Shaken Baby Syndrome – Medico-Legal Approach of a Clinical Case
*Corresponding Author(s):
Ricardo Pereira MendonçaResident Of Legal Medicine, National Institute Of Legal Medicine And Forensic Sciences, Polo Das Ciências De Saúde (Polo III), Azinhaga De Santa Comba, 3000-548 Coimbra, Portugal
Email:ricardo.j.mendonca@inmlcf.mj.pt
Abstract
Shaken Baby Syndrome occurs in a context of non-accidental injury when a child is shaken violently, originating acceleration-deceleration phenomena of the brain, which usually cause subdural and retinal hemorrhages, as well as encephalopathy.
The authors approach, from a medico-legal point of view, the case of a latent patient assisted in the emergency room with a suspected clinical and imaging representation of Shaken Baby Syndrome, focusing on: the injury mechanisms underlying its genesis; the compatibility between the clinical findings of the complementary diagnostic tests and the history provided by the caregivers, and the importance of differential and exclusion diagnoses. The combination of all these elements allows the medical expert to pronounce on the compatibility of the injury condition with the shaken child syndrome, the existence of danger to life and the need for neuropsychological reassessment, deferred over time, to determine any sequelae.
Keywords
Child abuse; Medico-legal Medicine; Shaken baby syndrome; Trauma
Introduction
Physical abuse in children manifests itself essentially as skin and skeletal injuries, with organic injuries being less frequent, including brain injuries [1].
Shaken baby syndrome (SBA) is characterized by brain acceleration-deceleration phenomena [2], producing acute traumatic injuries (subdural and retinal hemorrhage), which can progress to brain edema and/or encephalopathy [3]. It occurs in 14–33.8/100 000 children in the first year of age and often leads to cognitive and developmental, ophthalmological changes or even death (25% in the days following the injury), with less than 35% recovering without any sequelae2. It is more prevalent in male under one year of age, children of young parents, with low socioeconomic status and family instability [3].
This case study intends to highlight and analyze the particularities of this syndrome and discuss the possible causes of injury to be excluded from the Medico-Legal point of view.
Clinical Case
The present case refers to an infant aged 8 months and 24 days, submitted to a medical-legal examination in the Scope of Urgent Acts, for suspected child abuse.
On the day of the event, the babysitter mentioned hearing the child crying, finding him hypotonic and with an eye deviation, having called health care. Upon admission to the Emergency Department, he presented with eye deviation to the left, with tonic-clonic movements, vomiting, irritability, fluctuating state of consciousness, with no traumatic skin lesions. Cranioencephalic computed tomography (CT-CE) and cranioencephalic nuclear magnetic resonance (NMR-CE) were performed, which revealed the presence of subdural hemorrhages (HSD) in different locations and stages, subarachnoid hemorrhage (SAH) and left parietal vein thrombosis. (Figure 1). He was evaluated by Ophthalmology and was diagnosed with extensive pre-retinal and bilateral retinal hemorrhages (RH). As he showed signs of intracranial hypertension, he was admitted to the Intensive Care, where he underwent medical treatment, requiring intubation for 2 days. His evolution was favorable during hospitalization, with coagulation and metabolic studies without changes.
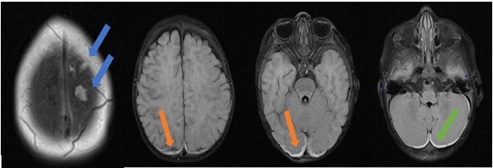 Figure 1: Subdural blood collections: several clots in the high left convexity (blue arrows); supratentorial (orange arrows) and infratentorial (green arrow)
Figure 1: Subdural blood collections: several clots in the high left convexity (blue arrows); supratentorial (orange arrows) and infratentorial (green arrow)
He was a healthy child, with no known personal or family history. The mother denied any known accidental trauma or similar episodes in the past, moreover, the babysitter also did not mention any traumatic event. The infant had been with the babysitter for about 1 month, and he was sleeping in a bed without rails while she was taking care of 6 other older children. The child stayed only with his parents or with the babysitter.
In our physical examination, performed 8 days after the day of the event, the infant showed no signs of recent or old traumatic lesions on the skin surface or any apparent motor development deficit.
Discussion
Naturally occurring SAH are uncommon in children and may, however, originate from vascular malformations, namely aneurysms, which were excluded in the imaging study [4]. The clinical and analytical evaluation allowed to exclude the existence of natural diseases that could be in its genesis or could contribute to it, namely metabolic, coagulopathic and/or hematological. On the other hand, the most common cause of SAH is undoubtedly traumatic [5].
In the formation of HSD are involved mechanisms related to rapid acceleration/deceleration and rotation movements that lead to shearing of communicating veins of the convexity of the cerebral hemispheres [6]. These
rapid and short duration movements tend to be produced by severe high-intensity trauma, and the hemorrhage may be secondary to cerebral contusion or result from direct trauma to the skull [7,8].
Regarding the appearance of RH, the child had extensive and bilateral hemorrhage and pre-retinal hemorrhages, whose traumatic origin is highly suggestive, with a sensitivity of 75% and specificity of 93.2% for the diagnosis of child abuse [9].
In the present case, it was unlikely that it was a natural disease, due to the fact that not only was the child healthy but also had regular medical follow-up.
The absence of cutaneous, bone (namely linear fractures of the skull, isolated or associated with long bones, or even complex or depressed skull fractures) and specific meningoencephalic lesions, in particular epidural hematomas, focal subarachnoid hemorrhage or small contusions in the brain parenchyma [7,8] rule out the possibility of falls or high-speed impacts, as reported by the mother.
In the absence of other probable etiologies and in the presence of severe traumatic head injuries, the presented situation is suggestive of abuse [9]. The clinical picture shown compatible with SBA, resulting a situation of repeated child abuse, taking into account the result of the MRI- EC.
The infant brain is highly susceptible to serious injury due to several factors, including disproportionate size of the head, weak neck musculature, elasticity of the skull, presence of open sutures, large subarachnoid space, high brain water contente and the fragility of the communicating veins involved in subdural and subarachnoid hemorrhages [8].
Initial symptoms may be obscured by late seeking medical help, the most common are loss of or altered state of consciousness, vomiting, apnea and seizures [8].
At the time of the forensic evaluation, the infant did not present neuromotor changes. However, about 70% of victims may manifest neurological sequelae such as cognitive, motor, linguistic and behavioral disabilities, which may even appear years later [10], which is why neuropsychological reassessment was suggested at 6 and 12 years of age. It was considered the existence of danger to the examinee's life due to the cranial hypertension.
The suspicion of SBA requires a multidisciplinary, cautious and thorough approach, the conclusions of which must be scientifically based, given the consequences for all those involved in the scope of the Criminal Law Code.
References
- Ermertcan AT, Ertan P (2010) Skin manifestations of child abuse. Indian J Dermatol Venereol Leprol 76: 317-326.
- Tasar MA, Sahin F, Polat S, Ilhan M, Çamurdan A, et al. (2014) Long-term outcomes of the shaken baby syndrome prevention program: Turkey's experience. Turk Pediatri Ars 49: 203-209.
- Tariq SM, Haider SA, Hussain A (2018) Shaken Baby Syndrome: A preventable calamity. J Pak Med Assoc 68: 982-983.
- Ziu E, Mesfin FB (2021) Subarachnoid Hemorrhage. Treasure Island (FL): StatPearls Publishing PMID: 28722987.
- McDonald KC (2007) Child abuse: approach and management. Am Fam Physician 75: 221-228.
- Nooraudah AR, Mohd Sham K, Zahari N, Fauziah K (2004) Non-accidental fatal head injury in small children--a clinico-pathological correlation. Med J Malaysia 59: 160-165.
- Gabaeff SC (2011) Challenging the Pathophysiologic Connection between Subdural Hematoma, Retinal Hemorrhage and Shaken Baby Syndrome. West J Emerg Med 12: 144-158.
- Hung KL (2020) Pediatric abusive head trauma. Biomed J 43: 240-250.
- Karibe H, Kameyama M, Hayashi T, Narisawa A, Tominaga T (2016) Acute Subdural Hematoma in Infants with Abusive Head Trauma: A Literature Review. Neurol Med Chir (Tokyo) 56: 264-273.
- Lee WJ, Lim YC, Yoon SH (2020) Abusive Head Traumas in 4 Infants. Korean J Neurotrauma 16: 246-253.
Citation: Mendonça RP, Tavares S, Costa M (2023) Shaken Baby Syndrome – Medico-Legal Approach of a Clinical Case. J Med Stud Res 5: 025.
Copyright: © 2023 Ricardo Pereira Mendonça, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.