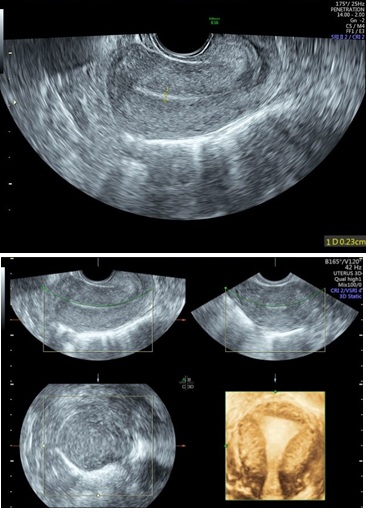
Figure 8: 2D & 3D USG showing Nomal Uterine Cavity.
 Hysteroscopy showing Adhesions in Left Cornua of Uterine Cavity (Asherman Syndrome). Left Ostia is obscured due to adhesions.
Hysteroscopy showing Adhesions in Left Cornua of Uterine Cavity (Asherman Syndrome). Left Ostia is obscured due to adhesions.
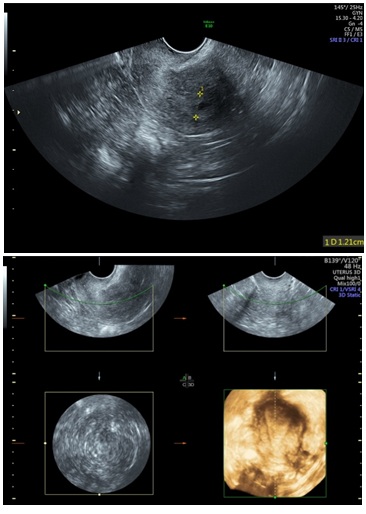 Figure 9: D & 3D USG showing Endometium Hyperplasia with small cystic space.
Figure 9: D & 3D USG showing Endometium Hyperplasia with small cystic space. 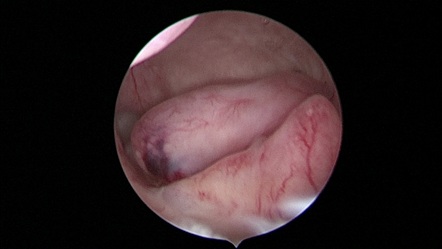
Hysteroscopy showing Multiple Endometrial Polyps inside Uterine Cavity.
Discussion
Uterine cavity is an important factor for successful implantation of the embryo. Presence of benign intrauterine lesion, such as endometrial polyps, uterine septum, intrauterine adhesions and submucous myoma may contribute to infertility or decrease chances of successful ART or bleeding. Therefore, accurate and reliable tools for uterine cavity assessment are very important. Similarly menorrhagia is easily attributed to uterine cavity abnormalities like polyp, submuocus fibroid, hyperplasia and IUCD [7]. Uterine cavity lesion is an important and correctable factor that can lead to improvement in ART outcome or a condition of abnormal uterine bleeding. Identification of accurate and reliable detection and diagnostic tools for assessment of the uterine cavity is a necessary first step in the improvement of ART success rates [8]. 3D-TVS had 84.1% diagnostic accuracy for detecting uterine cavity abnormalities in infertile women. Reports vary regarding the diagnostic accuracy of 3D-Trans Vaginal Sonography.
Three-Dimensional Ultrasonography (3D USG) in comparison to hysteroscopy is less invasive, cheaper, easily accepted by most patients and does not require much training. In most cases an endometrial polyp can be differentiated from the submucous fibroid based on the imaging characteristics. The polyps are typically round in shape, smooth in outline, and are generally echogenic, compared to the endometrium or are isoechoic to it. The underlying endometrial-myometrial interface is preserved (Figure 5). Moreover the presence of a vascular pedicle has a positive predictive value of up to 81.3%. Fibroids are more inhomogeneous, hypoechoic, and there is a loss of endometrial-myometrial interface. The percentage of the intra cavitary portions of the submucous fibroids i.e., grade of submucous myoma can be assessed on 3D USG by the degree of distortion caused by it (Picture 6).
A study by Van den Bosch [9] evaluated diagnostic accuracy of 3DTVS in detection of uterine cavity lesion in women with abnormal uterine bleeding. They found endometrial polyp in 26%, submucous myoma in 7%, endometrial hyperplasia in 6%, and cancer in 1% of subjects. They also reported 93% diagnostic accuracy, 96% sensitivity, and 91% specificity. In our study, 3D-TVS detected all cases of submucous myoma while missed 13 cases out of twenty eight cases with endometrial polyps. Even though there were only a small number of cases with submucous myoma, 3D TVS demonstrated 100% diagnostic accuracy. Hence hysteroscopy is recommended for accurate detection and diagnosis of uterine cavity lesion.
In a similar study Haemila et al., [10] in a study of females with premenopausal bleeding found that 3D TVS detected myomas in 14 (20%), polyps in 8 (11.43%), and endometrial mass in 1 while hysteroscopy detected myomas in 6 (8.57%), polyps in 11 (15.72%) and endometrial mass in 1 (1.43%). In contrast to the study above, we found that 3D TVS detected 20% abnormalities, out of which 15 (7.5%) were endometrial polyps, 6 (3%) were submucous myomas, 6 (3%) were septa, 1 (2%) were adhesions, and 5 (2.5%) was unicornuate uterus. While hysteroscopy detected 32.5% abnormalities, out of which 28 (14%) were polyps, 7 (3.5%) were submucous myomas, 5 (2.5%) were septa, 5 (2.5%) were adhesions and 5 (2.5%) were unicornuate uteruses. In our study, 3D-TVS failed to detect 13 (36.45%) cases with endometrial polyps, which were detected on hysteroscopy.
Our study demonstrated that 3D TVS had high specificity, but its sensitivity was limited, especially for detecting endometrial polyp. A significant percentage of patients had evidence of uterine cavity pathology. As such, hysteroscopy remains the preferred procedure for accurate detection and diagnosis of uterine cavity lesion.
Hysteroscopy is an accurate and less invasive method for the evaluation of uterine cavity and allows direct visualization of the endometrium, revealing the nature, location, shape, size and vascular pattern of any uterine cavity abnormalities. Complications [11] such as vasovagal reaction, Uterine perforation, Cervical laceration, Haemorrhage, are rare with hyseroscopy. The patient may experience anxiety, discomfort, and mild lower abdominal cramps during hysterscope insertion. However, the symptoms subside soon after the end of the procedure. The procedure is usually tolerated well.
Conclusion
Hysteroscopy is a safe and reliable procedure to evaluate benign endometrial lesion, direct visualization of uterine cavity with high diagnostic accuracy. It has the advantage of simultaneous treatment or biopsy procedures in few cases while 3D USG is non invasive and good tool for basic evaluation of uterus and adnexa.
References
- Maged AM, Nasr ALA, Selem MA, Allah SHG, Wali AA (2016) Uterine Cavity Assessment and Endometrial Hormonal Receptors in Women with Peri and Post Menopausal Bleeding. Trends Gynecol Oncol 1:105.
- Pundir J, El Toukhy T (2010) Uterine cavity assessment prior to IVF. Womens Health (Lond) 6: 841-847.
- Fang L, Su Y, Guo Y, Sun Y (2013) Value of 3-dimensional and power Doppler sonography for diagnosis of endometrial polyps. J Ultrasound Med 32: 247-255.
- Bahadur A, Malhotra N, Singh N, Gurunath S, Mittal S (2013) Comparative study on the role of diagnostic hysteroscopy in evaluation of the uterine cavity prior to in vitro fertilization in a developing country. Arch Gynecol Obstet 288: 1137-1143.
- Downey DB, Fenster A, Williams JC (2000) Clinical utility of three dimensional US. Radiographics 20: 559-571.
- Michael SB, Rafael FV, Hubert G (2007) Hysteroscopy: Visual perspectives of uterine anatomy, physiology, and pathology (3rdedn). Lippincott Williams & Wilkins, Philadelphia, USA.
- Vercellini P, Cortesi I, Oldani S, Moschetta M, De Giorgi O, et al. (1997) The role of transvaginal ultrasonography and outpatient diagnostic hysteroscopy in the evaluation of patients with menorrhagia. Hum Reprod 12: 1768-1771.
- Society for Assisted Reproductive Technology; American Society for Reproductive Medicine (2007) Assisted reproductive technology in the United States: 2001 results generated from the American Society for Reproductive Medicine/Society for Assisted Reproductive Technology registry. Fertil Steril 87: 1253-1266.
- Van den Bosch T, Valentin L, Van Schoubroeck D, Luts J, Bignardi T, et al. (2012) Detection of intracavitary uterine pathology using offline analysis of three-dimensional ultrasound volumes: interobserver agreement and diagnostic accuracy. Ultrasound Obstet Gynecol 40: 459-463.
- Haemila FA, Youssef D, Hassan M, Soliman A, Mossad M (2005) A prospective comparative study of 3-D ultrasonography and hysteroscopy in detecting uterine lesions in premenopausal bleeding. Middle East Fertility Society 10: 238-243.
- Jansen FW, Vredevoogd CB, van Ulzen K, Hermans J, Trimbos JB (2000) Complications of hysteroscopy: a prospective, multicenter study. Obstet Gynecol 96: 266-270.
Citation: Aggarwal R, Mishra V (2022) Role of 3D Ultrasonography and Hysteroscpy in Detecting Uterine Cavity Pathologies. J Reprod Med Gynecol Obstet 7: 097.
Copyright: © 2022 Rohina Aggarwal, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

