
Scar Sarcoidosis as Presenting Finding in Pembrolizumab Induced Systemic Sarcoidosis in Stage III Melanoma: A Case Report
*Corresponding Author(s):
Birgit ReynDepartment Of Dermatology, University Hospital Leuven, Leuven, Belgium
Email:Birgit.reyn@uzleuven.be
Abstract
Immune checkpoint blockade using inhibition of Programmed Cell Death-1 (PD-1) improves both progression-free and overall survival in patients with advanced melanoma, but is associated with a unique set of toxicities termed immune-related Adverse Events (irAEs). We present a case of a man with stage IIIc melanoma who was treated with pembrolizumab (anti PD-1). Two months after initiation of the therapy, the patient developed subcutaneous nodules on his upper lip and right knee, both in a pre-existing scar. Histological examination showed non-necrotising granuloma, most consistent with sarcoidosis. PET-CT showed hypermetabolic mediastinal and hilar adenopathies as well as lung lesions and some cutaneous and subcutaneous metabolic hot spots. Bronchoscopy with biopsy of a lymph node confirmed the diagnosis of sarcoidosis. Pembrolizumab was withheld, whereby a gradual decrease and near spontaneous resolution of all lesions was seen over a period of approximately 6 months. The patient is currently in follow up with no evidence of disease recurrence.Our case shows a unique presentation of sarcoidosis in old scar tissue as presenting symptom of pembrolizumab-related systemic sarcoidosis and demonstrates the importance of histological examination of new lesions occurring during checkpoint inhibitor therapy in order to avoid misdiagnosis of melanoma progression.
Keywords
Melanoma; PD-1 inhibitor; Pembrolizumab; Sarcoidosis; Scar
List of Abbreviations
PD-1: Programmed Cell Death-1
irAEs: Immune-Related Adverse Events
SLR: Sarcoid-Like Reactions
Introduction
Pembrolizumab is a humanized IgG4 monoclonal antibody that selectively inhibits programmed cell death-1 (PD-1) receptor on the surface of activated cytotoxic T lymphocytes. Immune checkpoint blockade using anti PD-1 has shown clinically significant antitumor response and improvement of overall survival and has been approved for the treatment of advanced melanoma, among other malignancies [1,2].
Despite important clinical benefits, checkpoint inhibition is associated with a unique spectrum of side effects termed immune-related Adverse Events (irAEs). Cutaneous toxicities appear to be one of the most prevalent irAEs. A wide range of dermatologic manifestations can occur, mainly a maculopapular rash and pruritus, but also many others such as lichenoid reactions, auto-immune skin diseases and sarcoidosis [3]. We report the case of a 52-year old patient receiving pembrolizumab for a stage IIIc melanoma who developed cutaneous sarcoidosis in two pre-existing scars as well as extracutaneous manifestations. Pembrolizumab-induced sarcoidosis / Sarcoid-Like Reactions (SLR) has already been described in medical literature [4,5], but this case is unique as the sarcoidosis developed in old scar tissue.
Case Description
We present the case of a 52-year-old male patient who was diagnosed in December 2017 with a stage IIIc (pT3bN1aM0, AJCC 8th edition) superficial spreading melanoma of the left thigh. In February 2018, a resection with 1.5 cm margin and a sentinel procedure of the left groin were performed. The sentinel node was positive for melanoma localization, for which completion iliaco-femoral lymphadenectomy was conducted. Histopathology showed negative iliacal and inguinal lymph nodes.
In January 2020, the patient relapsed with an in-transit metastasis under the resection scar on the left leg (stage IIIc, pT3bN2cM0). This metastasis was widely excised with a margin of 1 cm. Adjuvant immunotherapy with pembrolizumab (anti PD-1) was initiated in March 2020. Molecular examination showed presence of BRAF mutation, MAP2K1 mutation and TERT promoter.
Two months after the start of therapy, the patient presented early to our consultation because of a newly developed lesion on the upper lip. The lesion was located at the level of a pre-existing scar (resulting from a bike accident at adolescent age) and did not cause any local discomfort. On clinical examination we confirmed a subcutaneous, mobile nodule at the level of the upper lip further continuing into the lip mucosa, underneath an overlying scar (Figure 1A). The differential diagnosis included an epidermoid cyst, cutaneous sarcoidosis or cutaneous melanoma metastasis. Ultrasound examination of the lesion showed an iso- to hypo-echogenic tubular structure, with heterogeneous content. An incisional biopsy was planned for further histopathological investigation. During this procedure, a similar subcutaneous nodule was noticed in an existing scar on the right knee (resulting from a traumatic fall at childhood) (Figure 1B) and was biopsied as well. Histological examination of both lesions showed non-necrotising granulomatous inflammation associated with multinucleated giant cells, most consistent with sarcoidosis, in the context of hypertrophic scar tissue (Figure 1C&1D).
 Figure 1: Clinical and histological imaging. A) Scar sarcoidosis on the upper lip; B) Scar sarcoidosis on the right knee; C) Histology (H&E staining, scale 500 mm) shows hypertrophic scar tissue with underlying non-necrotising granulomatous inflammation; D) Histology (H&E staining, scale 100 mm) shows more detailed image of a non-necrotising granuloma with some multinucleated giant cells.
Figure 1: Clinical and histological imaging. A) Scar sarcoidosis on the upper lip; B) Scar sarcoidosis on the right knee; C) Histology (H&E staining, scale 500 mm) shows hypertrophic scar tissue with underlying non-necrotising granulomatous inflammation; D) Histology (H&E staining, scale 100 mm) shows more detailed image of a non-necrotising granuloma with some multinucleated giant cells.
Additional examinations were scheduled for screening of systemic sarcoidosis. Laboratory showed no relevant abnormalities with normal calcium and ACE levels. ECG was normal with the exception of sinus bradycardia. Echocardiography showed no evidence of cardiac sarcoidosis. Ophthalmological examination as well showed no arguments for sarcoidosis. PET-CT showed multiple hypermetabolic foci scattered throughout the body, most pronounced at the level of mediastinal and hilar lymph nodes, but also at the level of the cervical lymph nodes, lung, soft tissues of the thoracic wall and skin in the right prepatellar location and the upper lip (Figure 2A-C). Especially the pattern of the mediastinal lymph nodes was strongly reminiscent of sarcoidosis. Bronchoscopy with bioptic sampling confirmed the diagnosis of sarcoidosis. Lung function test was normal. The diagnosis of sarcoidosis secondary to immunotherapy with cutaneous manifestations and mediastinal and hilar adenopathies was made. Pembrolizumab was withheld. There was no indication for systemic or local steroidal therapy given the absence of pulmonary or cardiac impairment in an asymptomatic patient.
PET-CT control in November 2020 showed a substantial decrease of the known right prepatellar nodule and disappearance of the other lesions described on previous examination. There were no new suspected PDG-avid lesions. At clinical examination in January 2021, the skin lesions could no longer be felt at palpation. The patient is currently being followed with ultrasound and PET-CT. Therapy with pembrolizumab was permanently discontinued.
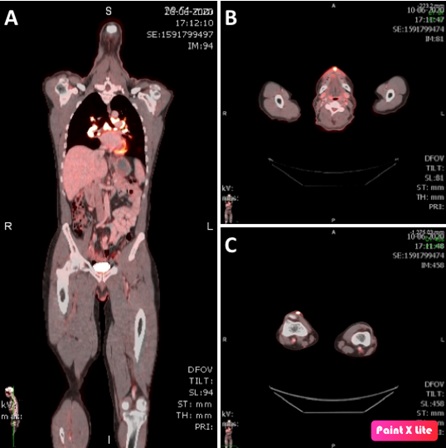 Figure 2: PET-CT imaging. A) Full body overview with multiple hypermetabolic foci, most pronounced at the level of mediastinal and hilar lymph nodes. B) Hypermetabolic foci right prepatellar. C) Hypermetabolic foci at the upper lip.
Figure 2: PET-CT imaging. A) Full body overview with multiple hypermetabolic foci, most pronounced at the level of mediastinal and hilar lymph nodes. B) Hypermetabolic foci right prepatellar. C) Hypermetabolic foci at the upper lip.
Discussion
Immune checkpoint inhibitors, including anti-PD-1 antibodies have changed the prognosis of patients diagnosed with advanced melanoma. However, these therapies have a very specific safety profile due to their unique mechanism of action. They harbor a new spectrum of adverse events that are mostly immune related (irAEs), presumably mediated by off-target effects induced by cytotoxic T cell activation [3]. Cutaneous toxicities appear to be one of the most prevalent irAEs. A wide range of dermatologic manifestations can occur, including sarcoidosis.
In anti-PD-1 therapy associated sarcoidosis, blockade of PD-1 has been associated with Th17 cell hyperactivity and increased interleukin 17 expression. This overexpression is thought to potentially induce sarcoidosis or SLR, since these cells have an important role in sarcoidosis not related with immunotherapy. We found a recent systematic review of all sarcoidosis/SLR cases under immunotherapy (CTLA-4 or PD-1) described in the medical literature [4]. Ninety-eight patients diagnosed with sarcoidosis/SLR under immunotherapy were included in this paper. Skin involvement and mediastinal and peripheral lymph nodes were the most common manifestations. There was only one case described where a SLR to pemprolizumab manifested in an old scar [6]. Therefore, our case reports a unique clinical presentation of pembrolizumab-induced sarcoidosis that manifests as clinical changes in old scar tissue.
Our case (together with the case already described [6]) shows that sarcoidosis should always be considered in the event of a reaction to previous scar tissue in patients treated with immunotherapy. Biopsy is therefore imperative to avoid misdiagnosis of melanoma progression.
References
- Kwok G, Yau TCC, Chiu JW, Tse E, Kwong YL (2016) Pembrolizumab (Keytruda). Hum Vaccines Immunother 12: 2777-2789.
- Villadolid J, Amin A (2015) Immune checkpoint inhibitors in clinical practice: Update on management of immune-related toxicities. Transl Lung Cancer Res 4: 560-575.
- Sibaud V (2018) Dermatologic Reactions to Immune Checkpoint Inhibitors: Skin Toxicities and Immunotherapy. Am J Clin Dermatol 19: 345-361.
- Rubio-Rivas M, Moreira C, Marcoval J. (2020) Sarcoidosis related to checkpoint and BRAF/MEK inhibitors in melanoma. Autoimmun Rev 19: 102587.
- Tetzlaff MT, Nelson KC, Diab A, Staerkel GA, Nagarajan P, et al. (2018) Granulomatous/sarcoid-like lesions associated with checkpoint inhibitors: A marker of therapy response in a subset of melanoma patients. J Immunother Cancer 6: 14.
- McKenna MC, Molloy K, Crowther S, Feeney J, Gillis A, et al. (2018) Pembrolizumab-related sarcoid-like reaction presenting as reactivation of quiescent scars. J Oncol Pract 14: 200-201.
Citation: Reyn B, Smets K, Boecxstaens V, Bosisio F, Garmyn M, et al. (2021) Scar Sarcoidosis as Presenting Finding in Pembrolizumab Induced Systemic Sarcoidosis in Stage III Melanoma: A Case Report. J Clin Dermatol Ther 7: 085.
Copyright: © 2021 Birgit Reyn, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

