Journal of Medicine Study & Research Category: Medical
Type: Case Report
Single-Photon Emission Computed Tomography / Computed Tomography (Hybrid Imaging) in the Diagnosis of Unilateral Facet Joint Arthritis after Internal Fixation for Atlas Fracture
*Corresponding Author(s):
Shin-Tsu ChangDepartment Of Physical Medicine And Rehabilitation, Tri-Service General Hospital, School Of Medicine, National Defense Medical Center, Chung Shan Medical University, No.161, Sec. 6, Minquan East Road, Neihu District, Taipei,Taichung, Taiwan, Province Of China
Tel:+886 423741350,
Fax:+886 945605523
Email:ccdivlaser1959@gmail.com
Received Date: Jun 08, 2019
Accepted Date: Jun 18, 2019
Published Date: Jun 25, 2019
Abstract
Cervical facet joint, one of the potential sources of spinal and extremity pain, is susceptible to arthritic changes, degenerative process, inflammation, and injury and all of which will lead to painful event upon movement and restriction in range of neck motion. A definite diagnosis will help us to make sure the exact reason for the discomfort. We herein report a case with neck discomfort after surgery due to prior degeneration of cervical facet joint, rather than the operative procedure or internal fixator fixed in neck. Combination of high sensitivity of SPECT and high specificity of CT, as hybrid SPECT/CT, has been shown to obtain diagnostic accuracy in clinical practice. With the help of hybrid SPECT/CT imaging in vertebral disorders, the clinical pictures of our patient to identify facet joint arthropathy, rather than surgical procedure or implantation. The fact of unilateral facet joint erosion at C3/4 confirmed the role of prior facet pathology and a setback in the recovery upon a subsequent injury, returning to the holy tasks performed by neurosurgeon.
Keywords
Atlas; Bone scan; Cervical Spine; Facet joint; Fracture; Hybrid imaging
INTRODUCTION
Chronic neck pain commonly comes across in modern health attention [1]. Unlike the thoracic and lumbar spines, the cervical spines have distinct size and shape of vertebral components, particularly transverse and posterior processes, and facet (zygapophyseal) joints; the latter has been created as one of the potential sources of spinal and extremity pain [2,3]. Cervical facet joint is susceptible to arthritic changes, degenerative process, inflammation, and injury, and all of which will lead to painful event upon movement and restriction in range of neck motion [4-6].
In respect to consequence of neck injury due to vehicle accident or other incidents, if any discomfort remained after operation, the discomfort patients concerned was usually attributed to surgical procedure or implantation, no matter how the endeavor has been paid from the surgeons. A definite diagnosis will help us to make sure the exact reason for the discomfort. We herein report a case with neck discomfort after surgery due to prior degeneration of cervical facet joint, rather than the operative procedure or internal fixator fixed in neck.
In respect to consequence of neck injury due to vehicle accident or other incidents, if any discomfort remained after operation, the discomfort patients concerned was usually attributed to surgical procedure or implantation, no matter how the endeavor has been paid from the surgeons. A definite diagnosis will help us to make sure the exact reason for the discomfort. We herein report a case with neck discomfort after surgery due to prior degeneration of cervical facet joint, rather than the operative procedure or internal fixator fixed in neck.
CASE PRESENTATION
Patient, a 50 year-old man, suffered from a vehicle accident on 21/10/2018. The accident happened when he was riding a motorcycle and hitting by a rushing car, and he lost his consciousness for 1-2 hours at that time. He was sent to our ER, where multiple injuries were noted, including fractures of orbital floor, metatarsal bones, right 4th metatarsal bone, left ulna and left distal radius, and most important, closed fracture of atlas (C1) spine, shown as Computed Tomography (CT) scan in (Figure 1a-1e). He experienced multiple operations since them. Of them was C1 posterior spinal fusion surgery. The post-OP plain films of C-spine showed the good alignment of internal fixator (Figure 2a-2d). Unexpectedly, he reported severe neck pain, tenderness and numbness over scalp and neck stiffness two weeks after operation. Besides, he mentioned right upper limb pain with numbness from shoulder, upper arm, elbow, to the back of the hand of 1-3 fingers. The pain exaggerated while he was yawning (pain score = 8).
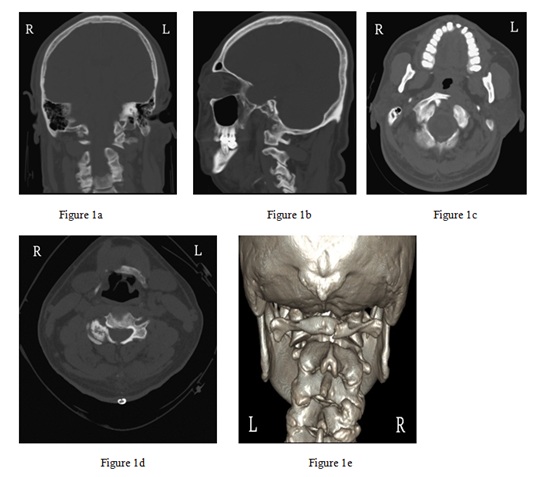
Figure 1: CT scan of cervical spine.
Coronal section (a) Sagittal section, (b) Axial section of C1, (c) Axial section of C3, (d) 3D Reconstruction, and (e) showing obvious fracture in the C1 vertebra.
R = Right side; L = Left side.
Coronal section (a) Sagittal section, (b) Axial section of C1, (c) Axial section of C3, (d) 3D Reconstruction, and (e) showing obvious fracture in the C1 vertebra.
R = Right side; L = Left side.

Figure 2: Plain films of cervical spine after surgical internal fixation.
AP view (a) Lateral view, (b) Hyper-flexion view, (c) Hyper-extension view and (d) showing apparent restrict range of motion while doing hyperextension of cervical spine.
AP view (a) Lateral view, (b) Hyper-flexion view, (c) Hyper-extension view and (d) showing apparent restrict range of motion while doing hyperextension of cervical spine.
The condition has persisted for 6-7 months even after C spine surgery, and became worsen leading to poor sleep. He came to our OPD for help, and showed the exact painful location (Figure 3). Physical examination showed limited neck ROM at every direction, decreased muscle power over right upper limb, and decreased right-sided DTR. C-Spine MRI performed on 06/04/2019 only revealed herniation of intervertebral discs, C3-4, C4-5, C5-6, and C6-7. Bone scan with hybrid images was suggested and performed on 25/02/2019 disclosing increased bone turnover located at right C3/4 facet joint (Figure 4). Instead, there was no any increased uptake found in C1 and operated area. Patient received the fact that the painful discomfort came from his prior old C3/4 arthropathy, rather than the surgical procedure or metallic implantation.

Figure 3: The significant tender point in the right-sided neck pointed out by left middle finger tip of our case.
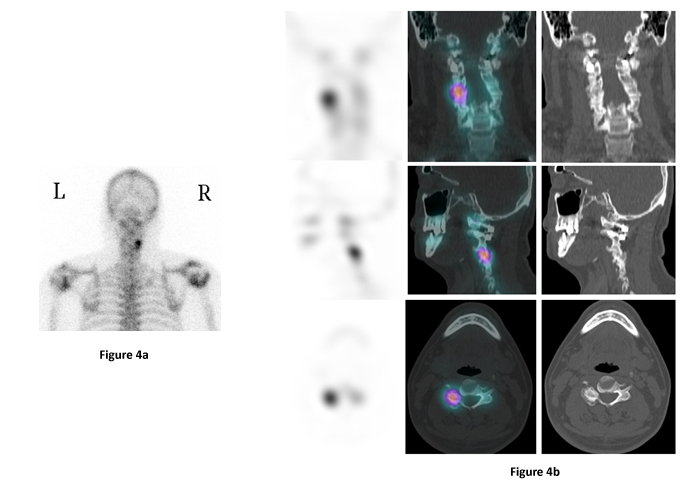
Figure 4: Images of bone scan of the case.
Image of whole body bone scan seen from behind (a) SPECT/CT images (b) Coronal section (upper panels X 3), Sagittal section (middle panels X 3), and axial section (lower panels X 3).
An increased uptake in the C3/C4 facet joint can be seen on the right side compared to the corresponding location on the left side.
R = right side; L = left side.
An increased uptake in the C3/C4 facet joint can be seen on the right side compared to the corresponding location on the left side.
R = right side; L = left side.
Under the diagnosis of unilateral facet joint arthropathy in C3/4, patient agreed to allow us to treat him by using blocking the medial branches of the dorsal ramus of the spinal nerves under local anesthetic. He was lying in a lateral position on the injection table with a pillow was placed under his head. The exact position of the injection was marked, and a 22 gauge needle was forwarded under sonographic guide until it contact to the facet joint capsule. When the needle was in the proper position, the steroid was injected. No allergic reactions or cardiovascular abnormalities took place, and neurological examination was normal. The relevant injections provided significant pain relief, and the painful restriction improved much after the twice pain-killing procedures. Patient refused to have the identical hybrid images for follow-up.
DISCUSSION
The cervical facet joint has been known as a pain generator in neck, and a stress lesion in cervical facet joint can hamper patients in his daily activities, for example, injury after sports or car driving. Diagnosis of facet joint arthropathy sends a challenge to clinicians, because conventional radiological tests such as Magnetic Resonance (MR), plain CT, dynamic bending films, and planar radionuclide bone scanning are inconsistently reliable when accurately localizing pain generators in facet joints [7]. Single Photon Emission Computed Tomography (SPECT) has been widely accepted to evaluate patients with spinal pain and facet joint arthropathy. Skeletal scintigraphy with SPECT provides functional imaging and is sensitive for detecting micro calcification due to increased osteoblastic activity, which foci of increased activity reflect areas of mechanical stress and degenerative change in the skeleton, even in the absence of other pathology [8].
Nonetheless, with SPECT imaging alone, there can be difficulty in precise localization due to anatomical variants and the low spatial resolution of the scan (7 mm only) [9]. Combination of high sensitivity of SPECT and high specificity of CT, as multimodality hybrid SPECT/CT, emerges to meet a historic destiny. The CT module gets the SPECT image better quality by correcting for soft tissue attenuation, thus improving sensitivity of the scan for regions of unusual tracer activity. The CT has a higher spatial resolution of 1 mm and fusion of the scan images allows better localization of abnormal tracer activity and defines congenital anomalies that may affect segmental nomenclature. The anatomy upon the CT component also improves scan specificity by defining the structural pathology causing increased tracer activity. SPECT/CT is gaining popularity and has already been shown to bring together diagnostic accuracy in clinical practice. With the help of hybrid SPECT/CT imaging in vertebral disorders, the clinical pictures of our patient confirmed the exact source of pain from the right C3/4 facet joint, which corroborate McDonald et al. [10], who used SPECT/CT to identify facet joint arthropathy in lumbar spine, although not cervical spine like our case.
Biomechanical studies of the cervical spine kinematics during a whiplash load also reveal possibilities for permanent lesions of the facet joints and capsules, even with minor loading [11-14]. Based on biomechanical research, postmortem studies, and clinical research, Bogduk et al. claimed that cervical facet joints are prone to impact during whiplash suffering [12]. Degeneration of the cervical facet joint can be easily resulted from abnormal motion associated with disc degeneration and arthritis [5,6]. A randomized double-blind placebo control trial in Sweden explored the prevalence of cervical facet joint pain in chronic Whiplash Associated Disorder (WAD), and confirmed that a substantial amount of patients with chronic WAD have their persistent pain emanating from cervical facet joints. The trial also found that the most common level being responsible for the pain is level C5/C6, and females, rather than males, are more prone to report a positive response to medial branch blocks, which blocks as a diagnostic tool for the joint pain [15]. Our case represented the level being responsible for the pain is level C3/C4 because of prior erosion change (Figure 1d). A latest study assessed its prevalence in asymptomatic patients and found that the prevalence of asymptomatic cervical facet arthritis (grade 1-3) was 33% (grade 1, 19%; grade 2, 11%; and grade 3, 3%), and the C6-C7 levels was the most likely to show arthritic changes [16].
With respect to the radiological parameters of unregenerate facet joint of cervical spine, a Korean study confirmed as 5.0 mm in normal cervical disc height and 1.4 mm in normal facet joint space [17]. The facet joint degeneration in Rt C3/4 is compatible with grade III (Figure 1d), as category of Park et al [18]. Degenerated facet joints have been demonstrated mort common at C2-C3 level, and facet degenerative changes were more common in patients above 50 years old [19]. However, our case occurred only in facet joint of C3-4 because of prior joint erosion.
Our case occurred only in facet joint of C3-4 in the right side. The reason for unilateral occurrence is unclear. An article of Van Vlasselaer et al. provided some information regarding structural asymmetry of cervical spines, who studied the morphology of superior facet joints from C3 through C7, by measuring facet dimensions, surface area, curvature, and degeneration of the joints [20]. They found that when a facet exhibits a higher degree of degeneration, it often results in a bigger total facet surface; therefore, for degeneration, there are major differences regardless of the side-occurrence, e.g. one side can show very strong degeneration, while the other side preserves. They also stated that asymmetry in the degree of degeneration and morphology of the superior facets of cervical spines will involve ipsilateral symptom, motion limits and instability. There was a significant correlation between the dimensions of the total facet surface and the degree of degeneration, e.g. the bigger difference in degeneration asymmetry, the bigger difference in facet joint dimension asymmetry [20].
The facet joint pain in neck can be managed with therapeutic pain-killing including facet joint nerve blocks, facet joint neurolytic procedures, or intraarticular injections like our case [21]. Controlled comparative local anesthetic block is an eligible substitute for confirming the diagnosis in patients clinically suspected of having characteristic facet joint arthropathy [22]. The facet joint pain can be obviously ameliorated in pain score and disability by therapeutic application of modalities, or steroid as shown in our patient who obtained remarkable amelioration in neck painful after steroid injection [2,3,23].
While we investigate the reason for neck pain and restrict range of motion, the prior operated location is often thought as one of the contributors. However, the neighboring tissues surrounding the operated region cannot be ignored. Viewing the images of our case, the adjacent facet joint, even unilateral, might contribute the development of clinical neck pain and stiffness. We have solved a major issue on the debate; at least, because the patient misread the neck pain/stiffness was caused by the surgical procedure or metallic implantation. Instead, hybrid SPECT/CT images failed to show any inflamed spot close to the operated area, meaning an excellent operative procedure performed by neurosurgeon.
The limitation/weak point of this case report was, after steroid injection, without second hybrid images for follow-up due to amelioration of pain. The second was no comparable cases to show, which might disappoint the readers who wonder if there were retrospective data of such patients. The third was the type of diagnosis, which sit actual quite common in Europe, but not in Taiwan.
The fact of unilateral facet joint erosion at C3/4 raised confirmation that the role of prior facet joint arthropathy and a setback in the recovery upon a subsequent injury, returning to the holy tasks performed by neurosurgeon.
Nonetheless, with SPECT imaging alone, there can be difficulty in precise localization due to anatomical variants and the low spatial resolution of the scan (7 mm only) [9]. Combination of high sensitivity of SPECT and high specificity of CT, as multimodality hybrid SPECT/CT, emerges to meet a historic destiny. The CT module gets the SPECT image better quality by correcting for soft tissue attenuation, thus improving sensitivity of the scan for regions of unusual tracer activity. The CT has a higher spatial resolution of 1 mm and fusion of the scan images allows better localization of abnormal tracer activity and defines congenital anomalies that may affect segmental nomenclature. The anatomy upon the CT component also improves scan specificity by defining the structural pathology causing increased tracer activity. SPECT/CT is gaining popularity and has already been shown to bring together diagnostic accuracy in clinical practice. With the help of hybrid SPECT/CT imaging in vertebral disorders, the clinical pictures of our patient confirmed the exact source of pain from the right C3/4 facet joint, which corroborate McDonald et al. [10], who used SPECT/CT to identify facet joint arthropathy in lumbar spine, although not cervical spine like our case.
Biomechanical studies of the cervical spine kinematics during a whiplash load also reveal possibilities for permanent lesions of the facet joints and capsules, even with minor loading [11-14]. Based on biomechanical research, postmortem studies, and clinical research, Bogduk et al. claimed that cervical facet joints are prone to impact during whiplash suffering [12]. Degeneration of the cervical facet joint can be easily resulted from abnormal motion associated with disc degeneration and arthritis [5,6]. A randomized double-blind placebo control trial in Sweden explored the prevalence of cervical facet joint pain in chronic Whiplash Associated Disorder (WAD), and confirmed that a substantial amount of patients with chronic WAD have their persistent pain emanating from cervical facet joints. The trial also found that the most common level being responsible for the pain is level C5/C6, and females, rather than males, are more prone to report a positive response to medial branch blocks, which blocks as a diagnostic tool for the joint pain [15]. Our case represented the level being responsible for the pain is level C3/C4 because of prior erosion change (Figure 1d). A latest study assessed its prevalence in asymptomatic patients and found that the prevalence of asymptomatic cervical facet arthritis (grade 1-3) was 33% (grade 1, 19%; grade 2, 11%; and grade 3, 3%), and the C6-C7 levels was the most likely to show arthritic changes [16].
With respect to the radiological parameters of unregenerate facet joint of cervical spine, a Korean study confirmed as 5.0 mm in normal cervical disc height and 1.4 mm in normal facet joint space [17]. The facet joint degeneration in Rt C3/4 is compatible with grade III (Figure 1d), as category of Park et al [18]. Degenerated facet joints have been demonstrated mort common at C2-C3 level, and facet degenerative changes were more common in patients above 50 years old [19]. However, our case occurred only in facet joint of C3-4 because of prior joint erosion.
Our case occurred only in facet joint of C3-4 in the right side. The reason for unilateral occurrence is unclear. An article of Van Vlasselaer et al. provided some information regarding structural asymmetry of cervical spines, who studied the morphology of superior facet joints from C3 through C7, by measuring facet dimensions, surface area, curvature, and degeneration of the joints [20]. They found that when a facet exhibits a higher degree of degeneration, it often results in a bigger total facet surface; therefore, for degeneration, there are major differences regardless of the side-occurrence, e.g. one side can show very strong degeneration, while the other side preserves. They also stated that asymmetry in the degree of degeneration and morphology of the superior facets of cervical spines will involve ipsilateral symptom, motion limits and instability. There was a significant correlation between the dimensions of the total facet surface and the degree of degeneration, e.g. the bigger difference in degeneration asymmetry, the bigger difference in facet joint dimension asymmetry [20].
The facet joint pain in neck can be managed with therapeutic pain-killing including facet joint nerve blocks, facet joint neurolytic procedures, or intraarticular injections like our case [21]. Controlled comparative local anesthetic block is an eligible substitute for confirming the diagnosis in patients clinically suspected of having characteristic facet joint arthropathy [22]. The facet joint pain can be obviously ameliorated in pain score and disability by therapeutic application of modalities, or steroid as shown in our patient who obtained remarkable amelioration in neck painful after steroid injection [2,3,23].
While we investigate the reason for neck pain and restrict range of motion, the prior operated location is often thought as one of the contributors. However, the neighboring tissues surrounding the operated region cannot be ignored. Viewing the images of our case, the adjacent facet joint, even unilateral, might contribute the development of clinical neck pain and stiffness. We have solved a major issue on the debate; at least, because the patient misread the neck pain/stiffness was caused by the surgical procedure or metallic implantation. Instead, hybrid SPECT/CT images failed to show any inflamed spot close to the operated area, meaning an excellent operative procedure performed by neurosurgeon.
The limitation/weak point of this case report was, after steroid injection, without second hybrid images for follow-up due to amelioration of pain. The second was no comparable cases to show, which might disappoint the readers who wonder if there were retrospective data of such patients. The third was the type of diagnosis, which sit actual quite common in Europe, but not in Taiwan.
The fact of unilateral facet joint erosion at C3/4 raised confirmation that the role of prior facet joint arthropathy and a setback in the recovery upon a subsequent injury, returning to the holy tasks performed by neurosurgeon.
REFERENCES
- Hoy D, March L, Woolf A, Blyth F, Brooks P, et al. (2014) The global burden of neck pain: Estimates from the global burden of disease 2010 study. Ann Rheum Dis 73: 1309-1315.
- Rubinstein SM, van Tulder M (2008) A best-evidence review of diagnostic procedures for neck and low-back pain. Best Pract Res Clin Rheumatol 22: 471-482.
- Boswell MV, Manchikanti L, Kaye AD, Bakshi S, Gharibo CG, et al. (2015) A Best-evidence systematic appraisal of the diagnostic accuracy and utility of facet (zygapophysial) joint injections in chronic spinal pain. Pain Physician 18: 497-533.
- Windsor RE, Nagula D, Storm S, Overton A, Jahnke S (2003) Electrical stimulation induced cervical medial branch referral patterns. Pain Physician 6: 411-418.
- Bykowski JL, Wong WH (2012) Role of facet joints in spine pain and image-guided treatment: A review. AJNR Am J Neuroradiol 33: 1419-1426.
- Gellhorn AC, Katz JN, Suri P (2013) Osteoarthritis of the spine: The facet joints. Nat Rev Rheumatol 9: 216-224.
- Boswell MV, Shah RV, Everett CR, Sehgal N, Mckenzie-Brown AM, et al. (2005) Interventional techniques in the management of chronic spinal pain: Evidence-based practice guidelines. Pain Physician 8: 1-47.
- Delbeke D, Schöder H, Martin WH, Wahl RL (2009) Hybrid imaging (SPECT/CT and PET/CT): improving therapeutic decisions. Semin Nucl Med 39: 308-340.
- Matar HE, Navalkissoor S, Berovic M, Shetty R, Garlick N, et al. (2013) Is hybrid imaging (SPECT/CT) a useful adjunct in the management of suspected facet joints arthropathy? Int Orthop 37: 865-870.
- McDonald M, Cooper R, Wang MY (2007) Use of computed tomography-single-photon emission computed tomography fusion for diagnosing painful facet arthropathy. Technical note. Neurosurg Focus 22: 2.
- Cusick JF, Pintar FA, Yoganandan N (2001) Whiplash syndrome: Kinematic factors influencing pain patterns. Spine 26: 1252-1258.
- Bogduk N, Yoganandan N (2001) Biomechanics of the cervical spine Part 3: Minor injuries. Clin Biomech (Bristol, Avon) 16: 267-275.
- Stemper BD, Yoganandan N, Pintar FA (2004) Gender- and region-dependent local facet joint kinematics in rear impact: Implications in whiplash injury. Spine 29: 1764-1771.
- Cavanaugh JM, Lu Y, Chen C, Kallakuri S (2006) Pain generation in lumbar and cervical facet joints. J Bone Joint Surg Am 88: 63-67.
- Persson M, Sörensen J, Gerdle B (2016) Chronic Whiplash Associated Disorders (WAD): Responses to Nerve Blocks of Cervical Zygapophyseal Joints. Pain Med 17: 2162-2175.
- Kim JH, Sharan A, Cho W, Emam M, Hagen M, et al. (2019) The prevalence of asymptomatic cervical and lumbar facet arthropathy: a computed tomography study. Asian Spine J 13: 417-422.
- Choi SH, Lee H, Cho JH, Jung JI, Lee DH (2017) Radiological parameters of undegenerated cervical vertebral segments in a Korean population. Clin Orthop Surg 9: 63-70.
- Park MS, Lee YB, Moon SH, Lee HM, Kim TH, et al. (2014) Facet joint degeneration of the cervical spine: a computed tomographic analysis of 320 patients. Spine (Phila Pa 1976) 39: 713-718.
- Rong X, Liu Z, Wang B, Pan X, Liu H (2017) Relationship between facet tropism and facet joint degeneration in the sub-axial cervical spine. BMC Musculoskelet Disord 18: 86.
- Van Vlasselaer N, Van Roy P, Cattrysse E (2017) Morphological asymmetry of the superior cervical facets from C3 through C7 due to degeneration. Biomed Res Int 2017: 5216087.
- Falco FJE, Manchikanti L, Datta S, Wargo BW, Geffert S, et al. (2012) Systematic review of therapeutic effectiveness of cervical facet joint interventions: An update. Pain Physician 15: 839-868.
- Sehgal N, Dunbar EE, Shah RV, Colson JD (2007) Systematic review of diagnostic utility of facet (zygapophysial) joint injections in chronic spinal pain: an update. Pain Physician 10: 213-228.
- Wiechert K (2018) Lumbar epidural and cervical facet joint injection techniques. Eur Spine J 27: 568-570.
Citation: Chang ST, Liu CC, Yang WH (2019) Single-Photon Emission Computed Tomography / Computed Tomography (Hybrid Imaging) in the Diagnosis of Unilateral Facet Joint Arthritis after Internal Fixation for Atlas Fracture. J Med Stud Res 2: 010.
Copyright: © 2019 Shin-Tsu Chang, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
© 2026, Copyrights Herald Scholarly Open Access. All Rights Reserved!