Sperm Motility and Morphology is Affected by Body Mass Index
*Corresponding Author(s):
William E RoudebushDepartment Of Biomedical Sciences, University Of South Carolina School Of Medicine Greenville, South Carolina, United States
Email:ROUDEBUS@greenvillemed.sc.edu
Abstract
Objective
No one semen parameter, (e.g. sperm motility or morphology) has been found to be highly diagnostic of male sub fertility. Previously we reported that Sperm Motility Index (SMI) can describe sperm motility more specifically than a sperm cell being simply motile or non-motile. SMI has been shown to have a positive association with IUI pregnancy outcomes. Additionally, Body Mass Index (BMI) has been reported to have a significant relationship with semen parameters, however no data is available associating BMI with sperm motility index and sperm morphology. The study determined if BMI impacts the sperm motility index with morphology incorporated into the algorithm.
Design
Retrospective cohort study in male patients undergoing a semen analysis in a tertiary fertility clinic.
Materials and Methods
Semen samples were assessed which included the following patient values: Weight (M) and weight (Kg), semen volume, sperm concentration, percent sperm motility, percent sperm morphology (normal forms). Sperm Motility-Morphology Index (SM2I) was calculated as follows: SM2A = (percent motility*sperm progression*morphology percent).
Results
Semen samples from 53 men assessed as described with a mean BMI of 27.5 and a mean SM2A of 8.9. Regression analysis showed a significant (P<0.05) relationship between BMI and the SM2A.
Conclusion
This study further collaborates that an increased body mass index will have a negative impact on the sperm motility and sperm morphology as shown via a novel algorithm. Additional research is warranted to see how this association between BMI and SM2A impacts pregnancy outcomes.
Keywords
INTRODUCTION
As the prevalence of obesity continues to rise, so does its impact on the health of the population and cost to the medical community. Surpassing both smoking and diabetes as the leading cause of preventable death in the United States, treatment of obesity and obesity-related disease was estimated to cost over $190 billion in 2012 [1]. Recently, there has been a surge of interest in the relationship of obesity with male factors of fertility. The most widely accepted studies investigating male-factor fertility have suggested an 1.1-1.4-fold increased risk in sub/infertility in overweight and obese males, often showing a dose-response relationship [2]. Sallmen et al., found that weight gain as small as a three unit increase in Body Mass Index (BMI) is associated with infertility [3]. Elevated BMI in men is strongly correlated with several physiologic pathways that play a role in fertility such as hormonal regulation, hypogonadism, and semen parameters [4]. Sperm collected from obese men used for in vitro fertilization has been associated with a greater number of pregnancy losses and is less likely to result in live births [5]. Furthermore, evidence has shown improvement in sexual function, semen parameters, and pregnancy rates in males following significant reduction in BMI [4,6,7].
Semen analysis has been the longstanding clinical tool for measuring semen parameters and is regularly used to evaluate male partners of infertile couples. In 2010 the World Health Organization (WHO) released an updated assessment of semen parameter reference ranges to help predict male fertility and pregnancy outcomes of couples [8]. When comparing semen quality of obese men to the general population, studies have shown that men with higher BMIs show a significantly decreased semen volume and total sperm count, but no impact was seen in sperm concentration, motility, morphology, or DNA fragmentation index [9]. However, these studies have failed to show reproducibility leaving the exact underlying mechanisms of obesity’s role in infertility largely unknown [10,11].
One of the most useful purposes of analyzing semen is for predicting pregnancy outcomes of Intrauterine Insemination (IUI). IUI has been a first-line treatment for the treatment of infertility for several decades, but reported pregnancy rates following treatment with IUI have varied tremendously from 5% to 62% [12,13]. Much of this variation is a direct result of the various techniques and protocols for semen preparation and insemination, but some of it can be contributed to the imperfect WHO reference ranges and semen parameter analysis. Because the WHO reference range values of semen parameters frequently fail strict clinical and statistical standards, they are consistently under scrutiny for reconsideration [14]. Likewise, novel semen criteria and algorithms are being devised and studied to find a more reliable and diagnostic standard for predicting fertility rates.
Although clinicians routinely use semen analysis to predict pregnancy outcomes, there is no single standard or combination of parameters that is diagnostic of infertility. Motility has been a primary focus for many fertility improving treatments due to a strong link found between motile sperm and pregnancy outcomes [15]. IUI attempts to functionally increase the number of motile spermatocytes by shortening the distance that sperm must travel to the oviduct to reach the site of fertilization. Historically, motility was determined as a binary value and was classified as either “motile” or “nonmotile” without consideration of linearity or velocity, but advancements in technology and technique have attempted to quantify motility more accurately. Sperm Motility Index (SMI) is a novel semen parameter that utilizes a Computer-Assisted Semen Analyzer (CASA) to objectively categorize sperm motility based on an individual sperm’s curvilinear velocity. Thus far, SMI has not been successful in showing a significant relationship between motility and pregnancy [16].
Sperm morphology is another semen parameter that has been strongly implicated in predicting pregnancy outcomes. Although abnormal sperm morphology has long been associated with infertility, the failure to standardize morphologic evaluation among researchers has led to high variability in its reporting [17]. Development of the Tyberg strict criteria and the 2010 WHO sperm parameter update have attempted to minimize this variation, yet morphology by itself has not been found to be sensitive or specific enough for diagnosing infertility [18,19]. More recent steps in semen analysis have combined multiple semen parameters into algorithms to more accurately predict pregnancy outcomes in previously infertile couples. The goal of this study is to combine morphology parameters into SMI calculations to create the Sperm Motility-Morphology Algorithm (SM2A) in order to determine whether an impact of BMI onto fertility can be measured.
METHODS
Study population and participants
Semen samples from 53 men were analyzed per WHO 5th edition (2010).
Measurement
The data collected included height (m), and weight (kg), body mass index was calculated as follows: BMI = (weight/height2). Sperm morphology was analyzed using the strict criteria per WHO 2010 (5th edition). Sperm motility with forward progression was determined via a computer assisted semen analyzer (Sperm Class Analyzer; Version 5.1, Microptics. I., Barcelona, Spain). Forward progression was categorized as follows:
- Category 4: Rapid, >35 µ/sec
- Category 3: Medium, 15-35 µ/sec
- Category 2: Slow, 10-14 µ/sec
- Category 1: Static/twitching <10 µ/sec
The Sperm Motility-Morphology Algorithm (SM2A) was calculated as follows:
SM2A = (motility*progression category*morphology percent)
STATISTICAL ANALYSIS
Regression analysis (Sigma Plot for Windows v14.0 Build 14.0.1.142, Systat Software, Inc., GmbH, Germany) was performed compared BMI and SM2Avalues.
Ethics approval and consent to participate
Research approval was granted by the Institutional Review Board (IRB) of the University of South Carolina Office of Research Compliance. The study itself is conducted as Not Human Research (since are de-identified) set forth by the Code of Federal Regulations (45 CFR 46) and therefore exempt from further IRB review.
RESULTS
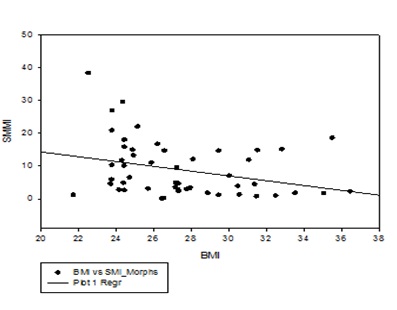
A total of 53 semen samples were assessed as described. The mean BMI was 27.5 with a low of 21.7 and a high of 36.5. The mean SM2A (calculated as motility*progression category*morphology percent) was 8.9 with a low of 0.22 (this individual had a BMI of 26.6) and a high of 38.4 (this individual had a BMI of 22.5. Regression analysis showed a significant (P<0.05) negative relationship between BMI and the SM2A (Figure 1).
DISCUSSION
The detriment of excessive body mass on male fertility has been well-studied and demonstrated. This study found that an increased body mass has a negative impact on the sperm motility-morphology algorithm. Despite numerous studies showing negative effects of obesity, comprehensive metrics have not been elucidated consistently. Obesity has been shown to have a negative impact on fertility, but inconsistent correlation to various sperm metrics have made predicting fertility difficult. However, this study contributes to the hypothesis that BMI can be used to predict the significant harmful effects of obesity on fertility. Unlike SMI data, there was both a statistically and clinically significant difference when morphology was accounted for in the algorithm. In the context of obesity, the SM2A showed to be a useful metric for demonstrating sperm health as a dependent variable. This shows promise that the SM2A algorithm may serve a purpose to generate information that will aid physicians and patients in making more informed treatment decisions regarding infertility.
The current project was limited by its small sample size. Expansion of the sample would allow for greater delineation of the correlation between BMI and SM2A and allow for the analysis of subpopulations within the study. The SM2A should be considered by other groups as a tool for future research as a concise indicator of sperm health that can be studied in the context of other variables. Continued use would develop a greater confidence in the reliability and validity for the metric across multiple variables. Perhaps most impactful would be the determination if SM2A has a correlation with male fertility and achieving successful intrauterine pregnancies thus solidifying it as a clinically significant analytical tool. Future research could then be directed to interpreting the weight of each component of the SM2A. A single quantitative metric that incorporates both motility and morphology such as the SM2A should be studied further as a guiding marker of sperm health.
REFERENCES
- Cawley J, Meyerhoefer C (2012) The medical care costs of obesity: An instrumental variables approach. J Health Econ 31: 219-230.
- Nguyen RH, Wilcox AJ, Skjaerven R, Baird DD (2007) Men’s body mass index and infertility. Hum Reprod 22: 2488-2493.
- Sallmen M, Sandler DP, Hoppin JA, Blair A, Baird DD (2006) Reduced fertility among overweight and obese men. Epidemiology 17: 520-523.
- Di Vincenzo A, Busetto L, Vettor R, Rossato M (2018) Obesity, male reproductive function and bariatric surgery. Front Endocrinol 9: 769.
- Chambers TJ, Richard RA (2015) The impact of obesity on male fertility. Hormones 14: 563-568.
- Skurla M, Rybar R (2018) Obesity and reduced fertility of men. Ceska Gynekol 83: 212-217.
- Corona G, Rastrelli G, Monami M, Saad F, Luconi M, et al. (2013) Body weight loss reverts obesity-associated hypogonadotropic hypogonadism: A systematic review and meta-analysis. Eur J Endorinol. 168: 829-843.
- Cooper TG, Noonan E, von Eckardstein S, Auger J, Gordon Baker HW, et al. (2010) World Health Organization reference values for human semen characteristics. Human Reproduction Update 16: 231-245.
- Eisenberg ML, Kim S, Chen Z, Sundaram R, Schisteman EF, et al. (2014) The relationship between male BMI and waist circumference on semen quality: Data from the LIFE study. Hum Reprod 29: 193-200.
- B MA-A, Gutschi T, Pummer K, Zigeuner R, Brookman-May S, et al. (2014) Body mass index has no impact on sperm quality but on reproductive hormone levels. Andrologia 46: 106-116.
- Alshahrani S, Ahmed AF, Gabr AH, Abalhassan M, Ahmad G (2016) The impact of body mass index on semen parameters in infertile men. Andrologia 48: 1125-1129.
- Proctor JH, Blackhurst DW, Boone WR (2004) Does seasonality alter intrauterine insemination outcomes: A 5-year study. J Assis Reprod Genet 21: 263-270.
- Allen NC, Herbert CM 3rd, Maxson WS, Rogers BJ, Diamond MP, et al. (1985) Intrauterine insemination: A critical review. Fertil Steril 44: 569-580.
- Lewis KC, Lam I, Nieb J, Lam G, Desai AS, et al. (2018) Inconsistent adoption of World Health Organization V (2010) semen analysis reference ranges in the United States eight years after publication. Urology 126: 96-101.
- Tijani H, Bhattacharya S (2010) The role of intrauterine insemination in male fertility. Hum Fertil (Camb). 13: 226-232.
- Bonds CL, Roudebush WE, Lessey BA (2017) Sperm motility index and intrauterine insemination pregnancy outcomes. GHs Proceedings 2: 125-130.
- Van Waart J, Kruger TF, Lombard, CJ, Ombelet W (2001) Predictive value of normal sperm morphology in Intrauterine Insemination (IUI): A structured literature review. Hum Reprod Update 7: 495-500.
- Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima ST, et al. (2001) Sperm morphology, motility, and concentration in fertile and infertile men. NEJM 345: 1388-1393.
- Gatimel N, Moreoua J, Parinaud J, Leandri RD (2017) Sperm morphology: Assessment, pathyophysiology, clinical relevance, and state of the art in 2017. Andrology 5: 845-862.
Citation: Smith JS, Holtel M, Wynia B, Roudebush WE (2019) Sperm Motility and Morphology is Affected by Body Mass Index. Arch Urol 3: 006
Copyright: © 2019 Shawn Smith J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.