Self Medication and its Pattern among Patients Attending the General Outpatient Clinic of a Tertiary Institution in Abakaliki, Ebonyi State, Nigeria
*Corresponding Author(s):
Chihurumnanya AloDepartment Of Community Medicine, Federal Teaching Hospital Abakaliki, Ebonyi State, Nigeria
Tel:+23 48036777800,
Email:chihurumnanyalo@gmail.com
Abstract
Background: Self medication is the practice of taking medicines by individuals to treat self recognised symptoms or illness without the prescription of a health practitioner.
Objectives: This study seeks to assess the frequency, pattern of self medication, and the different forms of medications used by patients who attend the outpatient clinic of a tertiary hospital.
Methods: This was a cross-sectional study that lasted for three months. The respondents were selected using systematic random sampling. A pretested semi-structured interviewer administered questionnaire was used to collect information from the respondents. The data was analyzed using Epi info version 7 and significance level was set at P < 0.05.
Results: The study involved 398 patients with mean age and standard deviation of 37.18±14.9. Males were 161 (40.45%) and females were 237 (59.55%). The frequency of self medication was 375 (89.70%) and those who live in the urban areas were about twice more likely to practice self medication than rural dwellers. The medicines used for self medication include multivitamins (99.5%), antimalarials (79.15%), analgesics (66.33%), and antibiotics (46.98%).
Conclusion: Self medication practice was high among our respondents, rural dwellers were more likely to practice self medication than urban dwellers and the drugs commonly used for self medication include multivitamins, analgesics, antimalarials and antibiotics.
Keywords
INTRODUCTION
Self medication by definition is the practice of taking medicines by individuals to treat self recognised symptoms or illness [1] without the prescription of a health practitioner. It has been shown that in developing communities, self medication is a very common practice [2]. Self medication is different from responsible self medication which is the practice whereby individuals treat their ailments and conditions with medicines which are approved and available without prescription, and which are safe and effective when used as directed [1]. This entails that the medicines used must be of proven safety, quality and efficacy and that they are those indicated for conditions that can be recognised by self or used for some chronic or recurrent conditions. This must also follow initial medical diagnosis. In all cases, these medicines should be specifically designed for the purpose, and will require appropriate dose and dosage forms [1]. However, there is the potential for misuse and abuse of such medicines. It is important that self medication is made responsible and that it is undertaken only when it is safe and advisable to do so by qualified medical personnel. Self medication that is not responsible is practiced in varying degrees in different communities. A study done in a hospital in a Nigerian community showed that 85% of patients admitted to self medication [3]. Same study also revealed that drugs were used singly or in combination and some of their results showed that (15.3%) of respondents admitted using antimalaria-analgesic-antibiotic combination and (10.0%) admitted using antibiotic-analgesic combinations. It is important to note that heavy reliance is made on analgesics as well as on other over the counter medicines [3]. The prolonged use of these medicines has long been associated with chronic renal failure [4]. The use of Over the Counter (OTC) analgesics is widespread and the potential impact of these drugs on the development of chronic renal failure may be significant [4]. It is also possible that, consumers may be unaware that several products sold with different brand names and for different indications may contain the same active ingredients. Though self medication as part of self care has advantages for the patients and health care, it is supposed to be responsible and safe.
A major problem of self medication with antimicrobials is the emergence of human pathogens resistance worldwide particularly in developing countries, where antibiotics are often available without a prescription [2]. In our environment regulation of prescription drugs is seen to be relaxed and the magnitude of use of prescription medicine and other forms of medication such as traditional medicines and herbal concoction is not known. This study seeks to assess the prevalence and pattern of self medication, and the different forms of medications utilised by patients who attend the General Outpatient Department of the Federal Teaching Hospital Abakaliki.
METHODOLOGY
This was a cross-sectional study carried out in a tertiary hospital that offers primary, secondary and tertiary care. The hospital is government owned and is purely orthodox; not offering any alternative medicine services and has no religious inclination. The primary care services are offered through the General Out Patient Department (GOPD) of the hospital. The hospital serves communities in Ebonyi State and its environs. The GOPD takes care of adult patients only because the hospital also has a paediatrics department. Adult population aged 15 years and above who attend the general outpatient clinic of the hospital was the target of this study. The sample size was calculated using the formula for calculating samples size when the population is greater than 10,000 (N = Z2pq/d2). The calculated sample size was 404 but 398 questionnaires were completely and correctly returned for analysis. The sampling method used for selection was systematic random sampling method. The GOPD is visited daily by an average of 150 patients. Thus we expected 13,500 patients during the study period of 3 months and as such giving a sampling interval of 33.41. Thus every 33rd patient was selected and if the patient consented, the patient was recruited into the study. Data was collected using a semi-structured, pre-tested, interviewer administered questionnaire. Information on demographic characteristics, family type, history of self medication, and drugs used for self medication was collected. The data was analysed using statistical software Epi Info 7. All statistical calculations are significant at P<0.05, and 95% confidence interval.
RESULTS
Three hundred and ninety eight patients participated in the study out of which 161 (40.45%) were males and 237 (59.55%) females. The mean age of respondents was 37.18±14.9. Urban dwellers were 245 (61.56%), while rural dwellers were 153 (38.44%). Most of the respondents had tertiary education (41.33%) and secondary education (40.31%). More than half were married (56.03%), 39.70% were single and 4.27% were widowed (Table 1). The frequency of self medication among the respondents was 375 (89.70%) (Table2). The number of females that practiced self medication was 207 (87.34%) while males were 150 (93.17%), but the difference among sex was not statistically significant, χ2 = 3.521, p = 0.0605. With respect to place of residence, those who live in urban areas that practice self medication (215) were more in number that rural dwellers (142). However, this difference was not statistically significant, χ2 = 2.6049, p = 0.1065 but the odds ratio was 1.8 (Table 1). Logistic regression modelling on age group was statistically significant indicating that age predicted between practising self medication and not (χ2 = 21.3062, P = 0.000). The results also showed that the patients practiced self medication with different types of drugs such as antibiotics, antimalarials, analgesics, antidiabetic, antihypertensives, cough syrups, antihelminthics and multivitamins. The group of drug with the highest frequency was multivitamins (99.5%), followed by antimalarials (79.15%), analgesics (66.33%), antibiotics (46.98%), while antidiabetics (0.75%) and antihypertensives (1.10%) were quite low (Figure 1).
| Self medication frequency (%) | ||||
| Yes | No | Total | Statistics | |
| Age group | Logistic regression | |||
| 17-40 (Young adult) | 208 (84.21) | 39 (15.79) | 247 (100) | Model χ2 = 21.3062 |
| 41- 64 (Middle age) | 114 (998.24) | 2 (1.72) | 116 (100) | Df = 2 |
| 65-82 (Old age) | 35 (100) | 0 (100) | 35 (100) | P= 0.0000 |
| Total | 357 (89.7) | 41 (10.30) | 398 (100) | |
| Mean (Standard deviation) | ||||
|
Mean age (standard deviation) |
37.18 (14.9) | |||
| Self medication | ||||
| Sex | Yes | No | Total | Chi-Squared test |
| Males | 150 (93.17) | 11 (6.83) | 161 (100) |
χ2 = 3.521, p = 0.0605 |
| Females | 207 (87.34) | 30 (12.66) | 237 (100) | |
| Total | 357 (89.70) | 41 (10.30) | 398 (100) | |
| Place of residence | Yes | No | ||
| Rural | 142 (92.81) | 11 (7.19) | 153 (100) | χ2 = 2.6049, p = 0.1065 |
| Urban | 215 (87.76) | 30 (12.24) | 245 (100) | OR = 1.80 |
| Total | 357 (89.70) | 41 (10.30) | 398 (100) | |
| Marital status | Logistic regression | |||
| Single | 128 (81.01) | 30 (11.99) | 158 (100) | Model χ2 = 21.8087 |
| Married | 212 (95.07) | 11 (4.93) | 223 (100) | Df = 2 |
| Widowed | 17 (100) | 0 (0) | 17 (100) | P = 0.0000 |
| Total | 357 (89.70) | 41 (10.30) | 398 (100) | |
| Educational level | ||||
| None | 20 (100) | 0 (0) | 20 (100) | Model χ2 = 5.6188 |
| Primary | 50 (96.15) | 2 (3.85) | 52 (100) | Df = 3 |
| Secondary | 141 (88.13) | 19 (11.88) | 160 (100) | P = 0.1317 |
| Tertiary | 146 (87.95) | 20 (12.05) | 166 (100) | |
| Total | 357 (89.70) | 41 (10.30) | 398 (100) | |
Table 1: Shows demographic characteristics of respondents and their relationship with self medication.
| Class of drug | ||||
| Antimalarial | Total | Statistics | ||
| Place of residence | Yes | No | ||
| Rural | 134 | 19 | 153 |
χ2 = 10.7165 P = 0.0010 |
| Urban | 181 | 64 | 245 | |
| Total | 315 | 83 | 398 | |
| Analgesics | ||||
| Yes | No | |||
| Age group |
Corrected Chi-squared |
|||
| Young | 141 | 106 | 247 |
χ2 = 25.9531 P = 0.0000 |
| Middle age | 91 | 25 | 116 | |
| Old age | 32 | 3 | 35 | |
| Total | 264 | 134 | 398 | |
| Sex | ||||
| Female | 142 | 95 | 237 |
χ2 = 10.7994 P = 0.0010 |
| Male | 122 | 39 | 161 | |
| Total | 264 | 134 | 398 | |
| Educational status | Corrected Chi-squared | |||
| None | 17 | 3 | 20 |
χ2 = 12.6048 p = 0.0035 |
| Primary | 39 | 13 | 52 | |
| Secondary | 114 | 46 | 160 | |
| Tertiary | 94 | 72 | 166 | |
| Total | 264 | 134 | 398 | |
| Place of residence | ||||
| Urban | 143 | 102 | 245 |
χ2 = 18.1014 p = 0.0000 |
| Rural | 121 | 32 | 153 | |
| Total | 264 | 134 | 398 | |
| Antibiotics | ||||
| Sex | ||||
| Female | 99 | 138 | 237 |
χ2 = 6.3912 P = 0.0114 |
| Male | 88 | 73 | 161 | |
| Total | 187 | 211 | 398 | |
Table 2: Shows demographic characteristics and relationship with class of self medicated drug.
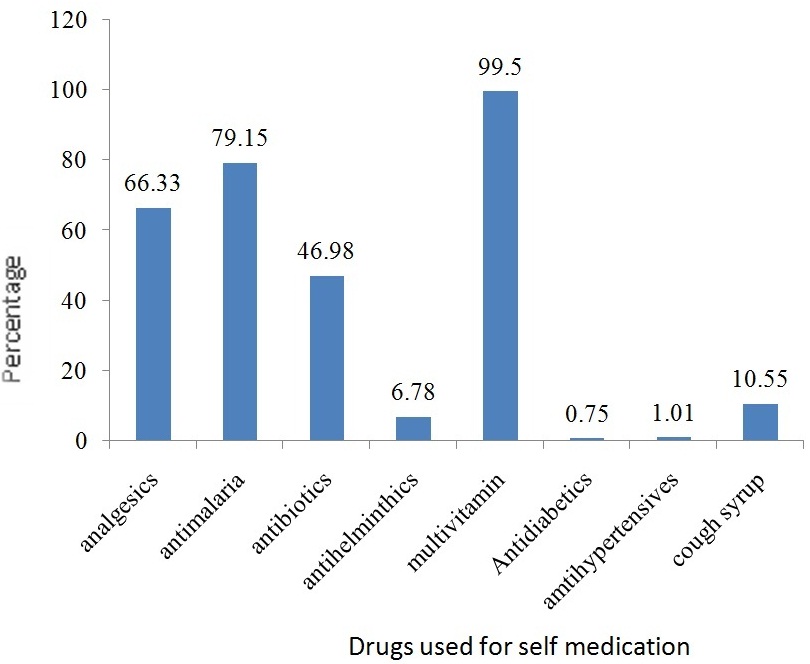 Figure 1: Bar chart showing frequency of drugs used for self medication.
Figure 1: Bar chart showing frequency of drugs used for self medication.
The results of statistical analysis concerning the demographic characteristics as they relate to the different drugs used for self medication are shown in table 2. Only statistically significant results have been shown. It shows that with anti malarial use, there was a significant difference between self medication by urban dwellers and rural dwellers (χ2 = 10.7165, P = 0.0010). On the use of analgesics, age, sex, educational status, and place of residence, all showed significant differences between practicing self medication with analgesics and not. However concerning antibiotics, the difference between its use for self medication among males and females was statistically significant (χ2 = 6.3912, P = 0.0114), table 2.
DISCUSSION
A great number of the respondents practiced self medication (89%). This result is similar to the study conducted by Omolase et al., where they got a frequency of 85% [3]. Other studies also revealed self medication frequency of 85% [5] and 87% [6] respectively. This shows that the practice of self medication is really high among patients. A possible explanation could be the availability of these drugs as over the counter drugs and so people easily walk up to the patent medicine dealers and purchase these drugs for perceived symptoms. In the face of a weak health system and poor health services, patients might have to resort to seeing a physician as the last course of action only when the patient feels the symptoms are getting out of hands. Another possible explanation could be that in the bid to cut the cost of seeking health care in an orthodox hospital, patients might just walk into a patent medicine dealer and explain the symptoms to them and they will be given medications to take and often times, the patient does not know the different constituents of the drugs being sold to them. Since our study was a hospital based study, one could assume that that it will lead to the high frequency of self medication because of the population being studied. However, Afolabi reported 85% among market women in Lagos [7], another cross-sectional study in Jos reported a prevalence of 75.4% [8], while another in Islamabad reported a lower frequency of 61.2% among urban and rural populations [9]. Therefore the prevalence from our study is not too different from what is obtainable from the general population. This high percentage of patients practicing self medication should be a source of worry to all especially clinicians, pharmacists and food and drug administration and control policy makers.
Our results showed that different age groups practiced self medication. A possible implication of this is that the young people who practice self medication may have unrestricted access to drugs and this may lead to misuse of drugs. Onajole et al., in their study found out that 71% of those who practiced self medication also admitted to drug misuse [10]. Hence leaving some of these medicines in the hands of young people may have consequences ranging from drug abuse to drug dependence and some adverse events that may be fatal. Self medication was also practiced among the elderly from our results. Another study also showed a significant self medication among the elderly and concluded that it was important that health care workers need to make their patients aware of the harmful effects of these medicines [11]. It has been shown that adverse events requiring hospitalisation occurred as a result of self medication and these occurred amongst men and women aged 60-79 years of age [12]. The mean age of respondents in our study was about 37 years. This result is not too different from the results of a similar study done on Kano state, Northern Nigeria where the mean age was 35±15.10 years [5]. The study was a cross-sectional study among adult population with sample size as 380 [5]. The importance of these results is that it should suggest to clinicians to always assess the medications that patients have taken on their own in an attempt to treat their ailments before presenting to hospital. This will help them counsel patients properly on responsible drug use.
We contemplated that there could be a pattern of self medication that existed amongst the sociodemographic characteristics of our respondents. From the results it appeared that the proportion of females that practiced self medication was more than males, but this difference was not statistically significant χ2 = 3.521, p = 0.0605. Age and marital status were predictors of self medication, likewise place of residence where the rural dwellers were 1.8 times more likely to practice self medication more than those who live in urban areas. In our study, there appeared to be higher proportions of the educated more than uneducated but the educational level was not a good predictor of self medication. However, Afolabi found an association between marital status, and educational level with self medication [7]. Martin-Perez et al., found significant association of age with self medication among males but not females [13]. These associations help physicians in assessing the risk that a client sitting before them in the consulting room might be practicing self medication and therefore should be offered counselling for responsible drug use. These associations however should not make clinicians forget that the other sociodemographic variables where associations were not significant might also be important when assessing medication use among clients.
Multivitamins ranked highest among the group of medicines the respondents used for self medication. This was followed by antimalarial drugs, analgesics, and then antibiotics. This result is similar to the findings reported by Umar et al., [5], Lucas et al., [14], and Akanbi et al., [15]. Inappropriate use of antibiotics has led to the development of resistance to antimicrobials by so many microorganisms [16]. For this reason, WHO in 2011 made the theme of the World health day to be “Antimicrobial resistance: no action today, no cure tomorrow” with a six-point policy package which was published to help countries combat antibiotic resistance. It therefore follows that if indiscriminate use of antibiotics is not curtailed by concerted efforts from policy makers and health professionals, then antimicrobial resistance will continue to be a problem. This is also the case for antimalarials where resistance to P. falciparum has since emerged [16].
This study however has limitations. It was a cross sectional study that spanned only three months. This meant that the authors could not measure the trend of self medication over time among the respondents. The study did not also evaluate the impact of self medication on health such as adverse events following medication, overdosing, underdosing, and wrong prescriptions, etc. These are areas that have implications for further research. It will be important to policy makers to have evidenced based guidance in making decisions on which drugs should be over the counter or which drugs must be purchased only on a current prescription by qualified medical personnel and also evidence that will help draw up programmes that can educate people well on responsible self medication. The factors that lead to self medication need to be studied. This would give a clue to interventions that can be put in place to ensure that patients practice responsible self medication and not put their health in harm’s way.
CONCLUSION
Self medication prevalence was high among our respondents, urban dwellers were more likely to practice self medication than rural dwellers and the drugs commonly used for self medication include multivitamins, analgesics, antimalarials and antibiotics. Self medication on these drugs can be predicted by age, sex, educational status and place of residence.
REFERENCES
- World Health Organisation (1998) The Role of the pharmacist in self-care and self-medication: report of the 4th WHO Consultative Group on the Role of the Pharmacist, The Hague, Netherlands. World Health Organization, Geneva, Switzerland.
- Jain S, Malvin R, Purviya JK (2011) Concept of Self Medication: A review. International Journal of Pharmaceuticals and biological archives 2: 831- 836.
- Omolase CO, Adeleke OE, Afolabi AO, Afolabi OT (2007) Self medication amongst general outpatients in a nigerian community hospital. Ann Ib Postgrad Med 5: 64-67.
- A World Health Organization resource (2000) WHO Drug Information. World Health Organisation, Geneva, Switzerland. 14: 01-81.
- Lawan UM, Abubakar IS, Jibo AM, Rufai A (2013) Pattern, awareness and perceptions of health hazards associated with self medication among adult residents of kano metropolis, northwestern Nigeria. Indian J Community Med 38: 144-151.
- Al-Ramahi R (2013) Patterns and attitudes of self-medication practices and possible role of community pharmacists in Palestine. Int J Clin Pharmacol Ther 51: 562-567.
- Afolabi AO (2008) Factors influencing the pattern of self-medication in an adult Nigerian population. Ann Afr Med 7: 120-127.
- Auta A, Omale S, Folorunsho TJ, David S, Banwat SB (2012) Medicine Vendors: Self-medication Practices and Medicine Knowledge. N Am J Med Sci 4: 24-28.
- Aqeel T, Shabbir A, Basharat H, Bukhari M, Mobin S, et al. (2014) Prevalence of Self-Medication among Urban and Rural Population of Islamabad, Pakistan. Tropical Journal of Pharmaceutical Research 13: 627-633.
- Onajole AT, Bamgbala AO (2004) Socio-Demographic characteristics of drug misuse in a Polytechnic in Lagos, Nigeria. Nig Jnl Health and Biomed Sciences 3: 40-43.
- Vacas Rodilla E, Castellà Dagà I, Sánchez Giralt M, Pujol Algué A, Pallarés Comalada MC, et al. (2009) [Self-medication and the elderly. The reality of the home medicine cabinet]. Aten Primaria 41: 269-274.
- Schmiedl S, Rottenkolber M, Hasford J, Rottenkolber D, Farker K, et al. (2014) Self-medication with over-the-counter and prescribed drugs causing adverse-drug-reaction-related hospital admissions: results of a prospective, long-term multi-centre study. Drug Saf 37: 225-235.
- Martín-Pérez M, Hernández BV, López de Andrés A, Jiménez-Trujillo I, Jiménez-García R, et al. (2015) Predictors of medication use in the Roma population in Spain: a population-based national study. Public Health 129: 453-459.
- Lucas R, Lunet N, Carvalho R, Langa J, Muanantatha M, et al. (2007) Patterns in the use of medicines by university students in Maputo, Mozambique. Cad Saude Publica 23: 2845-2852.
- Akanbi OM, Odaibo AB, Afolabi KA, Ademowo OG (2005) Effect of self-medication with antimalarial drugs on malaria infection in pregnant women in South-Western Nigeria. Med Princ Pract 14: 6-9.
- WHO Media centre (2015) Antimicrobial resistance. World Health Organization, Geneva, Switzerland.
Citation: Alo C, Oguejiofor NC, Alo NC (2015) Self Medication and its Pattern among Patients Attending the General Outpatient Clinic of a Tertiary Institution in Abakaliki, Ebonyi State, Nigeria. J Community Med Public Health Care 2: 008.
Copyright: © 2015 Chihurumnanya Alo, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.