
Simultaneous Quadruple Nerve Transfer for Independent Zonal Facial Reanimation Following Traumatic Facial Paralysis: A Case Report
*Corresponding Author(s):
Celeste NagyDepartment Of Otolaryngology Head And Neck Surgery, Emory University School Of Medicine, Atlanta, GA, United States
Tel:+1 2144170806,
Email:celenagy@gmail.com
Abstract
Traumatic Facial Paralysis (FP) after nerve transection with an inaccessible proximal stump poses a reanimation challenge. We describe a systematic method for reanimation via reinnervation with four distinct donor nerves plus static techniques for symmetric, independent zonal reanimation of the upper, middle, and lower face. Pre-operative eFACE and FaCE scores were 61 and 33. At the 12 month post-operative period, the patient had symmetric tone and motion across all facial zones. Post-operative eFACE and FaCE scores were 87 and 52.Using the described technique for complete FP without proximal nerve stump accessibility one can achieve independent zonal reinnervation and reanimation.
Keywords
Crossface graft; Donor nerve; Facial nerve; Facial nerve reanimation; Facial paralysis; Facial reanimation; Hypoglossal nerve graft; Masseter nerve graft; Nerve graft; Sural nerve graft, Synkinesis
INTRODUCTION
Facial Paralysis (FP) is a devastating condition causing functional, aesthetic and psychosocial impairments [1]. Complete flaccid FP typically follows acute traumatic injury to the main trunk of the facial nerve. This results in a loss of resting tone and movement diffusely, resulting in brow ptosis, lagophthalmos, ectropion, nasal obstruction, midface ptosis, oral incompetence and dysarthria [1]. Ocular protection and smile restoration are top priority goals of the reanimation process. Within the first two years following nerve insult, the facial muscles remain receptive to reinnervation. Following this period, the muscles undergo fibrosis and atrophy rendering them nonfunctional. It is therefore critical to proceed with reinnervation procedures prior to this period in order to achieve dynamic restoration using native musculature. Following known or suspected nerve transection, exploration with primary repair or interposition grafting should be attempted as soon as feasible. In cases where the proximal facial nerve stump is unavailable or inaccessible, nerve transfer procedures should be considered for reinnervation [1,2]. Here, we present a case using four distinct donor nerves to perform four separate nerve transfers to independently reinnervate the upper, middle and lower face following traumatic transection of the intratemporal facial nerve.
Full analysis of pre and post-operative evaluation for complete facial paralysis and reconstruction are beyond the scope of this report. However, we use the validated electronic facial paralysis assessment tool (eFACE) and the Facial Clinimetric Evaluation (FaCE) scores for objective identification and improvement of this patient’s facial paralysis. The eFACE provides comprehensive information through weighted clinician-graded continuous visual analog scales of 16 categories (5 static, 7 dynamic, and 4 synkinetic zonal parameters), such as oral commissure excursion and philtral deviation [1]. Each domain of facial function (static, dynamic, and synkinesis) range from 1 to 100, with 100 representing normal facial symmetry and/or function. Final score is determined by averaging of all the domains [3]. FaCE are patient-graded scales designed to assess symptom severity and impact of quality of life [1]. The questionnaire consists of 15 questions with a 5-point Likert scale. The FaCE Scale comprises six domains; facial movement, facial comfort, oral function, eye comfort, lacrimal control, and social function. Domain scores range from 0 (worst) to 100 (best) and total score is averaged [4].
REPORT OF CASE
A 22-year-old male suffered a gunshot wound to the left preauricular area that traversed the external auditory canal and mastoid. He had immediate complete left sided flaccid facial paralysis. He presented 3 weeks after the event with florid mastoiditis and was taken for mastoidectomy and debridement. Attempts were made to identify the proximal facial nerve stump, however, these attempts were unsuccessful secondary to missile damage and infection. He reported left-sided lagophthalmos with dry eye symptoms, nasal obstruction, cheek biting, dysarthria, oral incompetence and smiling inability. Pre-operative eFACE and FaCE scores [3,4] were 61 and 33, respectively.
Given the recent timing of the injury (~ 1 month) and inaccessible proximal facial nerve stump, electrophysical studies were not deemed necessary in this case. The mastoid segment of the facial nerve was known to be transected and there was not concern for facial musculature fibrosis. Therefore, a quadruple nerve transfer was planned to independently reinnervate the upper, middle, and lower facial zones. On the left, a pre-auricular face lift incision was performed and a subcutaneous skin flap was elevated anterior to the parotid gland to the nasolabial fold. The zygomaticus major muscle was identified and dissection took place superficial to this muscle to protect distal nerve branches. Retrograde dissection on each nerve branch was performed, removing all parotid tissue superficial to each nerve branch, and was continued until the pes anserinus and main trunk were identified. There were two separate marginal mandibular-cervical complexes identified that were transected sharply near the pes and mobilized extensively to allow for eventual end-to-side anastomosis with the hypoglossal nerve and descending hypoglossi. The buccal branch was likewise transected sharply near the pes as was a zygomatic branch traveling to the orbicularis oculi. The left infratemporal fossa dissection for the identification of the masseteric nerve then ensued. A subzygomatic triangle was marked out which included the zygomatic arch, the anterior border of the condyle as well as the frontal branch of the facial nerve. Within the triangle, the parotid fascia was incised 1 cm below the zygomatic arch and the masseter muscle fibers were slowly dissected until the masseteric nerve was eventually identified. This was stimulated with 2 mA on the nerve stimulator with a large muscular response. The nerve was then traced distally and sharply transected for eventual anastomosis with the left buccal branch. Next, the anterior border of the sternocleidomastoid muscle was skeletonized moving medially towards the posterior belly of the digastric muscle. Deep to this, the hypoglossal nerve was identified and extensively mobilized for eventual end-to-side anastomosis with the marginal mandibular-cervical division. The descending hypoglossi branch was also identified and transected distally for eventual end-to-end anastomosis with an additional marginal mandibular - cervical division.
The right side was addressed with a pre-auricular face lift incision and a subcutaneous skin flap was elevated anterior to the parotid gland. There was redundancy of the frontalis/oculi branch to the orbicularis oculi, therefore the oculi branch of the zygomatic nerve was chosen to be sharply transected from the donor nerve for the cross-facial nerve graft with a sural nerve graft to the left zygomatic oculi branch.
Full operative technique is beyond the scope of this report, but the following nerve transfers were performed: 1) End-to end crossfacial nerve graft from largest redundant right zygomatic oculi branch to distal left zygomatic oculi branch using a sural nerve graft 2) End-to-end left nerve to masseter to distal left zygomatic branch supplying zygomaticus muscle complex 3) End-to-side distal left marginal mandibular branch to left hypoglossal nerve 4) End-to-end left descending hypoglossal nerve to distal left cervical branch. A depiction of the nerve procedures can be seen in figure 1. Additionally, a single-strip fascia lata graft was placed along the left nasolabial crease using the minimally invasive technique described by Faris et al., [5] as well as a right depressor labii inferioris resection as described by Lindsay et al., [6]. Post-operatively, #10 fluted Blake drains were placed in each facial/neck cavity, but compressive dressings were avoided. The patient was hospitalized for two days until the drains could be removed and he was not allowed to manipulate his face, valsalva, or undergo strenuous exercise for 7-10 days post-operatively.
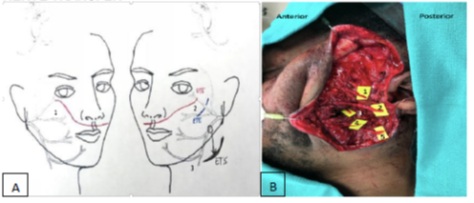
Figure 1A:
1) End-to end crossfacial nerve graft from largest redundant right zygomatic oculi branch to distal left zygomatic oculi branch using a sural nerve graft
2) End-to-end left nerve to masseter to distal left zygomatic branch supplying zygomaticus muscle complex
3) End-to-side distal left marginal mandibular branch to left hypoglossal nerve
Not pictured: End-to-end left descending hypoglossal nerve to distal left cervical branch
Figure 1B:
1) Left zygomatic branch of the facial nerve to orbicularis oculi
2) Left zygomatic branch of the facial nerve to zygomatic muscle complex
3) Left nerve to masseter
4 & 5) Left marginal mandibular branch of the facial nerve
Not pictured: LEFT hypoglossal nerve, LEFT descending hypoglossi nerve, LEFT cervical branch of the facial nerve
Figure 1: Schematic Depiction and Intraoperative Photos of Quadruple Nerve Transfer.
The patient was last evaluated 12 months postoperatively. He has excellent tone across all facial zones. Patient has declined facial physiotherapy for emotive smile strategies. He has not had tongue atrophy or difficulty with speech or eating. However, he did develop moderate oral-ocular synkinesis when he performs a volitional smile with bite-down technique. His synkinesis has been responsive to onabotulinumtoxinA injections to the orbicularis oculi. Post-operative eFACE and FaCE scores were 87 and 52, respectively. Pre- and postoperative photos are included in figure 2.
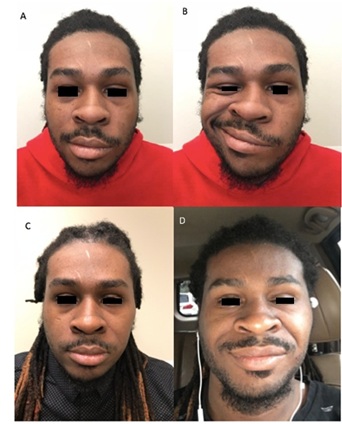
Figure 2:
A) Pre-operative photo at rest showing tone asymmetry
B) Pre-operative smile photo with complete left-sided facial paralysis
C) Post-operative photo at rest showing symmetric tone
D) Post-operative volitional smile photo demonstrating symmetric smile with oral-ocular
synkinesis requiring onabotulinumtoxinA injections to left orbicularis oculi
Figure 2: Preoperative and Postoperative Photos.
DISCUSSION
Acute traumatic FP with an inaccessible proximal facial nerve stump poses a reanimation challenge. Using 4 distinct donor nerves, independent zonal reinnervation was achieved. A redundant contralateral branch to the oculi musculature was used to restore ipsilateral periorbital tone. All ipsilateral masseteric axons were utilized to maximize oral excursion via the dominant zygomatic branch to the zygomatic musculature. Finally, two additional donor nerves were transferred to maintain symmetry of the lower face as the nerves were all of similar caliber. The described technique provides a systematic method for management of acute traumatic FP with an inaccessible facial nerve stump.
REFERENCES
- Jowett N, Hadlock TA (2015) An Evidence-Based Approach to Facial Reanimation. Facial Plast Surg Clin North Am 23: 313-334.
- Bhama PK, Hadlock TA (2016) Management of the Paralyzed Face. Facial Plastic and Reconstructive Surgery, 4th ed., Thieme Pg no.37-744.
- Banks CA, Bhama PK, Park J, Hadlock CR, Hadlock TA (2015) Clinician-Graded Electronic Facial Paralysis Assessment: The eFACE. Plast Reconstr Surg 136: 223e-230e.
- Kahn JB, Gliklich RE, Boyev KP, Stewart MG, Metson RB, et al. (2001) Validation of a patient-graded instrument for facial nerve paralysis: the FaCE scale. Laryngoscope 111: 387-398.
- Faris C, Heiser A, Jowett N, Hadlock T (2018) Minimal Nasolabial Incision Technique for Nasolabial Fold Modification in Patients With Facial Paralysis. JAMA Facial Plast Surg 20:148-153.
- Lindsay RW, Edwards C, Smitson C, Cheney ML, Hadlock TA (2011) A systematic algorithm for the management of lower lip asymmetry. Am J Otolaryngol 32:1-7.
Citation: Nagy C, Mattox DE, Baddour HM (2020) Simultaneous Quadruple Nerve Transfer for Independent Zonal Facial Reanimation Following Traumatic Facial Paralysis: A Case Report. J Otolaryng Head Neck Surg 6: 44
Copyright: © 2020 Celeste Nagy, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

