
Sonographic Examination two Weeks after Medical Termination of Pregnancy - What is the Benefit?
*Corresponding Author(s):
Aya Mohr-SassonDepartment Of Obstetrics And Gynecology, Sheba Medical Center, Tel-Hashomer, Israel
Tel:+972 523692906,
Fax:972 35302922
Email:mohraya@gmail.com
Abstract
Purpose: Follow-up evaluation after medical abortion is required to diagnose and treat complications, including ongoing pregnancy. We aimed to evaluate the yield of transvaginal ultrasonography performed two weeks treatment.
Methods: A retrospective cohort study, including all women up to 49 days of amenorrhea that underwent medical termination of pregnancy at a single medical center between January 2011 to January 2018. Treatment protocol included mifepristone (600 mg orally) followed by misoprostol (400 μg orally) 48 hours later. Follow up was two weeks after mifepristone administration and included transvaginal ultrasonography. Data were collected from women's medical files.
Results: During the study period 807 women underwent medical abortion, of them 82% (n=662) had documented sonographic examination. Normal examination was reported in 20.7% (n=137) of the women. In 48.0 % (n=318) a residua was suspected and in another 16.0% (n=106) endometrium was measured above 15 mm. Recommendation was given to 7.4% (n=60), 3.6% (n=29) and 0.7% (n=6) of the women, for further treatment with misoprostol, curettage and hysteroscopy, respectively. Second ultrasound examination after menstruation (or up to 2-4 weeks from the first examination), was recommended to 64.9% (n=430/662) of the women, with complete follow up in 372/430 (86.5%). Normal evaluation was almost three times higher in the second ultrasound examination compared to the first (56.4%, n=210/372).
Conclusion: Fifth of the women undergoing medical termination of pregnancy might benefit from early ultrasound examination. Nevertheless, it cannot predict failure of treatment due to high probability for normal ultrasound examination 2-4 weeks from the first.
Key Massage
Post medical abortion ultrasound follow up, should be deferred to after menstruation unless early intervention is required.
Introduction
Medical management of first trimester abortion is a standard method of providing abortion care worldwide [1]. Medical abortion, which involves the use of medications rather than a surgical procedure to induce an abortion, is an option for women who wish to terminate a first-trimester pregnancy [2-4]. Different agents and regiments are used for the induction of abortion mostly including prostaglandins (prostaglandin E1 analogue), mifepristone (progesterone receptor antagonist), methotrexate, mifepristone with prostaglandins and methotrexate with prostaglandins [4]. In a meta-analysis published by the Cochrane, the combined treatment was proven more effective compared to the use of a single agent [4]. The FDA approved treatment with mifepristone in a regimen with misoprostol, to end a pregnancy through 70 days gestation. This non-surgical treatment for pregnancy termination was found convenient, effective, and safe, with approximately 96-98% success rate in gestations of up to 42 days, and 91-95% in gestations up to 49 days [3,5]. The need for surgical evacuation following medical abortion varies according to gestational age and regimen used, and is estimated less than 5% [6].
Follow-up evaluation after medical abortion is required to diagnose and treat complications, including ongoing pregnancy [7]. The FDA-approved regimen includes an evaluation at 14 days after mifepristone administration to assess for bleeding and evidence of uterine involution on pelvic examination. Diverse methods of follow-up are considered acceptable including: 1. in-clinic transvaginal ultrasound examination 1or 2 weeks after treatment; 2. serum Human Chorionic Gonadotropin (hCG) level measurement before and 1 week after treatment; and 3. telephone follow-up at 1 week, with subsequent urine pregnancy testing at 2 weeks or 4 weeks after treatment [8,9].
Transvaginal ultrasonography two weeks after mifepristone administration is the method of choice in our medical center, primarily because it provides a definitive assessment of whether or not the products of conception have been expelled [10]. This method poses a challenge for practitioners, due to the fact that after surgical or spontaneous expulsion, uterus containing blood, blood clots, and decidua seen as hyperechoic signal on ultrasound evaluation is considered normal [11]. Rarely does this finding in women who have undergone medical abortion indicate a need for intervention. Previous studies found that measurement of endometrial thickness or other findings a week following treatment was not a predictor of the need for future surgical intervention [10,12]. Nonetheless, in practice, care givers tend to recommend additional intervention when follow-up ultrasound scan is inconclusive or show a large volume of heterogeneous material in the uterus even when symptoms are minimal. Incorrect interpretation of ultrasound examination results, may lead to unnecessary intervention and great emotional stress for the patients. Due to the aforementioned, we aimed to evaluate the yield of transvaginal ultrasonography performed two weeks after medical Termination Of Pregnancy (TOP) and the need for further follow-up.
Materials and Methods
This is a retrospective cohort study, including all women with amenorrhea up to 49 days, that underwent medical termination of pregnancy at a single tertiary university affiliated medical center, between January 2011 to December 2017. Transvaginal ultrasound was mandatory before the beginning of the treatment to confirm a viable intrauterine pregnancy. All patients received approval from the hospital’s “Pregnancy Termination Approval Committee” and provided a written informed consent for the medical pregnancy termination. The treatment protocol included a dose of mifepristone (600 mg orally) followed by misoprostol (400 μg orally) 48 hours later and is in concordance to the FDA approved protocol. Women that did not complete the treatment regime for medical abortion accepted in our medical center, were excluded from the study.
Management was ambulatory. Women were requested to complete vaginal sonographic examination 14 days after mifepristone administration at the ultrasound unit in our department. Examinations were documented in patients' medical files, and evaluated by the attending physician in order to determine further management, that included : 1- No need for further follow up - when ultrasound examination revealed a well-defined endometrial line, with a maximum thickness of <15 mm, combined with absence of vaginal bleeding. In these cases, complete abortion was diagnosed according to the guidelines from the Royal College of Obstetricians and Gynecologists for spontaneous abortions [13] ; 2- Second ultrasound examination after menstruation ( or up to 2-4 weeks from the first examination ) - when endometrial thickness was measured ≥15 mm and/or focal intrauterine hyperechogenic shadows in the presence of irregular endometrium were suspected for retained product of conception; 3- additional intervention ( misoprostol 400 micrograms (PO/PR) , hysteroscopy or dilatation and curettage ) - usually in cases where a gestational sac was still observed or cases with profound bleeding or signs of suspected infection.
Demographics, sonographic findings recommendation and further intervention were collected from patients’ medical files. The study protocol was approved by the “Sheba Medical Center” ethical committee Review Board (ID 7122-20 -SMC) on the 27 of April 2020. Due to the retrospective design of the study informed consent statement was not requested by the ethical committee.
Statistical analysis
Normality of the data was tested using the Shapiro-Wilk or Kolmogorov-Smirnov tests. Data are presented as median and Inter-Quartile Range (IQR). Comparison between unrelated variables was conducted with Student’s t-test or Mann-Whitney U test, as appropriate. The chi-square and Fisher’s exact tests were used for comparison between categorical variables. Significance was accepted at p < 0.05. Statistical analyses were conducted using the IBM Statistical Package for the Social Sciences (IBM SPSS v.19; IBM Corporation Inc, Armonk, NY, USA).
Patient and public involvement
How was the development of the research question and outcome measures informed by patients’ priorities, experience, and preferences? Based on women's' experience and desire for information regarding the success rate during the process of treatment, we aimed in this study to summarize our results to better consult women undergoing treatment and meet expectations.
How did you involve patients in the design of this study? This is a retrospective study. Were patients involved in the recruitment to and conduct of the study? Due to study design, patients were not involved in the recruitment or the conduction of the study. How will the results be disseminated to study participants? Results will be published and available to anyone seeking this information.
Results
During the study period 807 women underwent medical abortion, of them 82% (n=662) had documented follow up visit including sonographic examination findings (Figure 1). Women’s demographics and clinical characteristics are presented in table 1. Mean Women’s age was 27.4 (±7.7 SD) years and mean gestational age was 40.0 (±2.15 SD) days. Mean time for first sonographic examination after mifepristone administration was 17.3 (±5.97 SD) days. Sonographic findings are summarized in table 2. Normal ultrasound examination was documented in fifth of the women (n=134/662). Gestational sac was observed in 5.9%. In 48.0% (n=318) pregnancy rests ( residua) were suspected and in another 16.0% (n=106) endometrium was measured ≥ 15 mm. Based on the following findings, recommendation for further treatment with misoprostol, curettage and hysteroscopy was given to 9.1% (n=60), 3.6% (n=29) and 0.7% (n=5) of the women, respectively (Table 3).
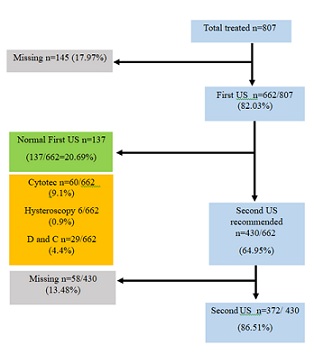 Figure 1: Study population.
Figure 1: Study population.
|
|
n |
% |
Mean |
±SD |
Minimum |
Maximum |
|
Age (years) |
27.38 |
7.70 |
14 |
47 |
||
|
Gestational age (days) |
40.00 |
2.15 |
21 |
49 |
||
|
Gravidity |
2.34 |
2.01 |
1 |
13 |
||
|
Parity |
0.87 |
1.45 |
0 |
8 |
||
|
Abortion |
0.22 |
0.71 |
0 |
5 |
||
|
Regular menses |
309 |
38.86 |
||||
|
Past TOP |
111 |
13.96 |
||||
|
First US from mifepristone (days) |
662 |
17.27 |
5.97 |
1 |
68 |
|
|
Second US from mifepristone (days) |
372 |
54.33 |
30.73 |
7 |
335 |
Table 1: Women's demographics and clinical characteristics.
TOP- Termination of pregnancy, US - Ultrasound
|
First US (n=662) |
Second US (n=372) |
|||
|
n |
% |
n |
% |
|
|
Normal US |
137 |
20.24 |
210 |
56.45 |
|
Endometrium (≥15mm) |
106 |
16.01 |
23 |
6.18 |
|
Gestational sac |
20 |
3.02 |
3 |
0.81 |
|
Fetus |
19 |
2.87 |
1 |
0.03 |
|
Residua |
318 |
48.03 |
142 |
38.17 |
Table 2: Sonographic findings.
|
First US(n=662) |
Second US(n=372) |
|||
|
n |
% |
n |
% |
|
|
No further follow up |
137 |
20.69 |
210 |
58.6 |
|
US after menses |
430 |
53.02 |
43 |
5.3 |
|
Misoprostol |
60 |
7.4 |
6 |
0.7 |
|
Hysteroscopy |
6 |
0.7 |
106 |
13.1 |
|
D and C |
29 |
3.6 |
7 |
0.9 |
|
Total |
662/807 |
83.06 |
372/430 |
86.51 |
Table 3: Recommendations following ultrasound examinations.
US - Ultrasound, D and C - Dilatation & Curettage
Second sonographic examination after menstruation or up to 2-4 weeks from the first ultrasound follow up examination, was recommended to 64.9% (n=430) of the women, of them 372 (86.5%) women completed examination (Figure 1). Normal evaluation was almost three times higher compared to the first examination (56.5%, n=210) (Table 2). Altogether, 52.41% (n=347) women had successful medical abortion based on normal ultrasound findings on first or second examination.
Hysteroscopy was recommended to 112/662 (16.9%) women, of them 94.6% after the second ultrasound examination. For 29 women we did not have the hysteroscopic or the pathology documentation, therefore complete follow was achieved in 74.11% (n=83). Histo-pathological report confirmed pregnancy rests in 95.18% (n=83) of the cases.
Discussion
Principle findings
Our study revealed the following findings: 1. Early ultrasound examination performed two weeks after medical termination of pregnancy will reveal a complete abortion with no need for further treatment or follow up in fifth of the women; 2. Early ultrasound examination cannot predict failure of treatment due to the high probability that following menstruation a normal ultrasound examination will be observed; 3. Hysteroscopy completed after failure of medical abortion defined by ultrasound, has high positive predicting value; 4. Total lost to following our study reached 25%.
Clinical implications
Vaginal ultrasound is the preferred method for follow up after medical pregnancy termination in our medical center. Determining the perfect timing for the examination should balance between the will to assure women as early as possible while avoiding unnecessary exams and interventions. The results of our study demonstrate 21% normal ultrasound findings after two weeks from mifepristone treatment. This finding is reassuring in a usually very inconvenient stressogenic situation, for fifth of the women undergoing medical abortion, after a short period from treatment, and long time before the preceding menstruation [14,15]. It might be that the shorter duration of the process reduces the negative psychological effect of the abortion [15].
On the other hand, any finding on early sonographic evaluation (that most probably will disappear after menstruation), could also be emotionally disturbing, and furthermore, lead to unnecessary medical interventions [14,16]. Studies concerning the acceptable follow up method and timing after medical abortion have emerged, aiming to simplifying the process for women [11,17-19]. The use of ultrasound after 14 days or after menstruation for follow-up after medical abortion, has been questioned mainly due to the need for additional in-clinic visit. According to the FDA approved regimen, an evaluation should be completed 14 days after mifepristone administration. Only if clinical history and physical examination do not confirm expulsion, ultrasonography is recommended. In a meta-analysis conducted by Baiju et al., [20] including four randomized controlled trials (RCT s; n = 5493), no significant difference were found in complete abortion rates between self-assessment and routine clinic follow up (RR = 1.00, 95% CI 0.99-1.01). The ongoing pregnancy rates were similar and the pooled results for the safety outcomes showed no significant differences between the groups. Schmidt-Hansen et al., [21] report similar findings in a meta- analysis including four randomized controlled trials (n = 5761) that compared in-clinic to remote self-assessment. They concluded that the published data support offering women who have had a medical abortion, up to and including 10+0 weeks’ gestation, the choice of self-assessment, remote assessment, or clinic follow-up.
In contrary to the aforementioned, the benefits of sonographic evaluation performed after menstruation has been demonstrated by Machtinger et al., [11] in a cohort of 191 women who underwent medical abortion and completed transvaginal sonography. Suspected products of gestation by transvaginal ultrasound were found in 3.7% of the asymptomatic women, and residual products of gestation were diagnosed by hysteroscopy in 85.7% having high potential for future gynecological and fertility outcomes [22,23]. A study conducting sonographic evaluation 2 weeks from initial treatment for medical abortion was conducted by Amer-Alshiek et al., [17]. The study included 301 women, of them in 236 (78.40%) ultrasound findings were negative and in 66 it was suspicious. This rate declined as the interval between ultrasound evaluation and first medical treatment increased (up to 10 weeks). They concluded that at 2 weeks after medical abortion, ultrasound findings suspicious for retained products of conception do not conclusively indicate failure of the procedure. Ultrasound evaluation should be repeated 4-6 weeks later (6-8 weeks after medical abortion) in women with suspected residua before diagnosing failure of the procedure.
Our results are in concordance with previous studies questioning the need for ultrasound evaluation after 2 weeks from mifepristone treatment due to substantial higher success rate while postponing the ultrasound examination. Early evaluation should be preserved for women with abnormal presentation (large uterus, profound bleeding or suspected infection). Nevertheless, providing women the information regarding the possible findings on early ultrasound evaluation and allowing them to be involved in decision making might be beneficial from psychologic point of view.
Our study revealed that hysteroscopy performed after failure of medical abortion defined by ultrasound, has high positive predicting value. 94.6% (106/112) of hysteroscopy examinations recommended were after the second ultrasound evaluation, mainly after menstruation, making the diagnosis of retained product of conception more accurate. Performing this intervention at the proper timing maximizes its efficiency. Amer-Alshiek et al., [17] and Machtinger et al., [11] reported similar results: In 15/18 (83.3%) and in 85.7% women, respectively, residua was found when hysteroscopy/curettage was performed due to abnormal ultrasound scan following medical abortion.
Unfortunately, albeit the fact that we advise to wait for post menstrual ultrasound before further treatment, 13.4% of our patients underwent further treatment based on the findings in the early scan. One must acknowledge that premature treatment is a hazard of early scan. Another challenge in post medical abortion practice is patient adherence to follow up. In light of the significant failure rate of medical compared to surgical abortion, follow up should be strongly encouraged [24]. However, in-person post-abortion follow-up visits are expensive, inconvenient to the patients, and not mandatory for detection of complications [24]. Initial reports showed that when patients are required to go to a facility for assessment of medical abortion outcome, approximately 25% lost to follow-up is expected [8,25]. Further reports in the clinical setting reach loss-to-follow-up rates as high as 45% [24].
Our study adhere with previous findings reporting lost to follow up rate of 25% (203/807 women) (Figure 1). First follow-up completed from medical files reached only 64.7% (522/807). Additional telephone calls were made in order to maximize the accuracy of our data, with additional information achieved for 82 women with no in-clinic documentation (604/807=75%). In order to improve adherence to follow up, alternative options for follow-up examination after medical abortion have been proposed aiming to reduce in-patient visits- among them Serum hCG testing. Serum hCG level decrease of at least 80% over 6-7 days after initiating treatment with mifepristone and misoprostol indicates a successful abortion [18]. A study comparing follow-up rates for women that chose ultrasound examination or hCG testing, revealed loss-to-follow-up rate higher among women who chose hCG testing (33.7% versus 22.9%; p=0.02) [26]. Rørbye et al., [26], compared ultrasonography and a βhCG measurement in monitoring the outcome of medical abortion in a clinical setting (15 days from treatment), and rejected each one of them as the single method for post-procedure evaluation. Our findings suggests the need for alternative follow up regime that will enable safe management, however, will be more convenient to adhere. A solely one ultrasound examination performed 4-5 weeks from medical termination of pregnancy or after menstruation, with the exception of cases with abnormal bleeding or signs of infection, might improve patients compliance and be in better timing for decision making regarding the need for further interventions.
Limitation and Strength
The study has limitations that need to be acknowledged. This is a retrospective study. The observational design limits our ability to infer a causal relationship between ultrasound findings two weeks from the beginning of the medical treatment to successful TOP. The fact that 13% of patients underwent treatment after the first scan also obscures results. Furthermore, lack of documentation in part of the women's follow up, might also introduced a recall bias. Our study has merits that should be mentioned. This study includes large cohort. All women were treated by the same protocol, in a single medical center and evaluated by the same team. Moreover, follow-up rate achieved was relatively high due to telephone survey conducted in cases of missing data, strengthening the external validity of our findings. We assume that the success rate reported in our study is probably underestimation presuming that women lost to follow up (145 and 58 women, before first and second ultrasound examination, respectively) abstained additional in- hospital visit due to favorable outcome.
Conclusion
Ultrasound evaluation two weeks after medical abortion in women with suspect findings cannot predict failure of treatment and can lead to unnecessary interventions. Post medical abortion ultrasound follow up, should be deferred to after menstruation unless early intervention is required due to hemodynamic instability or lack of any bleeding following treatment. In cases of high psychological stress, it is reasonable to assess two weeks from treatment due to the potential of completing abortion process in fifth of the women, and by that reducing anxiety. This information should be of value to physicians and patients alike. Further randomized prospective studies should be done comparing outcomes following single late ultrasound examination to the common practice today to strengthen our findings.
Disclosure
The authors report no conflict of interest.
Ethical Approval
The study protocol was approved by the “Sheba Medical Center” ethical committee Review Board (ID 7122-20 -SMC) on the 27 of April 2020.
Funding
The authors received no specific funding for this work.
References
- Sedgh G, Henshaw SK, Singh S, Bankole A, Drescher J (2007) Legal abortion worldwide: Incidence and recent trends. Int Fam Plan Perspect 33: 106-116.
- Blanchard K, Shochet T, Coyaji K, Thi Nhu Ngoc N, Winikoff B (2005) Misoprostol alone for early abortion: An evaluation of seven potential regimens. Contraception 72: 91-97.
- Spitz IM, Bardin CW, Benton L, Robbins A (1998) Early pregnancy termination with mifepristone and misoprostol in the United States. N Engl J Med 338: 1241-1247.
- Kulier R, Kapp N, Gülmezoglu AM, Hofmeyr GJ, Cheng L, et al. (2011) Medical methods for first trimester abortion. Cochrane Database Syst Rev 2011: CD002855.
- Aubény E, Peyron R, Turpin CL, Renault M, Targosz V, et al. (1995) Termination of early pregnancy (up to 63 days of amenorrhea) with mifepristone and increasing doses of misoprostol [corrected]. Int J Fertil Menopausal Stud 2: 85-91.
- Raymond EG, Shannon C, Weaver MA, Winikoff B (2013) First-trimester medical abortion with mifepristone 200 mg and misoprostol: A systematic review. Contraception 87: 26-37.
- Henshaw RC, Naji SA, Russell IT, Templeton AA (1994) A comparison of medical abortion (using mifepristone and gemeprost) with surgical vacuum aspiration: Efficacy and early medical sequelae. Hum Reprod 9: 2167-2672.
- Dayananda I, Maurer R, Fortin J, Goldberg AB (2013) Medical abortion follow-up with serum human chorionic gonadotropin compared with ultrasonography: A randomized controlled trial. Obstet Gynecol 121: 607-613.
- Grossman D, Grindlay K (2011) Alternatives to ultrasound for follow-up after medication abortion: A systematic review. Contraception 83: 504-510.
- Reeves MF, Fox MC, Lohr PA, Creinin MD (2009) Endometrial thickness following medical abortion is not predictive of subsequent surgical intervention. Ultrasound Obstet Gynecol 34: 104-109.
- Machtinger R, Seidman DS, Goldenberg M, Stockheim D, Schiff E, et al. (2005) Transvaginal ultrasound and operative hysteroscopy in women undergoing medical termination of pregnancy as a part of routine follow-up. Fertil Steril 84: 1536-1538.
- Cowett AA, Cohen LS, Lichtenberg ES, Stika CS (2004) Ultrasound evaluation of the endometrium after medical termination of pregnancy. Obstet Gynecol 103: 871-875.
- Luise C, Jermy K, May C, Costello G, Collins WP, et al. (2002) Outcome of expectant management of spontaneous first trimester miscarriage: Observational study. BMJ 324: 873-875.
- Attali L (2016) [Psychological aspects of abortion]. J Gynecol Obstet Biol Reprod (Paris) 45: 1552-1567.
- Whitney DK (2017) Emotional Sequelae of Elective Abortion: The Role of Guilt and Shame. J Pastoral Care Counsel 71: 98-105.
- Society of Family Planning Clinical Guideline (2014) Medical management of first-trimester abortion. Contraception 89: 148-161.
- Amer-Alshiek J, Shiekh O, Agmon A, Grisaru D (2015) What is the right timing for ultrasound evaluation after pregnancy termination with mifepristone? Eur J Obstet Gynecol Reprod Biol 189: 24-26.
- Fiala C, Safar P, Bygdeman M, Gemzell-Danielsson K (2003) Verifying the effectiveness of medical abortion; ultrasound versus hCG testing. Eur J Obstet Gynecol Reprod Biol 109: 190-195.
- Whaley NS, Burke AE (2015) Update on medical abortion: Simplifying the process for women. Curr Opin Obstet Gynecol 27: 476-481.
- Baiju N, Acharya G, D'Antonio F, Berg RC (2019) Effectiveness, safety and acceptability of self-assessment of the outcome of first-trimester medical abortion: A systematic review and meta-analysis. BJOG 126: 1536-1544.
- Schmidt-Hansen M, Cameron S, Lohr PA, Hasler E (2020) Follow-up strategies to confirm the success of medical abortion of pregnancies up to 10 weeks' gestation: A systematic review with meta-analyses. Am J Obstet Gynecol 222: 551-563.
- Guarino A, Di Benedetto L, Assorgi C, Rocca A, Caserta D (2015) Conservative and timely treatment in retained products of conception: A case report of placenta accreta ritention. Int J Clin Exp Pathol 8: 13625-13629.
- Hooker AB, Aydin H, Brölmann HA, Huirne JA (2016) Long-term complications and reproductive outcome after the management of retained products of conception: A systematic review. Fertil Steril 105: 156-164.
- Haimov-Kochman R, Arbel R, Sciaky-Tamir Y, Brzezinski A, Laufer N, et al. (2007) Risk factors for unsuccessful medical abortion with mifepristone and misoprostol. Acta Obstet Gynecol Scand 86: 462-466.
- Horning EL, Chen BA, Meyn LA, Creinin MD (2012) Comparison of medical abortion follow-up with serum human chorionic gonadotropin testing and in-office assessment. Contraception 85: 402-407.
- Rørbye C, Nørgaard M, Nilas L (2004) Prediction of late failure after medical abortion from serial beta-hCG measurements and ultrasonography. Hum Reprod 19: 85-89.
Citation: Mohr-Sasson A, Shats M, Key C, Meyer R, Mashiach R, et al. (2022) Sonographic Examination two Weeks after Medical Termination of Pregnancy - What is the Benefit? J Reprod Med Gynecol Obstet 7: 096.
Copyright: © 2022 Aya Mohr-Sasson, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

