Second trimester Abdominal Pregnancy: A Case Report in a Resource Limited Setting
*Corresponding Author(s):
Jimah B BashiruDepartment Of Medical Imaging, School Of Medical Sciences, University Of Cape Coast, Cape Coast, Ghana
Tel:+233 553299210,
Email:jimah@uccsms.edu.gh
Abstract
Introduction: Abdominal pregnancy is a rare form of ectopic pregnancy with very high feto-maternal morbidity and mortality. Diagnosis and management can pose difficulties in low-resource centres. High index of suspicion is vital in making a prompt diagnosis.
Case Presentation: A 23year old, gravida 2, para 1, who presented with a two-day history of severe abdominal pain was referred from a satellite clinic. Abdominal ultrasound scan revealed a live 18week 5day intra-abdominal pregnancy. Emergency laparotomy showed an intact gestational sac at the superior aspect of the uterus with massive hemoperitoneum. The placenta was attached to the right ovary, omentum, and fimbriae of the right fallopian tube.
Conclusion: Abdominal pregnancy is a rare occurrence and requires a high index of suspicion for prompt diagnosis. Massive hemoperitoneum can be life threatening and prompt surgical intervention is key in saving the life of the mother.
Keywords
Abdominal laparotomy; Ectopic pregnancy; Hemoperitoneum
Introduction
Ectopic pregnancy represents about 1-2% of all pregnancies with 95% occurring in the fallopian tube and abdominal pregnancies represent just about 1% of ectopic pregnancies [1]. Abdominal pregnancy is defined as pregnancy anywhere within the peritoneal cavity, exclusive of tubal, ovarian, or broad ligament locations [1]. The Pouch of Douglas (POD) is the most common location of abdominal pregnancy followed by the mesosalpinx and omentum [1]. However, implantation into other abdominal organs such as the spleen, liver, and appendix is also reported [2].
Primary abdominal pregnancy occurs when the gestational sac attaches directly to the abdominal peritoneum. In most cases, abdominal pregnancies are secondary, and the most common mechanism is implantation into the peritoneum after a tubal abortion. The abdominal pregnancy rates range between 1:10,000 and 1:30,000 in the population, and it represents 1% of extrauterine pregnancies [3]. Abdominal pregnancies are related to a high-risk of maternal morbidity and mortality with an estimated maternal and perinatal mortality of 0.5-18% and 40-95%, respectively [4,5].
Risk factors associated with abdominal pregnancy include tubal damage, pelvic inflammatory disease, endometriosis, assisted reproductive techniques, and multiparity. The diagnosis of abdominal pregnancy can be very problematic. These pregnancies can go undetected until an advanced gestational age, resulting in term pregnancy or complicated by massive hemoperitoneum [5]. Advanced abdominal pregnancy carries a risk of disseminated intravascular coagulation, bowel obstruction, and fistulae to the gastrointestinal and/or genitourinary tracts. The site of implantation and availability of vascular supply determine the possibility of fetal survival [6]. Clinical history and physical examination alone may be insufficient to make a preoperative diagnosis. Sonography is the most effective method for diagnosing an abdominal pregnancy. MRI is an emerging important, complementary imaging modality that helps not only to confirm the diagnosis but also to delineate the precise anatomical relationship between the fetus and various maternal abdominal organs.
Prompt diagnosis of extra-uterine pregnancy is important to prevent high mortality and morbidity associated with missed diagnosis.
We present a case of intra-abdominal pregnancy at 18 weeks 5 days, complicated by hemoperitoneum and successfully managed surgically.
Case Presentation
A 23-year-old woman (Gravida 2, Para 0) with a history of one previous pregnancy who presented to a satellite clinic with a two-day history of severe lower abdominal pain. She admitted taking an abortifacient to terminate the pregnancy. She had a history of vaginal bleeding with associated lower abdominal pain subsequent to her attempted termination which lasted 7 days, 8 weeks prior to presentation. She also experienced vaginal bleeding with associated lower abdominal pain of 5 days duration, 2 weeks before presentation. She took no ultrasound scans because she believed the pregnancy had been terminated.
She had a surgical history of one previous caesarean section 3 years prior and no known chronic disease. There was no history of bleeding per vaginum at presentation. Speculum exam showed a closed cervix with no blood in the os. A bedside ultrasound done at the obstetrics department showed multiple uterine fibroids and an impression of degenerating uterine fibroids were made. Confirmatory ultrasound scan revealed a single live abdominal pregnancy at 18 weeks 5days with massive free intra-abdominal fluid collection with internal echoes consistent with hemoperitoneum. The gestational sac was attached to the serosal surface of the uterine fundus. The fetal heart rate was 153bpm. The placenta was noted just inferior to the anterior abdominal wall at the level of the umbilicus, centrally, 12.7mm from the skin. The uterus was empty and anteverted. Both ovaries appeared normal in size and echopattern.The estimated gestational age was 18 weeks 5 days using biparietal diameter and femur length (Figures 1 A-D).
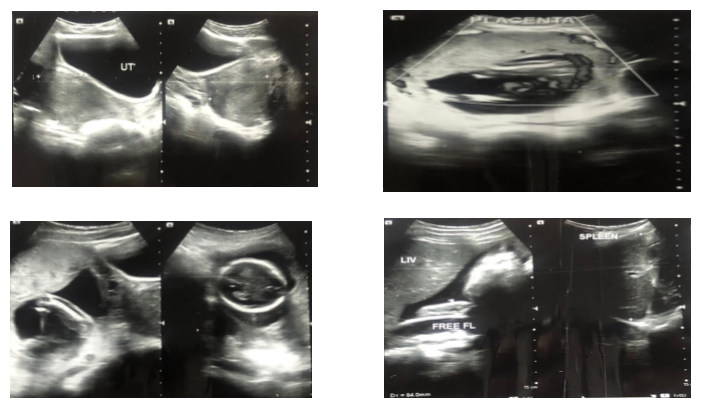
Figure 1: A-D. A. Sonogram showing empty uterus posterior to the anechoic urinary bladder. B. Sonogram showing placenta below the anterior abdominal wall. C. Sonogram showing fetal femur and fetal head. D. Sonogram showing free fluid in the abdomen consistent with hemoperitoneum.
The liver, spleen, gall bladder, pancreas, and kidneys showed normal sonographic appearance. The bowel was normal with no evidence of dilatation or fistula in the aforementioned gestational sac. Labs at presentation were: Haemoglobin 7.0g/dl, MCV 83.3fL, MCH 27.5pg, Platelet count 217, WBC 10.22, Her BP was 120/65mmHg, temperature 36.8 degree Celsius, pulse 113bpm and respiratory rate was 22. There was progressive hypotension and worsening of her vitals despite fluid resuscitation over a period of 1hour. Her pulse was 110, respiratory rate increased to 26, and her blood pressure fell to 90/60mmHg. She was transfused 4 units of blood post-operatively. Exploratory laparotomy was done on account of worsening vital signs and respiratory distress. Intra-operative findings confirmed a well-formed extra-uterine fetus in a gestational sac at the superior aspect of the uterus with an estimated weight of 200g and a massive hemoperitoneum. The estimated blood loss was 4litres. The placenta was attached to the right ovary, omentum, and fimbriae of the right fallopian tube. The left ovary and fallopian tube were normal (Figure 2). The placenta was evacuated and a damage control right salpingectomy with preservation of the right ovary. Her immediate postoperative condition was satisfactory with a blood pressure of 100/70, pulse of 70bpm, and respiratory rate of 16cpm. Her haemoglobin came up to 8g/dl with an MCV of 82.2fL, MCH of 28.0 pg, Platelet count of 44, WBC 15.05. 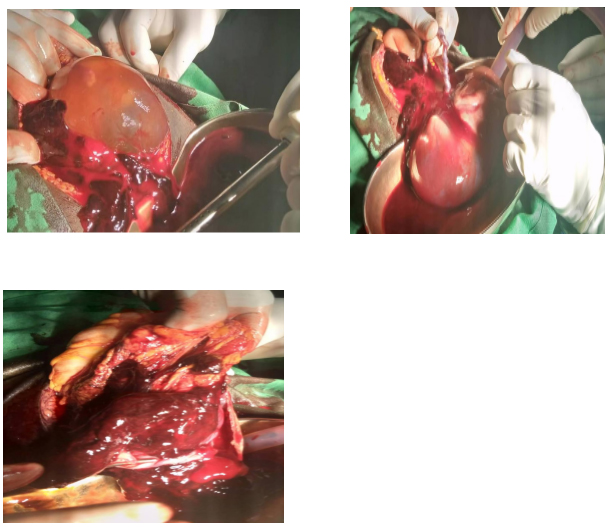
Figure 2: A-C. Intraoperative findings showing intact gestational sac (A), fetus within the sac extruded into the kidney dish with intact umbilical cord (B), and massive hemoperitoneum (C).
Discussion
Abdominal pregnancy is exceedingly rare. It is a type of extrauterine pregnancy where implantation of the fertilized ovum occurs in the abdominal cavity referred to as primary or secondary abdominal pregnancy occurs following re-implantation of an aborted or ruptured tubal pregnancy, the latter is the commoner of the two types [2]. It is often difficult to establish whether the abdominal pregnancy is primary or secondary.
In a review at the Komfo Anokye Teaching Hospital, Ghana, Opare-Addo et al reported an incidence of 1:1320 deliveries Whilst Amirtha et al. cited 1:25000 deliveries in India [3,4]. The reported incidences of maternal and perinatal mortality are, respectively, 0.5-8% and 45-90% [5].
The diagnosis of abdominal pregnancy requires vigilance from the obstetrician and sonographer. The high index of suspicion on the part of the obstetrician in the index case led to the diagnosis. The presenting complaint, the history and subsequent physical examination are often inconclusive and often more so when there is a history of attempted abortion in the index case.
Although there may be great variability in symptoms, they may present with severe lower abdominal painful fetal movements, vaginal bleeding, and varying degrees of anaemia, however, the commonest symptom is lower abdominal pain as seen in the index case [2]. Some patients may present with persistent gastrointestinal symptoms.
However, the risk factors for abdominal pregnancy are the same as those for tubal pregnancy. The recent use of progesterone-only pills and intrauterine devices with a history of surgery, pelvic inflammatory disease, and sexually transmitted disease, increases the risk of ectopic pregnancy [2].
It is a diagnostic challenge with ~ 55% missed during the antenatal period [6]. The index case was missed in the first trimester. Missed cases portends life-threatening complications.
Ultrasonography remains the imaging modality of choice world-wide and more so in low-resource countries, however, in equivocal cases Magnetic resonance imaging is used to resolve the diagnosis. Ultrasound scan is cheap and readily available, however operator dependent, and often leads to missed diagnosis. MRI is an expensive, long procedure time, and not readily available. MRI is contraindicated in patients with surgical implants, pace makers and patients who are claustrophobic [2]. In low resource settings, MRI is not readily available and hence ultrasonography remains the most readily accessible and affordable imaging modality to aid diagnosis. In the first trimester, both transvaginal and transabdominal ultrasound scan remains the first-line tool for diagnosis. MRI can help define the extent of abdominal and pelvic organ invasion by the placental tissue if not contraindicated [2]. Ultrasound scan features of abdominal pregnancy include an empty uterus, fetal parts close to the anterior abdominal wall, absent or near absent amniotic fluid around the fetus.
Termination of abdominal pregnancy is indicated when the pregnancy threatens the life of the mother due to its attachment to vital organs and the presence of hemoperitoneum. The clinical picture of deteriorating vital signs and the ultrasound findings of significant intraperitoneal fluid were life-threatening in the index case. Intraoperatively, there was an extra uterine fetus in the gestational sac at the superior aspect of the uterus with massive hemoperitoneum. About 4L of blood was evacuated from the peritoneal cavity. The placenta was attached to the right ovary, omentum, and fimbriae of the right fallopian tube. These features were consistent with preoperative ultrasound scan findings.
The management of the placenta depends on the attachment to vital organs. Because the abdominal organs lack the ability to contract and prevent bleeding, it is generally recommended to leave the placenta insitu and allow the natural process of regression and follow-up on ultrasound scan and human chorionic gonadotropin levels 7. In the index case, the placenta was easily removed and hemostasis secured. She was transfused with 4 units of whole blood and her postoperative condition was satisfactory.
Conclusion
Pre-operative diagnosis of abdominal pregnancy requires a high index of suspicion, thorough clinical and imaging assessment. This allows prompt diagnosis to safe mother in the early stages. Patients with amenorrhea with persistent abdominal pain and ultrasound assessment of an empty uterus should raise the suspicion of abdominal pregnancy. Ultrasound scan is routinely used to make the diagnosis even though MRI may be helpful. The decision to keep the pregnancy or intervene depends on the presence or absence of life-threatening complications such as hemorrhage. Fetal anomalies are common with term fetuses and counselling must be in depth to allow the woman make an informed decision in keeping or terminating the pregnancy.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Authors’ Contributions
JBB, EAI, MKA, JEM, AS, LNT and BD contributed equally to the concept, clinical management of the patient, writing of the paper, manuscript review and editing. All authors approved the final version.
Availability of Data
All relevant data are provided in the manuscript.
Funding
None
Reference
- Worley KC, Hnat MD, Cunningham FG (2008) Advanced extrauterine pregnancy: diagnostic and therapeutic challenges. Am J Obstet Gynecol 198: 1-7.
- Gurjar R (2018) Full-Term Live Secondary Abdominal Pregnancy?: A Rare Case Report. J Obstet Gynecol India 69: 36-39.
- Opare-Addo HS DS (2000) Advanced abdominal pregnancy: a study of 13 consecutive cases seen in 1993 and 1994 at Komfo Anokye Teaching Hospital, Kumasi, Ghana. Afr J Reprod Heal 4: 28-39.
- Amritha B, Sumangali T, Priya B, Deepak S, Sharadha R (2009) A rare case of term viable secondary abdominal pregnancy following rupture of a rudimentary horn: A case report. J Med Case Rep 3: 1-3.
- Martin JN Jr, Sessums JK, Martin RW, Pryor JA M (1988) Abdominal pregnancy: current concepts of management. JC Obs Gynecol 71: 549-557.
- Dahab AA, Aburass R SW (2011) Full-term extrauterine abdominal pregnancy:a case report. J Med Case Rep 5: 531.
- Jianping Z, Fen L QS (2008) Full-Term Abdominal Pregnancy. A Case Report and Review of the Literature. Gynecol Obs Invest 65: 139-141.
Citation: Bashiru JB, Idun EA, Amedi MK, Mozu JE, Saine A, et al. (2021) Second trimester Abdominal Pregnancy: A Case Report in a Resource Limited Setting. J Clin Stud Med Case Rep 8: 0125.
Copyright: © 2021 Jimah B Bashiru, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.