
Significant Efficacy of Traditional Chinese Medicine and Herbal Treatment on Chronic Seborrheic Dermatitis: A Case Report
*Corresponding Author(s):
Fu-Shih ChenGraduate School Of Pharmaceutical Sciences, Nihon Pharmaceutical University, Tokyo, Japan
Tel:+81 9048439386,
Email:fukushichen@gmail.com
Abstract
This case report presents a 27-year-old female who has been suffering from Seborrheic Dermatitis (SD) since the age of 12. After years of ineffective treatment with Western medicine, she turned to traditional Chinese medicine and achieved significant improvement. Upon initial examination in traditional Chinese medicine, her scalp and face were severely affected, exhibiting symptoms such as erythema, desquamation, hyperkeratosis, and skin atrophy, along with telangiectasia. The treatment included oral administration of traditional Chinese medicine and the topical application of Chinese herbal gel. The primary components consisted of Yin Chen Hao Tang (Virgate Wormwood Decoction), Ma Xing Gan Shi Tang (Ephedra, Apricot Kernel, Licorice and Gypsum Decoction), along with the external application of Qing Dai (Indigo Naturalis) gel. After three weeks of treatment, there was a significant reduction in the lesions on the scalp and face, with substantial improvement in symptoms. This case highlights the potential of traditional Chinese herbal medicine in treating SD, especially in instances where conventional Western medicine has been ineffective.
Introduction
In adults, SD is a chronic skin disease, that affects adults and is commonly associated with stress or sleep-related factors. It presents as mild to moderate erythema, popular, exudative, or scaly lesions, and is most prevalent on the face and scalp [1]. SD shares similarities with scalp psoriasis, but psoriasis lesions are characterized by clearly demarcated, thickened plaques accompanied by dry, white scales [2]. SD can affect both men and women, typically starting after puberty. While it is not a life-threatening condition, it may cause adverse psychological and social effects and may also predispose patients to acne [3].
The complete and detailed pathogenesis of SD needs to be fully understood, and the preferred medications for mild to moderate SD are primarily topical. The most effective among these include antifungals, corticosteroids, and immunomodulators. Systemic drugs may be employed for severe and refractory SD [4]. Due to concerns about the effectiveness and potential side effects, there is often an increasing demand for alternative treatments and therapies based on herbs/plants [5]. This case presents a female who had been struggling with Seborrheic Dermatitis for 15 years. After trying several ineffective treatments, she turned to traditional Chinese medicine and herbal therapy and experienced significant improvement.
Case Report
The case of a 27-year-old female suffering from SD since the age of 12 presents a challenge to medical professionals due to the lack of improvement and a trend towards worsening over the years, despite medical consultations. To find a viable solution, the patient sought treatment at a traditional Chinese medicine clinic in Taiwan, and the initial consultation took place on January 27, 2024. The condition primarily affects the scalp, forehead, and behind the ears, with erythematous papules, keratotic thickening, and desquamation. The prolonged use of topical steroid creams has resulted in cutaneous atrophy and thinning, telangiectasia, erythema, and even bleeding on the scalp. Furthermore, the patient exhibits severe pruritus, leading to disrupted sleep patterns, impaired sweat gland function, and constipation, with infrequent bowel movements occurring only twice per week. SD doesn't have a standardized system for grading its severity that is universally accepted [6]. According to the Seborrheic Dermatitis Area and Severity Index (SEDASI), facial SD severity is scored [6], it is important to note that the skin lesions on the scalp require separate attention. The affected area of the scalp is 100%, with telangiectasia, erythema, thickened scales shedding, and extreme itching (Figure 1). The SEDASI score on the face is 24, indicating a moderate severity of SD (Figure 2).
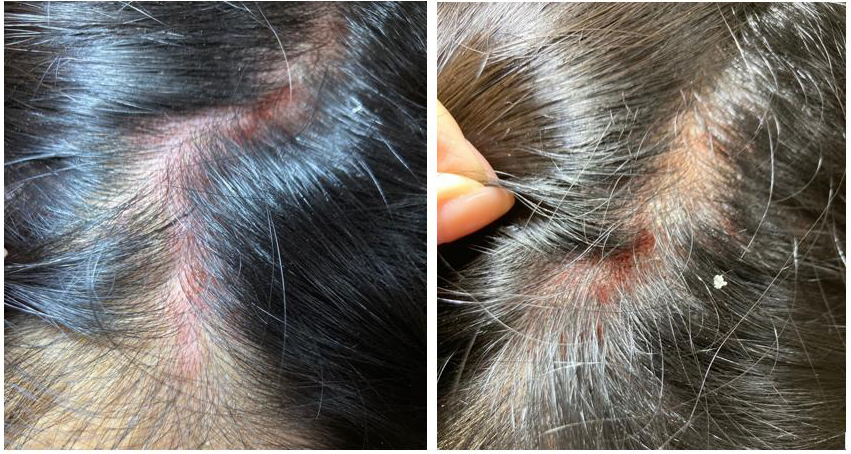
Figure1: January 27, 2024: The scalp area affected was 100%. Multiple and clustered plaques were observed upon parting the hair from various angles, with moderate to severe erythema. Significant flaking with large, thickened scales, and notable skin atrophy and thinning was significant. Microvascular dilation and reddening were present, and there was even bleeding of the scalp.
 Figure 2: January 27, 2024: The Seborrheic Dermatitis lesions on the facial forehead and near the ears were evaluated using the SEDASI score, amounting to 24 points, corresponding to moderate SD.
Figure 2: January 27, 2024: The Seborrheic Dermatitis lesions on the facial forehead and near the ears were evaluated using the SEDASI score, amounting to 24 points, corresponding to moderate SD.
On January 27, 2024, a treatment plan was prescribed as follows: a daily intake of traditional Chinese medicine powder made by CHUANG SONG ZONG PHARMACEUTICAL CO., LTD. The prescribed dosage includes Yin Chen Hao Tang (Virgate Wormwood Decoction) 10g, Ma Xing Gan Shi Tang (Ephedra, Apricot Kernel, Licorice and Gypsum Decoction) 10g, Dandelion (Taraxacum officinale) 5g, Ji Xue Teng (Spatholobus suberectus) 3g, and Indigo Leaf (Isatis indigotica) 2g. This medication should be taken once in the morning and once in the evening, and a one-week supply is prescribed. Additionally, Chinese herbal gel, Qing Dai (Indigo Naturalis), should be applied twice daily on localized SD lesions using approximately 1 gram per 100 square centimeters (Figures 3 & 4).
 Figure 3: February 16, 2024: The scalp area affected was reduced to 10%. Upon parting the hair from various angles, the plaques had disappeared, leaving only minor redness in certain areas.
Figure 3: February 16, 2024: The scalp area affected was reduced to 10%. Upon parting the hair from various angles, the plaques had disappeared, leaving only minor redness in certain areas.
 Figure 4: February 16, 2024: The Seborrheic Dermatitis lesions on the facial forehead and near the ears exhibited mild erythema and desquamation. According to the SEDASI score, the condition was assessed as 10 points, corresponding to mild SD.s
Figure 4: February 16, 2024: The Seborrheic Dermatitis lesions on the facial forehead and near the ears exhibited mild erythema and desquamation. According to the SEDASI score, the condition was assessed as 10 points, corresponding to mild SD.s
On the follow-up visit on February 16, 2024, there was a significant reduction in the extent of the scalp skin rash, and there were no visible plaques or desquamation remaining. The patient continued taking the same Chinese medicines, and the scalp had almost completely healed. Please refer to table 1 for more information.
|
Date |
January 27 |
February 16 |
|
Plaque Presentation |
Large and coalescing plaques |
No visible plaques |
|
Erythema Intensity |
Intense redness |
Light pink |
|
Desquamation Level |
Large, thickened scales |
None |
|
Percentage of Scalp Affected |
100% of scalp involved |
10% of scalp involved |
|
Itching Severity (Patient self-assessment of itching sensation, with 10 being intolerably itchy and 0 being not itchy at all) |
10 |
0 |
Table 1: Detailed Description of Scalp SD Lesion Presentation Before and After Treatment.
Discussion
SD is a skin condition typically occurring in areas of the body with a high concentration of sebaceous glands, such as the face, chest, and scalp. SD is also considered one of the causes of hair loss. The condition is characterized by age, sex, increased sebaceous gland activity, immunodeficiency, neurological and psychiatric disorders, use of certain medications, and low humidity or environmental temperatures. The prevalence in the general population is 1-3%, whereas it ranges from 34-83% among individuals with compromised immune systems [2]. Treatment options for SD include antifungal, anti-inflammatory, keratolytic, and coal tar therapies. Concerns exist regarding poor adherence, resistance, and some side effects for medications that have been used to treat SD [7]. These side effects include telangiectasia, hypertrichosis, skin atrophy, and others. Therefore, long-term use of these medications is not recommended [8]. Consequently, numerous studies have shown the efficacy of natural plant-based therapies for treating SD [7]. Additionally, many dermatological patients are turning to complementary medicine for treatment assistance [3].
Herbal medicine practices have been developed regionally across China, Japan, Australia, and the Americas. Traditional Chinese Medicine (TCM) concentrates on the individual's overall condition rather than the specific ailment or disease they are experiencing. Diagnosis and treatment in TCM are based on a holistic view of the patient and their symptoms [9]. In this case, the approach focuses on facilitating the patient's excretion of skin toxins through sweat, which improves symptoms of skin inflammation caused by difficulty with perspiration. [10]. In the compound traditional Chinese medicine formula, Ma Xing Gan Shi Tang, the ingredient Ephedra promotes sweating [11], Gypsum has anti-inflammatory effects [12], and Licorice acts as a natural anti-inflammatory agent [13]. Therefore, within the entire Ma Xing Gan Shi Tang formula, there is a simultaneous achievement of inducing sweating and alleviating SD skin inflammation. Research indicates that normal gastrointestinal function is crucial for maintaining overall health, and there is a strong association between gastrointestinal dysfunction and seborrheic conditions [3]. In this case, the patient with constipation symptoms completely resolved the issue after using the traditional Chinese medicine Virgate Wormwood Decoction (Yin Chen Hao Tang) [14]. After the normalization of gastrointestinal function, the dermatitis also improved. Furthermore, Indigo Leaf (Isatis indigotica) and Dandelion (Taraxacum officinale), due to their antipyretic and detoxifying effects, are used in the treatment of dermatitis [15]. Ji Xue Teng (Spatholobus suberectus) is also a commonly used traditional Chinese herbs in treating dermatitis [16].
In topical treatment, Qing Dai (Indigo Naturalis) its effects through several mechanisms: it regulates the proliferation and differentiation of keratinocytes, modulates the inflammatory response of the cell-mediated immune system, and ameliorates microvascular dilation and proliferation in skin lesions [17]. SD also presents issues ranging from erythema to popular, exudative, or squamous lesions. Consequently, in this case, a Qing Dai gel composed of 5% Qing Dai powder and 95% base (containing 5% Carbomer and 95% aloe vera gel) was utilized for the topical treatment of SD. The traditional Chinese pharmacy provided the gel in collaboration with our clinic. Aloe vera also offers benefits for treating SD [5].
TCM offers a significant healthcare service due to its cost-effectiveness, alleviation of concerns regarding the side effects of chemical (synthetic) drugs, and fulfilment of the desire for more personalized healthcare solutions [9]. TCM treatment focuses on alleviating symptoms and achieving sustained and stable therapeutic effects by regulating internal organ functions and improving overall constitution [18]. This treatment approach is based on a core concept: skin health directly reflects the balance of internal organs and the flow of energy within the body. Therefore, it emphasizes achieving therapeutic goals through comprehensive conditioning.
Conclusion
The case presented herein exemplifies a protracted 12-year history of chronic SD, a condition that proved refractory to standard Western medical and pharmacological treatments. A significant improvement was achieved by adopting TCM, topical treatments, and oral administration of Chinese herbal medicine. This highlights the potential of natural therapies, such as herbal medicine, in treating skin diseases. TCM targets skin symptoms and achieves significant short-term improvement in SD by adjusting the constitution and internal balance. In cases where conventional Western therapies fail to achieve remission, TCM offers a viable, safe, and cost-effective alternative treatment modality.
Acknowledgment
We extend our gratitude to the patients and their families who participated in this study; their trust and support were instrumental in the smooth conduct of this report, which holds significant importance for advancing medical knowledge and improving patient care.
Ethical Considerations
The authors of this article confirm that there are no direct financial conflicts of interest. There has been no financial support received from pharmaceutical companies or health organizations related to this study; there are no affiliations or involvement with any institutions that have financial interests; there are no personal interests that could affect the content of the study; and the research methods do not involve any patents or proprietary information. Furthermore, this case is original and has not been published elsewhere, and the data supporting the conclusions will be made publicly transparent. The authors understand the importance of disclosing potential conflicts of interest and ensuring that the information provided is accurate and based on the best available knowledge.
References
- Sampaio AL, Mameri AC, Vargas TJ, Ramos-e-Silva M, Nunes AP, et al. (2011) Seborrheic dermatitis. An Bras Dermatol 86: 1061-1074.
- Zhang F, Li Y, Ren W, Li S (2023) Establishment of clinical evaluation criteria for scalp seborrheic dermatitis. J Cosmet Dermatol 22: 3042-3046.
- Emtiazy M, Zareie E, Shirbeigi L, Sadeghpour O, Mansouri P (2018) Effect of oral herbal medicament on scalp seborrhea and gastrointestinal symptoms in a male patient: A case report. Iran J Public Health 47: 1030.
- Sowell J, Pena SM, Elewski BE (2022) Seborrheic dermatitis in older adults: Pathogenesis and treatment options. Drugs Aging 39: 315-321.
- Barak-Shinar D, Del Río R, Green LJ (2017) Treatment of seborrheic dermatitis using a novel herbal-based cream. J Clin Aesthet Dermatol 10: 17-23.
- Micali G, Lacarrubba F, Dall'Oglio F, Tedeschi A, Dirschka T (2017) A new proposed severity score for seborrheic dermatitis of the face: SEborrheic Dermatitis Area and Severity Index (SEDASI). Journal of the American Academy of Dermatology 76: 18.
- Mustarichie R, Rostinawati T, Pitaloka DAE, Saptarini NM, Iskandar Y (2022) Herbal Therapy for the Treatment of Seborrhea Dermatitis. Clin Cosmet Investig Dermatol15: 2391-2405.
- Asz-Sigall D, Tosti A Pirmez R (2020) Seborrheic Dermatitis. Hair and Scalp Treatments: A Practical Guide 161-176.
- Shenefelt PD (2012) Herbal treatment for dermatologic disorders. In: Herbal Medicine: Biomolecular and Clinical Aspects. 2nd edition. Boca Raton (FL): CRC Press/Taylor & Francis; 2011, Chapter 18.
- Koo JS, Seo BI (2016) A case of Seborrheic dermatitis treated by Bangpungtongsungsangamibang. The Korea Journal of Herbology 31: 1-5.
- Tang S, Ren J, Kong L, Yan G, Liu C, et al. (2023) Ephedrae Herba: A Review of Its Phytochemistry, Pharmacology, Clinical Application, and Alkaloid Toxicity. Molecules 28: 663.
- Liu K, Han S, Gao W, Tang YN, Han X, et al. (2021) Changes of mineralogical properties and biological activities of gypsum and its calcined products with different phase structures. Evidence-Based Complementary and Alternative Medicine 2021: 1-14.
- Ko HM, Lee SH, Jee W, Jung JH, Kim KI, et al. (2021). Gancaonin N from Glycyrrhiza uralensis attenuates the inflammatory response by downregulating the NF-κB/MAPK pathway on an acute pneumonia in vitro model. Pharmaceutics 13: 1028.
- Ullah K, Shah G, Alam J, Gul A, Omran A, et al. (2024). Ethnopharmacological and phytochemical assessment of medicinal plants used against livestock infections by tribal community under semi-arid conditions. Applied ecology and environmental research 22: 881-900.
- Yu Y, Wang L (2023) Study on the Rule of Traditional Chinese Medicine in Treating Psoriasis with Blood Heat Syndrome Based on Data Mining. MEDS Chinese Medicine 5: 42-49.
- Luo Y, Chen J, Kuai L, Zhang Y, Ding X, et al. (2021) Chinese herbal medicine for psoriasis: evidence from 11 high-quality randomized controlled trials. Frontiers in Pharmacology 11: 599433.
- Zhang Q, Xie J, Li G, Wang F, Lin J, et al. (2022) Psoriasis treatment using Indigo Naturalis: Progress and strategy. Journal of Ethnopharmacology 297: 115522.
- Yingshuai L, Yan L (2023) Progress in the study of Yang-deficiency constitution in terms of Traditional Chinese Medicine: a narrative review. Journal of Traditional Chinese Medicine 43: 409.
Citation: Chiu P-H, Chen T-C, Li P-Y, Chung H-Y, Arai I, et al. (2024) Significant Efficacy of Traditional Chinese Medicine and Herbal Treatment on Chronic Seborrheic Dermatitis: A Case Report. J Altern Complement Integr Med 10: 473.
Copyright: © 2024 Po-Hsuan Chiu, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

