
Sarcoidosis Masquerading Tuberculosis in the Post-Nasal Space
*Corresponding Author(s):
D ALNafiseeDepartment Of Otolaryngology, Royal Victoria Eye And Ear Hospital, Dublin, Ireland
Tel:+353 16028208924,
Email:dnafisee@gmail.com
Abstract
Presentation: We describe a clinical case of extra-pulmonary tuberculosis in the Posterior Nasal Space (PNS) that was initially misdiagnosed and managed as sarcoidosis.
Diagnosis: A twenty-two-year-old healthy woman presented to the Emergency Department with six months of nasal congestion and left-sided otorrhea. Otomicroscopy of the left ear and in-office nasolaryngoscopy showed polypoidal swellings in the external auditory canal and PNS, respectively. Initial biopsy showed non-caseating granulomas consistent with sarcoidosis.
Treatment: Given the absence of information in the literature on how to treat nasopharyngeal sarcoidosis, it was decided to ablate the PNS lesion using cautery and additional biopsies were sent to rule out lymphoma and re-test for Mycobacterium Tuberculosis (TB). Biopsies were culture-positive for TB and anti-TB treatment was started.
Discussion: This case highlights the importance of considering TB in the differential diagnosis for abnormal PNS tissue, especially in patients from TB endemic areas.
Keywords
Granuloma; Mycobacterium; Posterior Nasal Space; Sarcoidosis; Tuberculosis
Introduction
Extra-pulmonary tuberculosis in the nasopharyngeal region is rare and accounts for less than 1% [1]. We report a case of extra-pulmonary tuberculosis in the Posterior Nasal Space (PNS) that was initially misdiagnosed and managed as sarcoidosis at our institution.
Case Report
A 22-year-old healthy woman presented to the Emergency Department with a 6-month history of nasal congestion and left-sided otorrhea. Otomicroscopy of the left ear showed a polyp in the external auditory canal blocking direct visualization of the tympanic membrane. In-office nasolaryngoscopy showed left-sided polypoidal swelling in the Post-Nasal Space (PNS). No cervical lymph nodes were palpable on neck exam. She was treated with oral and topical antibiotics and encouraged to use a nasal rinse and decongestant. Magnetic Resonance Imaging (MRI) of the left middle ear ruled-out cholesteatoma but did identify a lesion in the deep parotid gland suspicious for necrosis and abnormal tissue in the nasopharynx which was biopsied. Histology confirmed multiple non-caseating granulomas suggestive of sarcoidosis. Given the absence of information in the literature on how to treat nasopharyngeal sarcoidosis, it was decided to ablate the PNS lesion using cautery and further biopsies were sent to out-rule lymphoma and re-test for Mycobacterium Tuberculosis (TB) (Figure1). The biopsies were culture-positive for Mycobacterium Tuberculosis complex despite not displaying respiratory symptoms. Chest x-ray and Computed Tomography scan (CT) of the thorax ruled out pulmonary TB. This could have resulted in aerosolization of the mycobacterium, but surgical staff had negative QuantiFERON Tests possibly because all were wearing FFP2 masks, customary during the COVID-19 pandemic. She was commenced on the standard four drug Anti-TB treatment for 6-months and the public health team was informed.
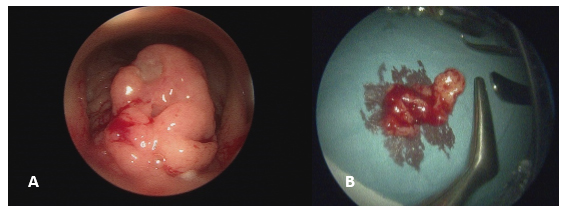 Figure 1: Intra-operative images of the post-nasal space polypoid mass pre and post excision. A) Zero degrees nasoendoscopy showing a large polypoid mass in the left post-nasal space. B) Suction adenoidectomy was performed, and samples were sent for both histology and TB culture.
Figure 1: Intra-operative images of the post-nasal space polypoid mass pre and post excision. A) Zero degrees nasoendoscopy showing a large polypoid mass in the left post-nasal space. B) Suction adenoidectomy was performed, and samples were sent for both histology and TB culture.
Discussion
Newly diagnosed Extra-Pulmonary TB (EPTB) accounts for 15% worldwide with 10-35% manifesting in the head and neck [2]. Both nasopharyngeal and salivary gland (submandibular andparotid) TB are uncommon even in endemic areas [3]. Patients typically present with nasal obstruction with or without discharge, and absence of respiratory and constitutional symptoms [2,4]. According to Qian X et al., the absence of pulmonary involvement is 70-90% in head and neck TB cases [2]. In addition to the non-specific symptoms, the paucibacillary nature revents conventional testing and delays diagnosis [2]. Anti-TB drugs for a minimum of 6-monthsremains the gold standard treatment [4]. This case highlights the importance of having a high index of suspicion for TB, and to consider it in the differential diagnosis for abnormal PNS tissue. Precautionary measures should be taken to avoid transmission to staff.
Compliance with Ethical Standards
Informed consent: Informed consent was obtained from all individual participants included in the study.
References
- Srivanitchapoom C, Sittitrai P (2016) Nasopharyngeal tuberculosis: Epidemiology, mechanism of infection, clinical manifestations, and management. Int J Otolaryngol 2016: 4817429.
- Qian X, Albers A, Nguyen D, Dong Y, Zhang Y, et al. (2019) Head and neck tuberculosis: Literature review and meta-analysis. Tuberculosi 116: 78-88.
- Nakao Y, Shibata R, Murohara T, Tanigawa T (2016) Primary nasopharyngeal tuberculosis: A case report. BMC Infectious Diseases 16: 121.
- Mishra R, Prasad B, Mathew S (2015) Nasopharyngeal tuberculosis. Med J Armed Forces India 71: 586-589.
Citation: ALNafisee D, McHugh A, Ganem JE, Mackle T (2023) Sarcoidosis Masquerading Tuberculosis in the Post-Nasal Space. J Otolaryng Head Neck Surg 9: 078.
Copyright: © 2023 D ALNafisee, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

