
Role of Inflammatory Markers in Terminating Antibiotic Therapy in Neonate
*Corresponding Author(s):
Sagar SwarnkarDepartment Of Pediatrics, Pt Jnm Medcal College, Raipur, India
Tel:+918109301116,
Email:sagarswarnkar@gmail.com
Abstract
Background and Aim
In neonates the early features of neonatal septicemia are often non-specific, and to differentiate between infected and uninfected is not always be easy. Indiscriminate use of antibiotics may increase the risk of emergence of multi drug resistant strains. Certain laboratory parameters such as CRP, m-ESR, WBC-count collectively termed as the “inflammatory markers”. This present study aimed to study the role of inflammatory markers in terminating antibiotic therapy in neonates.
Material and Methods
This was a hospital based prospective cross-sectional study conducted in the department of pediatrics at Pt JNMCH, Raipur. Total 252 neonates admitted in NICU and started on antibiotics were included as the study subjects. Inflammatory markers were recorded for each neonate after getting informed consent from the parents. Duration of antibiotic uses in each case was recorded and analyzed with respect to laboratory parameters.
Results
In present study out of 252 sampled neonates culture reports were positive for (21.8 %) neonates. In culture positive cases the mean antibiotic duration was 9.33 days and among negative cases it was 6.80 days (p=0.025).Neonates having CRP value >6 has the median antibiotic duration was 8 days and those with CRP value
Conclusion
In conclusion, CRP and mESR has crucial role in deciding antibiotic duration and antibiotic duration can be shortened with the use of these inflammatory markers. Overall, the mean duration of antibiotics was 7 days and 9 days in culture positive cases.
Keywords
Antibiotic duration; Culture; Inflammatory markers; Neonates; NICU; Sepsis.
Introduction
Neonates do not effectively meet the requisite minimum inflammatory response that makes them more susceptible to bacterial invasion of the blood stream [1]. In neonates the early features of neonatal septicemia are often non-specific, and to differentiate between infected and uninfected is not always be easy. Indiscriminate use of antibiotics in case of presumed bacterial infection may increase the risk of emergence of multi drug resistant strains [2].
Although a positive blood culture still remains „the gold standard" for diagnosing sepsis [3,4] and takes at least 48–72 h, but availability of culture facilities in many developing countries are still far from optimal. Hence, certain rapid diagnostic tests such as C-reactive protein (CRP), micro Erythrocyte Sedimentation Rate (m-ESR), WBC count, Absolute Neutrophil Count (ANC), immature/total neutrophil count ratio, and platelet (PL) count collectively termed as the “Sepsis Screen” [5,6] can be used. None of the widespread laboratory markers of infection has enough sensitivity or specificity to detect all infected children [7,8]. Their diagnostic value might be especially limited in the early course of the disease [9,10]. Clinical management, especially decisions for antibiotic treatment, can't be based solely on hematologic markers [11].
National Neonatology forum has divided neonatal sepsis into two types. First is proven sepsis in which pathogen is isolated from blood, CSF(cerebrospinal fluid),urine or other body fluids or autopsy evidence of sepsis. Another is probable sepsis with two of the following four parameters: Total leukocyte count < 5000/cumm, Band cell to total neutrophil ratio of ≥0.2, CRP ≥ 0.6 mg/dl and micro-ESR ≥ 15 mm AEFH (at the end of first hour). This present study is done with the purpose to study the role of inflammatory markers in terminating antibiotic therapy in neonates.
Aim and Objective
- Aim
Role of inflammatory markers in Terminating Antibiotic Therapy in Neonates.
- Objectives
To study inflammatory marker and clinical condition as a condition to terminate antibiotics
To study micro ESR and CRP as a combined marker to terminate antibiotics in neonates.
Material and Methods
This was a hospital based prospective cross-sectional analytical study conducted from January 2022 to December 2022. The study was conducted in the department of pediatrics at Pt JNMCH and Dr. BRAM Hospital, Raipur, Chhattisgarh. In this study neonates admitted in NICU and started on antibiotics were included as the study subjects. The sample size for the study was calculated using the formula 4pq/d2.Where, p= 46.4%, d= relative error using 5% at 80% of confidence interval. Total number of patients enrolled in the study was 252.
Neonates admitted in the nursery with sepsis and getting antibiotic will consecutively recruited into the study after getting informed consent from the parents. All neonates included in the study will have the following done:
1. Detailed history including demographic details, 2. Detailed Examination, 3. Septic screening. Investigation done in the study subjects were: Complete haemogram, Blood glucose, Serial and quantitative CRP, micro ESR and blood culture. The outcome of the patient was recorded at the time of discharge. Duration of antibiotic uses in each cases was recorded and analyzed with respect to laboratory parameters.
Data was entered in Microsoft excel using specified format and analysis was done using SPSS-20 version. Frequency and percentages were calculated whenever required. Data was presented in mean and standard deviations. Statistical significance was taken P value < 0.05.
Results
In present study all 252 sampled neonates were included as presumptive cases for sepsis and to confirm their sepsis status culture sensitivity was done. Out of that culture reports were positive for 55 (21.8 %) neonates.
Table 1 shows the culture sensitivity profile of sampled neonates. Among culture positives 11.11% were Klebsiella, 5.56% were CoNS and 5.16% were Pseudomonas. In present study antibiotic was started among all the study subjects and the mean duration of antibiotic duration was noted.
|
Blood culture |
Freq. |
Percent |
|
Klebsiella |
28 |
11.11 |
|
Coagulase-negative staphylococci (CoNS) |
14 |
5.56 |
|
Pseudomonas |
13 |
5.16 |
|
No growth |
197 |
78.17 |
|
Total |
252 |
100 |
Table 1: Blood culture results in study subjects
Table 2 shows that in culture positive cases the mean antibiotic duration was 9.33 days that is 5 days less than the standard protocol and among negative cases mean duration of antibiotic was 6.80 days. The mean difference in duration of antibiotic in culture positive and negative cases was statistically significant (p=0.025).
|
Blood culture |
No of neonates |
Mean antibiotic duration in days |
[95% Conf. Interval] |
P value |
|
|
Positive |
55 |
9.33 |
6.75 |
12.17 |
0.025 |
|
Negative |
197 |
6.80 |
6.48 |
7.12 |
|
|
Total |
255 |
7.92 |
6.64 |
8.20 |
|
Table 2: Mean antibiotic duration in study subjects
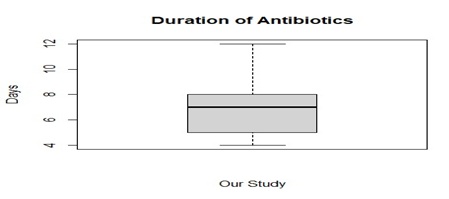 Figure 1: Median duration of antibiotic days (box whisker plot)
Figure 1: Median duration of antibiotic days (box whisker plot)
Table 3 shows that in present study neonates having CRP value >6 has the median antibiotic duration was 8 days and those with CRP value < 6 has mean antibiotic duration was 6 days. The difference in antibiotic duration days was statistically significant (p=0.015).
|
CRP value |
No of cases |
Median antibiotic duration days |
Std. dev. |
95% Confidence Interval for Median |
P value |
|
|
Lower Bound |
Upper Bound |
|||||
|
<6 |
144 (57.1%) |
6 |
1.87 |
5.63 |
7.43 |
0.015 |
|
>6 |
108 (42.9%) |
8 |
2.28 |
6.57 |
7.43 |
|
|
Total |
252 |
7.92 |
2.25 |
6.64 |
7.2 |
|
Table 3: CRP value at the time of admission and median antibiotic duration days
Table 4 shows that in present study neonates having mESR value >15 have the median antibiotic duration been 8 days and those with mESR value
|
mESR value |
No of cases |
Median antibiotic duration days |
Std. dev. |
95% Confidence Interval for Median |
P value |
|
|
Lower Bound |
Upper Bound |
|||||
|
<15 |
151(59.9%) |
7 |
1.63 |
5.71 |
7.82 |
0.031 |
|
>15 |
101 (40.1%) |
8 |
2.19 |
6.96 |
8.32 |
|
|
Total |
252 |
7.5 |
2.01 |
6.76 |
8.07 |
|
Table 4: mESR value at the time of admission and median antibiotic duration days
Table 5 shows that the decision of termination in blood culture positive cases based on inflammatory markers was successful in 94.5 % cases among 3 culture positive cases, antibiotics were restarted. In all 197 culture negative cases, antibiotics were successfully terminated. Overall out of 252 cases in 249 (98.80%) cases the antibiotics were terminated successfully
|
Blood culture |
Successful termination |
Restarted |
|
Positive (n=55) |
52 (94.54%) |
3 (5.46%) |
|
Negative (n=197) |
197 (100%) |
0 |
|
Total (N=252) |
249 (98.80%) |
3 (1.20%) |
Table 5: Successful termination of antibiotic based on laboratory markers on culture positive cases.
Discussion
The present study conducted in department of pediatrics at Pt. JNMCH, Raipur with the purpose to study the role of inflammatory markers in terminating antibiotic therapy in neonates.
In present study among sampled neonates to those antibiotics was started 21.8 % were culture positive cases and the microorganism identified were Klebsiella, CoNS and 5.16% Pseudomonas. Swarnkar K at el (2012) did a similar study and reported among the total neonates those treated for sepsis and 51.38% cases were culture proven sepsis [12]. Punyashety KB at el [2016] reported that 42% cases were positive for blood culture proven sepsis [13]. Ali S Z at el [2017] in a hospital based cross sectional study reported that total of (46.1%) cases were blood culture proven sepsis [14].
In present study antibiotic was started among all the study subjects and the mean duration was 7.92 days that is 6 days less than standard protocol. Culture positive cases the mean antibiotic duration was 9.33 days as compare to 6.80 days in negative cases. Mean difference in duration of antibiotic in both the cases was statistically significant (p=0.025).Salsabila, K et al (2022) did a similar descriptive study on early-onset neonatal sepsis and antibiotic use. The median durations of antibiotic therapy were 19 and 9 days in culture-proven and culture-negative EOS groups, respectively [15]. Wagstaff JS et al (2019) did a retrospective analysis on antibiotic treatment neonatal sepsis. Neonates with culture-positive sepsis received a mean duration of 12 days antibiotics, while the culture negative 11 days [16].
In present study overall out of 252 cases in 249 (98.80%) cases the antibiotics were terminated successfully. Among 55 culture positive cases, in 3 cases the antibiotics were restarted thus the decision of termination in blood culture positive cases based on inflammatory markers was successful in (94.5 %) cases. Newby B et al (2021) did a study on antimicrobial stewardship intervention to reduce unnecessary antibiotic doses in neonates reported that almost 75% of very-preterm and low-birth-weight babies received antibiotics [17].
Indiscriminate use of antibiotics for longer periods than required will result in drug resistance, side effects related to medication, and superimposed infection with other bacteria and fungi. Sivanandan S et al (2011) did a study on choice and duration of antimicrobial therapy for neonatal sepsis and meningitis and reported that among 91% cases the antibiotics were terminated successfully [18].
In present study neonates having CRP value >6 has the median antibiotic duration was 8 days and those with CRP value < 6 has mean antibiotic duration was 6 days and was statistically not significant (p=0.015) [19].
Conclusion
In conclusion, CRP and mESR has crucial role in deciding antibiotic duration and antibiotic duration can be shortened with the use of these inflammatory markers. Overall, the mean duration of antibiotics was 7 days and 9 days in culture positive cases. Only 3 cases the antibiotics were restarted. Thus, antibiotics duration can be shortened and drug resistance can be prevented with the use of these markers in accordance with the antibiotic stewardship program.
References
- Ghosh S, Mittal M, Jaganathan G (2001) Early diagnosis of neonatal sepsis using a hematological scoring system. Indian J Med Sci 55: 495-500.
- Ng PC (2002) Diagnostic markers of infection in neonates. Arch Dis Child Fetal Neonatal Ed 89: F229-35.
- Gotoff SP, Behrman RE (1976) Neonatal septicemia. J Pediatr 76: 142-153.
- Sankar MJ, Agarwal R, Deorari AK, Paul VK (2008) Sepsis in the newborn. Indian J Pediatr 275:261-266.
- Paul VK, Singh M (1986) Diagnosis and treatment of neonatal sepsis. Indian Pediatr 23:1023-1035.
- Camacho-Gonzalez A, Spearman PW, Stoll BJ (2013) Neonatal infectious diseases: evaluation of neonatal sepsis. PediatrClin North Am 60: 367-389.
- Steinberger E, Hofer N, Resch B (2014) Cord blood procalcitonin and Interleukin-6 are highly sensitive and specific in the prediction of early-onset sepsis in preterm infants. Scand J Clin Lab Invest 74:432-436.
- Labenne M, Lizard G, Ferdynus C, Montange T, Iacobelli S, et al. (2011) A clinic-biological score for diagnosing early-onset neonatal infection in critically ill preterm infants. PediatrCrit Care Med12: 203-209.
- Doellner H, Arntzen KJ, Haereid PE, Aag S, Austgulen R (1998) Interleukin-6 concentrations in neonates evaluated for sepsis. J Pediatr132: 295-299.
- Antonakos N, Tsaganos T, Oberle V, Tsangaris I, Lada M, et al. (2017) Decreased cytokine production by mononuclear cells after severe gram-negative infections: early clinical signs and association with final outcome. Critic Care 21: 48.
- Remington JS (2011) Infectious diseases of the fetus and newborn infant. Philadelphia Elsevier.
- Swarnkar K, Swarnkar M (2012) A Study Of Early Onset Neonatal Sepsis With Special Reference To Sepsis Screening Parameters In A Tertiary Care Centre Of Rural India. The Internet Journal of Infectious Diseases 10.
- Punyashetty KB, Patil T (2016) Interpretation of haematological parameters in neonates at risk for sepsis. J Evid Based Med Healthc 3: 2492-2496.
- Ali ZS, Ghodke BA, Deka AB (2017) Sepsis screen parameters as a tool for diagnosis of neonatal sepsis. J Evolution Med Dent Sci 6: 5584-5588.
- Salsabila K, Toha NMA, Rundjan L, Pattanittum P, Sirikarn P, et al. (2022) Early-onset neonatal sepsis and antibiotic use in Indonesia: A descriptive, cross-sectional study. BMC Public Health 22.
- Wagstaff JS, Durent RJ, Newman MG, Eason R, Ward RM, et al. (2019) Antibiotic treatment of suspected and confirmed neonatal sepsis with 28 days of life: a retrospective analysis. Front Pharmacol 10:1191.
- Newby B, Mok SHS, Sun Yi (2021) Antimicrobial stewardship intervention to reduce unnecessary antibiotic doses in neonates. Am J Infect Control 49: 126-127.
- Sivanandan S, Soraisham AS, Swarnam K (2011) Choice and duration of antimicrobial therapy for neonatal sepsis and meningitis. Int J Pediatr 712150.
- Manandhar SR, Basnet R (2020) Micro-Erythrocyte Sedimentation Rate in Neonatal Sepsis of a Tertiary Hospital: A Descriptive Cross-sectional Study. JNMA J Nepal Med Assoc 58: 377-382.
Citation: Swarnkar S, Khandwal OP, Subhdha S (2023) Role of Inflammatory Markers in Terminating Antibiotic Therapy in Neonate. J Neonatol Clin Pediatr 10: 106.
Copyright: © 2023 Sagar Swarnkar, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

