
Small Bowel Anastomotic Ulcers: A Source of Iron Deficiency Anemia in Adults Detected by Capsule Endoscopy
*Corresponding Author(s):
Megan E ReindersDepartment Of Medicine, Division Of Internal Medicine, University Of California San Diego, La Jolla, United States
Tel:+1 4153423511,
Email:mreinders@ucsd.edu
Abstract
Anemia affects roughly a third of the world’s population with half of these cases being attributed to iron deficiency anemia. Gastrointestinal bleeding is the most common cause of iron deficiency anemia in patients without an obvious source of bleeding. Anastomotic or marginal ulcers are a known complication following small bowel resection and a source of chronic blood loss and anemia. However, small bowel anastomotic ulcers have only been described in the pediatric population and they have not been well defined as a source of adult obscure gastrointestinal bleeding leading to iron deficiency anemia. Here the authors report six cases of iron deficiency anemia secondary to small bowel anastomotic ulcers in adults that highlight a previously poorly described source of occult bleeding and emphasize the diagnostic benefit of video capsule endoscopy.
Keywords
ABBREVIATIONS
VCE: Video Capsule Endoscopy
OGIB: Obscure Gastrointestinal Bleeding
NSAID: Nonsteroidal Anti-Inflammatory Drugs
INTRODUCTION
Anemia affects roughly a third of the world’s population with half of these cases being attributed to Iron Deficiency Anemia (IDA) [1,2]. In the USA approximately 5-12% of women and 1-5% of men have IDA. Gastrointestinal (GI) bleeding is the most common cause of IDA in patients without an obvious source of bleeding [3,4]. A thorough examination of the gastrointestinal tract via colonoscopy and upper endoscopy is considered standard of care in the evaluation of IDA. In patients with obscure GI bleeding with negative upper and lower endoscopies, the recommendation is to proceed with an examination of the small bowel with Video Capsule Endoscopy (VCE) [5]. Up to three-quarter of patients with obscure GI bleeding have a lesion in the small intestine, defined as bleeding that occurs between the ligament of Treitz and the ileocecal valve [6]. The most common lesions responsible for small bowel bleeding are vascular (including arteriovenous malformations), with other causes being benign tumors, inflammatory lesions and lesions secondary to non-steroidal anti-inflammatory medications [7].
Anastomotic or marginal ulcers are a known complication following gastric bypass surgeries and a source of chronic blood loss and anemia [8]. However, small bowel anastomotic ulcers have only been described in the pediatric population and they have not been well defined as a source of adult obscure GI bleeding leading to IDA [9-12]. Here we present six patients with iron deficiency anemia secondary to small bowel anastomotic ulcers. In each case, other sources of anemia including abnormal uterine bleeding or nutritional deficiencies were ruled out.
CASE REPORTS
Patient 1: A 29-year-old caucasion female with a past medical history significant for lupus anticoagulant syndrome complicated by deep vein thrombosis and pulmonary embolism on anticoagulaton who was evaluated by gastroenteroloy for iron deficiency anemia and melena. She had a history of congenital intestinal obstruction and was status post partial small bowel resection in infancy, 26 years prior to her presentation with IDA. She denied Non Steroidal Anti-Inflammatory Drug (NSAID) use. Hemoglobin on presentation was 9.5 g/dL with an MCV of 73.6 um3 and a ferritin of 6 nag/mL. Initial work up included normal upper endoscopy and colonoscopy. Small bowel follow-through was negative for mass or stricture. Capsule endoscopy showed two areas of ulceration at the mid and distal small bowel at prior anastomotic sites. Subsequent double balloon enteroscopy confirmed anastomotic ischemic ulcerations in the distal jejunum and proximal ileum (Figure 1). She did not respond appropriately to oral iron supplementation and continued to have melena. Thus she was referred to surgery and underwent a segmental jejunal resection. Histopathology showed chronic mucosal ulceration and granulation tissue. 6-month follow up laboratory results were significant for hemoglobin of 14.0 g/dL, MCV 90.6 um3 and ferritin 70 ng/mL.
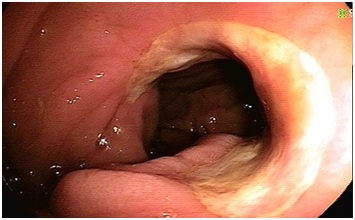 Figure 1: Anastomotic ischemic ulcerations in the distal jejunum and proximal ileum in Patient 1.
Figure 1: Anastomotic ischemic ulcerations in the distal jejunum and proximal ileum in Patient 1.
Patient 2: A 78-year-old caucasion female with a past medical history significant for type 2 diabetes mellitus and essential hypertension was evaluated by gastroenteroloy for iron deficiency anemia. She had a history of refractory bleeding ileal ulcers and had undergone anileal resection 7 years prior. She reported recent NSAID use. Hemoglobin on presentation was 6.8 g/dL with an MCV of 66.2 um3 and a ferritin of 8 ng/mL. Initial work up included un remarkable upper endoscopy, colonoscopy and computed tomography enterography. Capsule endoscopy showed erosions at the small bowel anastomosis in the distal ileum. She was treated with oral iron. Laboratory results on 6-month follow up were significant for hemoglobin of 13.5 g/dL, MCV 84.4 um3 and ferritin 91 ng/mL.
Patient 3: A 37-year-old hispanic male with a past medical history significant for HIV (CD4 351, viral load undetectable) complicated by CMV colitis, disseminated mycobacterium bovis and central nervous system toxoplasmosis was evaluated by gastroenteroloy for iron deficiency anemia. He had a history of a massive gastrointestinal hemorrhage refractory to endoscopic intervention and was status post right hemicolectomy with resection of 75 cm of the ileum and end ileostomy formation. Pathology demonstrated ulcers with CMV inclusions and granulomas containing acid-fast-bacilli. He later underwent take down of the end ileostomy with ileocolonic anastomosis two years prior to his presentation with IDA. His NSAID use is unknown. Hemoglobin on presentation was 8.5 g/dL with an MCV of 63.7 um3 and a ferritin of 4 NG/mL. Initial work up included unremarkable upper endoscopy and colonoscopy. Capsule endoscopy showed suture material in the distal ileum with surrounding ulceration at the anastomotic site (Figure 2). He was intolerant to oral iron and therefore was treated with intravenous iron. Laboratory results on 6-month follow up were significant for hemoglobin of 14.1 g/dL, MCV 85.1 um3 and ferritin 13 nag/mL.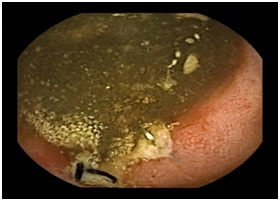 Figure 2: Suture material within the distal ileum with surrounding ulceration at the anastomotic site in Patient 3.
Figure 2: Suture material within the distal ileum with surrounding ulceration at the anastomotic site in Patient 3.
Patient 4: A 82-year-old caucasion male with a past medical history significant for essential hypertension, hyperlipidemia, type 2 diabetes mellitus and hypothyroidism was evaluated by gastroenteroloy for iron deficiency anemia. He had a history of colon cancer and had undergone colectomy with partial ileal resection. He was referred from an outside gastroenterologist and therefore much of his history is unknown. It is unknown whether he was taking NSAIDs or how long after his colectomy he developed iron deficiency anemia. Hemoglobin on presentation was 11.5 g/dL with an MCV of 98.3 um3 and a ferritin of 19 ng/mL. Initial work up included unremarkable upper endoscopy and colonoscopy. Capsule endoscopy showed ulceration at the small bowel anastomosis. He was lost to follow up after his capsule was completed.
Patient 5: A 73 year old caucasion female with a past medical history significant for essential hypertension, hyperlipidemia and type 2 diabetes mellitus was evaluated by gastroenteroloy for iron deficiency anemia. She had a history of incarcerated hernia and was status post small bowel resection. It is unknown how long after her small bowel resection she developed iron deficiency anemia. She reported recent NSAID use. Hemoglobin on presentation was 6.0 g/dL. Her MCV and ferritin are unknown. Initial work up included unremarkable upper endoscopy and colonoscopy. Capsule endoscopy showed ulceration at the small bowel anastomotic site (Figure 3). She was treated with oral iron and instructed to stop NSAID use. Laboratory results on 6-month follow up were significant for hemoglobin of 12.1 g/dL, MCV 89.7 um3 and ferritin 47 ng/mL.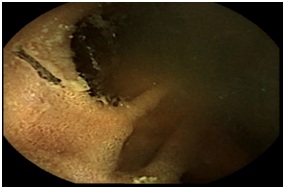
Figure 3: Ulceration in the ileum at the site of the small bowel anastomosis with suture material in Patient 5.
Patient 6: A 28 year old middle eastern male with a past medical history significant for idiopathic thrombocytopenic purapura status post splenectomy was evaluated by gastroenterology for iron deficiency anemia. He had a history of small bowel obstruction due to adhesions and had undergone an ileal resection one year prior to presentation with IDA. He reported chronic NSAID use. Hemoglobin on presentation was 7.2 g/dL with an MCV of 67 um3 and a ferritin of 4 ng/mL. Initial work up included normal upper endoscopy, colonoscopy, capsule endoscopy and single balloon enteroscopy. Repeat capsule endoscopy showed a clean-based ulcer at the small bowel anastomotic site. He was treated with intravenous iron due to poor oral iron absorption.Laboratory results on 6 month follow up were significant for hemoglobin of 10.4 g/dL with MCV 82.4 um3. Ferritin was not rechecked. Summary of the case reports is given in table 1.
| Patient | Age (yrs) | Sex (M/F) | AC Use | NSAID Use |
Indication for Resection |
Type of Resection |
Presenting Symptoms |
Time from resection to IDA (yrs) |
Presenting Hgb (g/dL), MCV (um3), Ferritin (ng/mL) |
Investigative Modalities Used |
Capsule Endoscopy Findings | Treatment | 6 Month Follow Up Hgb, MCV, ferritin |
| Patient 1 | 29 | F | Yes | No | Congenital intestinal obstruction |
Partial small bowel resection, unknown anatomy |
Anemia, Melena |
26 | Hgb 9.5, MCV 73.6, ferritin 6 | EGD, colonoscopy, push enteroscopy, small bowel follow through | Two areas of ulceration at the mid and distal small bowel at prior anastomotic sites | Jejunal Resection | Hgb 14, MCV 90.6, ferritin 70 |
| Patient 2 | 78 | F | No | Yes |
Bleeding ileal ulcers |
Ileal resection |
Anemia | 7 | Hgb 6.8, MCV 66.2, Ferritin 8 | EGD, push enteroscopy, colonoscopy, CTE | Erosions at the small bowel anastomosis in distal ileum | Oral iron | Hgb 13.5, MCV 84.4, Ferritin 91 |
| Patient 3 | 37 | M | No | Unknown |
Gastro intestinal hemorrhage |
Right hemi colectomy with resection of 75cm of ileum, end ileostomy. Then take down with ileocolonic anastomosis |
Anemia | 2 | Hgb 8.5, MCV 63.7, Ferritin 4 | EGD, colonoscopy | Suture material in distal ileum with surrounding ulceration at the anastomotic site | Intravenous iron | Hgb 14.1, MCV 85.1, ferritin 13 |
| Patient 4 | 82 | M | No | Unknown | Colon Cancer | Colectomy with partial ileal resection | Anemia | Unknown | Hgb 11.5, MCV 98.3, Ferritin 19 | Upper endoscopy, colonoscopy | Small patchy areas of possible anastomosis with ulcerated suture material seen in mid to distal ileum | Lost to follow up | Lost to follow up |
| Patient 5 | 73 | F | No | Yes | Incarcerated Hernia | Small bowel resection | Anemia | Unknown | Hgb 6. No other data available | EGD, colonoscopy | Ulceration seen at small bowel anastomosis | Oral iron, discontinue NSAIDs | Hgb 12.1, MCV 89.7, Ferritin 47 |
| Patient 6 | 28 | M | No | Yes | Small bowel obstruction due to adhesions | Ileal resection | Anemia | Unknown | Hgb 7.2, MCV 67, Ferritin 4 | EGD, colonoscopy, SBE, VCE | Clean based ulcer at small bowel anastomosis distal to pylorus | Intravenous Iron, discontinue NSAIDs | Hgb 10.4, MCV 82.4, no repeat ferritin |
Table 1: Summary of patient characteristics, capsule endoscopy findings and follow up.
*AC: Anticoagulation; NSAID: Nonsteroidal Anti-Inflammatory Drugs; EGD: Esophagogastroduodenoscopy; Hgb: Hemoglobin; MCV: Mean Corpuscular Volume; VCE: Video Capsule Endoscopy; SBE: Single Balloon Enteroscopy; CTE: Computed Tomography Enterography,; IDA: Iron Deficiency Anemia
DISCUSSION
The American College of Gastroenterology (ACG) guidelines recommend a thorough upper endoscopy and colonoscopy evaluation for patients with iron deficiency anemia. If no source of bleeding is found, examination of the small bowel with VCE is recommended as long as there are no concerns for possible small bowel obstruction which could lead to capsule retention. Capsule endoscopy is currently the initial test of choice if repeat endoscopy is not warranted. If capsule endoscopy shows a bleeding source, subsequent investigation with push or deep/balloon assisted enteroscopy may be needed depending on the finding [13].
End-to-end small bowel anastomotic ulcers identified via capsule endoscopy have not been well described in the literature as a source of IDA in adults. Although previous literature has demonstrated the existence of several cases of chronic iron deficiency anemia in adults with history of side-to-side small bowel anastomoses, these sources of bleeding were identified during exploratory laparotomy or colonoscopy [12,14]. The pathophysiology behind anastomotic ulcers involves ischemia due to sutures, the tension of the anastomosis, or an inflammatory response to the materials used during anastomosis [15].
This small case series highlights an unusual source of occult bleeding that has yet to be well described and emphasizes the diagnostic benefit small bowel capsule endoscopy in the evaluation of iron deficiency anemia. These techniques are especially important in the evaluation of anastomotic sites outside the reach of traditional upper endoscopy and colonoscopy since anastomotic ulcers many times cannot be visualized on other modalities such as CT or MR enterography. By finding the bleeding source in these patients with VCE, further studies including repeat upper endoscopy, colonoscopy or enterography can be avoided which also has significant impact on cost.
Of note, despite the history of small bowel surgery in these patients, there were no complications of capsule endoscopy, including no reports of capsule retention. If there is concern about small bowel patency, a radiological study such as CT versus MR enterography can be performed prior to capsule endoscopy. In patients with iron deficiency anemia and a history of small bowel surgery, capsule endoscopy is useful in determining whether a small bowel source is causing blood loss and contributing to anemia. In addition, anastomotic ulcers should be considered as a source of bleeding in patients who present with iron deficiency anemia and a history of bowel resection.
CONFLICT OF INTEREST
The authors whose names are listed immediately below certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
AUTHOR CONTRIBUTIONS
Megan E Reinders: Study concept and design, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript, approved final submission.
Albert Ding: Drafting of the manuscript, critical revision of the manuscript, approved final submission.
Denise Kalmaz: Study concept and design, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript, study supervision, approved final submission.
All authors approved the final version of this article.
INFORMED CONSENT
Informed consent was obtained for case publication.
REFERENCES
- Gasche C, Lomer MC, Cavill I, Weiss G (2004) Iron, anaemia, and inflammatory bowel diseases. Gut 53: 1190-1197.
- Lopez A, Cacoub P, Macdougall LC, Peyrin-Biroulet L (2016) Iron deficiency anaemia. Lancet 387: 907-916.
- Rockey DC, Cello JP (1993) Evaluation of the gastrointestinal tract in patients with iron-deficiency anemia. N Engl J Med 329: 1691-1695.
- Bosch X, Montori E, Guerra-García M, Costa-Rodríguez J, Quintanilla MH, et al. (2017) A comprehensive evaluation of the gastrointestinal tract in iron-deficiency anemia with predefined hemoglobin below 9 mg/dL: A prospective cohort study. Dig Liver Dis 49: 417-426.
- Enns RA, Hookey L, Armstrong D, Bernstein CN, Heitman SJ, et al. (2017) Clinical Practice Guidelines for the Use of Video Capsule Endoscopy. Gastroenterology 152: 497-514.
- Pasha SF, Leighton JA, Das A, Harrison ME, Decker GA, et al. (2008) Double-balloon enteroscopy and capsule endoscopy have comparable diagnostic yield in small-bowel disease: A meta-analysis. Clin Gastroenterol Hepatol 6: 671-676.
- Gunjan D, Sharma V, Rana SS, Bhasin DK (2014) Small bowel bleeding: A comprehensive review. Gastroenterol Rep (Oxf) 2: 262-275.
- Csendes A, Burgos AM, Altuve J, Bonacic S (2009) Incidence of marginal ulcer 1 month and 1 to 2 years after gastric bypass: a prospective consecutive endoscopic evaluation of 442 patients with morbid obesity. Obes Surg. 19: 135-138.
- Bass LM, Zimont J, Prozialeck J, Superina R, Cohran V (2015) Intestinal Anastomotic Ulcers in Children With Short Bowel Syndrome and Anemia Detected by Capsule Endoscopy. J Pediatr Gastroenterol Nutr 61: 215-219.
- Goldszmidt D, Duche M, Gauthier F (1994) [Small intestine ulcers 12 years after ileosigmoid anastomosis for neonatal necrotizing enterocolitis]. Arch Pediatr 1: 1011-1013.
- Sondheimer JM, Sokol RJ, Narkewicz MR, Tyson RW (1995) Anastomotic ulceration: a late complication of ileocolonic anastomosis. J Pediatr 127: 225-230.
- Chari ST, Keate RF (2000) Ileocolonic anastomotic ulcers: a case series and review of the literature. Am J Gastroenterol 95: 1239-1243.
- Gerson LB, Fidler JL, Cave DR, Leighton JA (2015) ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding. Am J Gastroenterol 110: 1265-1287.
- Alekseev GI, Veretnik GI, Archvadze VG, Baranovich VIu (1989) [Intestinal side-to-side anastomosis as a cause of iron deficiency anemia]. Khirurgiia (Mosk) 101-103.
- Wilson JA, Romagnuolo J, Byrne TK, Morgan K, Wilson FA (2006) Predictors of endoscopic findings after Roux-en-Y gastric bypass. Am J Gastroenterol 101: 2194-2199.
Citation: Reinders ME, Ding A, Kalmaz D (2018) Small Bowel Anastomotic Ulcers: A Source of Iron Deficiency Anemia in Adults Detected by Capsule Endoscopy. J Clin Stud Med Case Rep 5: 054.
Copyright: © 2018 Megan E Reinders, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

