
Spinal Osteoid Osteoma in L5 Vertebral Body-A Case Report and Literature Review
*Corresponding Author(s):
Eduardo Moreira PintoOrthopaedic And Traumatology Surgery, Spine Division, Entre Douro E Vouga Hospital Center, S.M.Feira, Portugal
Email:eduardoampinto@gmail.com
Abstract
An osteoid osteoma (OO) is a benign bone tumour with a higher predisposition to affect long bones such as the femur and tibia, presenting in the vertebral spine in approximately 10%-25% of the cases. Clinically, pain is the most frequent symptom. Radiography should be the first imaging choice. Computed tomography (CT) is the elective exam for anatomical location of the nidus and surgical excision is the treatment of choice. In this article, we will describe a rare clinical case of osteoid osteoma in the vertebral body of L5 of a 31-year-old female patient whose diagnosis was obtained from a careful physical examination, followed by radiography, CT, MRI, scintigraphy and confirmed by anatomopathological examination at the time of excision by a minimally invasive technique. The patient presented a significant clinical improvement after two years of follow up, with an Oswestry Disability Index improvement of 30%.
Keywords
Osteoid Osteoma; Osseous Tumors; Spine
Evidence Level: IV
Introduction
The osteoid osteoma (OO) is a rare tumour first described by Jaffe in 1935 [1], featuring a bone-producing tumour that can occur anywhere in the skeleton [2, 3]. However, there is a predilection for the appendicular skeleton, the long bones diaphysis being the most affected sites, especially the tibia (29%) and the femur (27%) [2, 4-6]. The tumour is seen at the vertebral spine in approximately 10%-25% of the cases [7]. The lumbar section is the most affected, with a predilection for the posterior elements of the vertebrae while the vertebral body is affected in only 10% of cases [8]. It is more common in young male patients, with about 90% of patients aged between 5 and 25 years [2].
The early diagnosis of this lesion is difficult given that the insidious symptomatology and the young age of most patients cause the complementary study to be postponed [9-11]. Clinically, pain is the most frequent symptom. Generally, patients report a violent pain located near the tumour, often being intermittent in the early stages and afterwards becoming constant and more intense. Pain worsens at night and with physical activity in 95% of patients and relieves completely with small doses of salicylates [2]. In fact, the mechanisms of pain production are not fully understood [12]. Several nerve fibers cross the OO and may explain the intense pain associated [2, 12, 13]. On the other hand, the levels of prostaglandins E2 are elevated within the nidus and are a possible cause of vasodilation within the tumour, with some authors associating it to pain and its characteristics [2, 12, 14, 15].
Schajowicz et al. [16], found painful scoliosis as the main complaint, accompanied by sciatica in 12 patients (6%) from a total of 214 studied. Saifuddin et al. [17] showed scoliosis in 8 of 10 patients (80%) and in 36 of 160 patients (23%) following meta-analysis of the literature. In the opinion of these authors, scoliosis is the result of the inflammatory process of the paravertebral musculature adjacent to the tumour, resulting in an asymmetrical muscle spasm.
Case Report
Adult patient, female, 31 years old, presented at spine department with complaints of low back pain with irradiation to the right lower limb. The symptoms began 1 year before and were progressively deteriorating, being predominantly inflammatory and nocturnal. On examination, the patient had a positive Lasegue at 45º and a slight decrease in the extension force of the right hallux, with an Oswestry Disability Index of 40%.
CT of the lumbosacral spine revealed osteolytic, radiolucent lesion and perilesional sclerosis located in the right posterior paramedian side of the L5 body (Figure 1). A later study with MR imaging showed a focal area with hyper intense signal in T2-weighted and STIR, hypo signal in T1-weighted and enhancement after contrast in the right vertebral body of L5, exhibiting a small soft tissue component that contacts the right L5 root in the medial aspect of the intervertebral foramen (Figure 2). Bone scintigraphy revealed a focus of intense osteoblastic hyperactivity in the right half of the L5 body, compatible with the diagnosis of osteoid osteoma (Figure 3). Removal of the lesion described in the images was made with a minimally invasive technique with the Quadrant system (Figure 4). The anatomopathological report confirmed the diagnosis of osteoid osteoma (Figure 5).
After two years of follow-up, the patient presented a considerable improvement, with occasional slight back pain, localized, without strength or neuro-sensory deficits. The Oswestry Disability Index showed an improvement from 40% to 10%.
 Figure 1: CT showing a radiolucent lesion located in the right posterior para median side of the L5 body. (300x300 dpi).
Figure 1: CT showing a radiolucent lesion located in the right posterior para median side of the L5 body. (300x300 dpi).
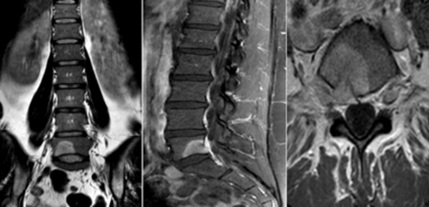 Figure 2: T2 weighted MRI revealing the presence of a focal hypersignal in the right vertebral body of L5 and a small soft tissue component that contacts the right L5 root. (300x300 dpi).
Figure 2: T2 weighted MRI revealing the presence of a focal hypersignal in the right vertebral body of L5 and a small soft tissue component that contacts the right L5 root. (300x300 dpi).
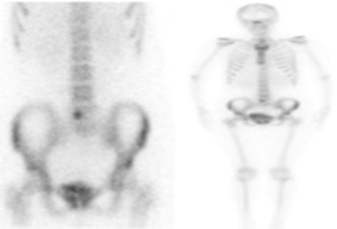 Figure 3: Bone scintigraphy revealed a focus of intense osteoblastic hyperactivity in the right half of the L5 body. (300x300 dpi).
Figure 3: Bone scintigraphy revealed a focus of intense osteoblastic hyperactivity in the right half of the L5 body. (300x300 dpi).
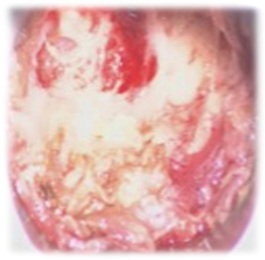 Figure 4: Removal of the lesion with a minimally invasive technique (Quadrant system). (600x600 dpi).
Figure 4: Removal of the lesion with a minimally invasive technique (Quadrant system). (600x600 dpi).
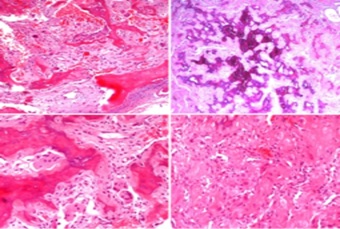 Figure 5: Microscopic examination disclosed, in a background of fibro vascular loose stroma, anastomosing irregular trabeculae of woven bone, with mineralization, rimmed by single layers of osteoblast and osteoclast typical of “nidus”. Nuclear atypia or mitotic figures were not observed. Pagetoid reversal lines or spindle cell component were absent. (600x600 dpi).
Figure 5: Microscopic examination disclosed, in a background of fibro vascular loose stroma, anastomosing irregular trabeculae of woven bone, with mineralization, rimmed by single layers of osteoblast and osteoclast typical of “nidus”. Nuclear atypia or mitotic figures were not observed. Pagetoid reversal lines or spindle cell component were absent. (600x600 dpi).
Discussion
This article is relevant as it reports a rare bone-producing tumor that only affects the vertebral spine in approximately 10 to 25% of the cases, 10% of which in the vertebral body. On the other hand, there are still many doubts in the literature regarding the best way to treat this type of tumors.
Concerning the diagnosis, radiography identifies the lesion in more than 75% of the cases and should be the first imaging choice [2]. However, the round radiolucent radiograph and surrounding sclerosis, typical of osteoid osteoma, is often not seen on plain radiographs. Computed tomography (CT) is the elective exam for anatomical location of the nidus, revealing a superior diagnostic acuity to that of magnetic resonance imaging (MRI) [12, 18-21]. MRI makes the initial diagnosis difficult because it emphasizes soft tissue alteration due to the inflammatory process adjacent to the bone lesion [11, 22-24]. Bone scintigraphy is a sensitive but not very specific examination, although the double density signal is practically diagnostic. This signal is characterized by a focus of intense fixation of the radiopharmaceutical surrounded by a less intense concentric area of hyper fixation [25, 26].
Surgical excision is the treatment of choice [17, 27, 28] but its complete resection may not be reached due to an increased risk of instability or iatrogenic neurological injury [27, 29, 30]. Careful planning through imaging examinations is therefore necessary [28, 31, 32]. The posterior approach is usually indicated since the it is the most common location for the tumour. If there is the need for articular facetectomy, arthrodesis should be performed to prevent the risk of iatrogenic instability [31]. The maintenance of pain is a frequent indication of residual disease due to incomplete resection, whereas pain recurrence is suggestive of recurrence of the tumour [16, 33]. When full tumour resection is not possible, many authors advocate selective embolization and radiofrequency ablation (RFA) as adjunctive therapy [28, 32]. Postoperative complications after tumour removal include postoperative hematoma, infections, incomplete removal and nerve iatrogenic damage [2].
Previous studies demonstrate the possibility of spontaneous resolution between 2 to 8 years after OO diagnosis. Nevertheless, is a tumour that often presents associated with significant pain complaints and risk of developing secondary scoliosis, what justifies surgical resection, generally made in blocks, removing sclerosis core and halo [31, 34-36]. The imagological changes associated with OO characterization are well described. Nevertheless, the definitive diagnosis is made after anatomopathological study [37].
Rosenthal et al. first described RFA has a minimally invasive treatment procedure with good outcomes for the treatment of osteoid osteoma [38-41]. RFA gained a vast consensus and quickly became the treatment of choice for no spinal OO [42]. Subsequently, this treatment was studied as a potential effective treatment for the treatment of OO in vertebral locations, even taking into account the increased risk of neural damage. There is growing evidence defending RFA as the gold standard procedure for spinal OO. Effectively, in case without neural elements compression, it has the potential to replace surgical and more invasive approaches [2, 43-46]. However, the lack of material for anatomopathological examination presents a disadvantage of this method for diagnostic confirmation.
Conclusion
The osteoid osteoma (OO) is a rare bone-producing tumour that can develop anywhere in the skeleton, with a predilection for the appendicular skeleton.
It is more common in young male patients, with about 90% of patients aged between 5 and 25 years.
The lumbar section is the most affected, with a predilection for the posterior elements of the vertebrae while the vertebral body is affected in only 10% of cases.
Surgical excision is the treatment of choice but its complete resection may not be reached due to an increased risk of instability or iatrogenic neurological injury.
There is increasing evidence defending RFA as the gold standard procedure for spinal OO. Effectively, in case without neural elements compression, it has the potential to replace surgical and more invasive approaches.
Conflict of interest
The authors declare that there are no conflicts of interest.
Sources of financial support that require acknowledgment
None
Approval code issued by the institutional review board (IRB)
This study is only a retrospective description of a clinical case and a narrative review; it does not present any type of change in conduct or follow-up. Therefore, approval by the IRB or ethics committee is not required.
Statement of Informed Consent
The patient was informed that data concerning the case would be submitted for publication and agreed with the creation and publication of this article.
References
- Jaffe HL (1935) Osteoid-osteoma. A benign osteoblastic tumor of osteoid and atypical bone. Arch Surg. 31: 709-28.
- Khan NA, Chandramohan M, Turnbull I, Macdonald S (2005) Osteoid Osteoma. E Medicine [serial online].
- Brook S, Piccora R (2021) Osteoid Osteoma: Diagnosis and Treatment. Available in online.
- Barbiera (2002) Osteoma osteoide intrarticolare. La Radiologia Medica, 103: 464-473.
- Kronbauer FL, Ortiz R, Kronbauer AL, Zylbersztejn S (1997) Osteoma osteóide no osso ilíaco: relato de caso. Rev Bras Ortop, 32: 12.
- Barros Filho TEP, Oliveira RP, Cristante AF, Barbarini AF (2006) Tratamento de osteoma osteóide de corpo vertebral da coluna lombar por abalação por radiofrequência. Acta Ortop Bras, 14.
- Azouz EM, Korolowski K, Marton D, Sprague P, Zerhouni A, et al. (1986) Osteoid osteoma and osteoblastoma of the spine in children: report of 22 cases with brief literature review. Pediatr Radiol. 16: 25-31.
- Lindner NJ, Ozaki T, Roedl R, Gosheger G, Winkelmann W, et al. (2001) Percutaneous radiofrequency ablation in osteoid osteoma. J Bone Joint Surg Br. 83: 391-6.
- Dezen EL, Avanzi O, Salomão JCA, Filho P, de Carvalho W (1994) Tumores benignos da coluna cervical. Rev Bras Ortop. 29: 94-8.
- Rothman RH, Simeone FA (1992) The spine. 4th ed. Philadelphia: W.B. Saunders; 2: 1171-3.
- Cecin HA (1997) Proposição de uma reserva anatomofuncional, no canal raquidiano, como fator interferente na fisiopatologia das lombalgias e lombociatalgias mecânico-degenerativas. Rev Assoc Med Bras. 43: 295-310.
- Arriaza-Loureda R, Canto-Lelián B, Sampedrocurbera C (2005) Presentación Atípica de un osteoma osteoide. Acta Ortop Gallega; 1: 24-26.
- Hasegawa T, Hirose T, Sakamoto R, Seki K, Ikata T, et al. (1993) Mechanism of pain in osteoid osteomas: an immunohistochemical study. Histopathol; 22: 487-491.
- Wold LE, Pritchard DJ, Bergert J, Wilson DM (1988) Prostaglandin synthesis by osteoid osteoma and osteoblastoma. Mod Pathol, 1: 129-131.
- Rosenthal D, Springfield DS, Gebhardt MC, Rosenberg AE, Mankin HJ, et al. (1995) Osteoid osteoma: percutaneous radiofrequency ablation. Radiology. 197: 451-4.
- Schajowicz F, Lemos C (1970) Osteoid osteoma and osteoblastoma. Closely related entities of osteoblastic derivation. Acta Orthop Scand. 41: 272-91.
- Saifuddin A, White J, Sherazi Z, Shaikh MI, Natali C, et al. (1998) Osteoid osteoma and osteoblastoma of the spine. Factors associated with the presence of scoliosis. Spine (Phila Pa 1976). 23: 47-53.
- Tekaya AB, Moalla M, Salah MB, Saidane O, Tekaya R, et al. (2021) Spinal Osteoid Osteoma Revealed by Radiculopathy: Case Report and Literature Review. Int J Spine Surg. 14: S26-S32.
- Ameri E, Nikouei F, Ghandhari H, Sabbaghan S, Givehchian B (2019) Osteoid Osteoma of Odontoid: Case Report and Literature Review. Arch Bone Jt Surg. 7: 566-570.
- Gomes SF, Alves C, Cardoso P, Ling TP (2020) A Rare Case of an Osteoid Osteoma of the Cervical Spine. Case Rep Orthop Res; 3: 79-87.
- Maalepati V, Raviraj A, Anand A (2019) Osteoid Osteoma of the Sacrum - Case Report and Review of Literature. Journal of Advances in Medicine and Medical Research, 30: 1-6.
- Ozaki T, Liljenqvist U, Hillmann A, Halm H, Linder N, et al. (2002) Osteoid osteoma and osteoblastoma of the spine: experiences with 22 patients. Clin Orthop Relat Res. (397): 394-402.
- Keim HA, Reina EG (1975) Osteoid-osteoma as a cause of scoliosis. J Bone Joint Surg Am. 57: 159-63.
- Weinstein JN, McLain RF (1987) Primary tumors of the spine. Spine (Phila Pa 1976). 12: 843-51.
- Etchbehere M (1967) Localização Intra-operatória do osteoma osteóide com auxílio de uma sonda de raios gama. Tese de doutoramento. Available in online.
- WU GM (1994) Osteoid Osteoma. Department of Radiology at Brigham and Women’s Hospital. Available in online.
- Jaffe HL, Mayer L (1932) An osteoblastic osteoid tissue-forming tumor of a metacarpal bone. Arch Surg. 24: 550-64.
- Chew FS, Pena CS, Keel SB (1998) Cervical spine osteoblastoma. AJR Am J Roentgenol. 171:
- McLeod RA, Dahlin DC, Beabout JW (1976) The spectrum of osteoblastoma. AJR Am J Roentgenol; 126: 321-5.
- De Souza DL, Frost HM (1973) Osteoblastoma of the spine. A review and report of eight new cases. Clin Orthop Relat Res. (91): 141-51.
- Ozaki T, Liljenqvist U, Hillmann A, Halm H, Linder N, et al. (2002) Osteoid osteoma and osteoblastoma of the spine: experiences with 22 patients. Clin Orthop Relat Res. (397): 394-402.
- Avanzi O, Joilda FG, Donato JP, Dezen EL, Carvalho PW (1996) Tumores benignos e lesões pseudotumorais da coluna vertebral. Análise de 60 pacientes. Rev Bras Ortop. 31: 131-42.
- Schajowicz F (1982) Tumores y lesiones seudotumolares de huesos y articulaciones. Buenos Aires: Editorial Medica Panamericana. ISBN: 9500619520.
- MacLellan DI, Wilson FC (1967) Osteoid osteoma of the spine. A review of the literature and report of six new cases. J Bone Joint Surg Am. 49: 111-21.
- Marcove R, Heelan R, Huvos A, Healey J, Lindeque BG (1991) Osteoid osteoma: diagnosis, localization and treatment. Clin Orthop. 267: 197-201.
- Lee D, Malawer MM (1992) Staging and treatment of primary and persistent (recurrent) osteoid osteoma: evaluation of intraoperative nuclear scanning, tetracycline fluorescence and tomography. Clin Orthop. 281: 229-38.
- Kchouk M, Mrabet A, Touibi S, Douik M, Siala M, et al. (1993) Osteoid osteoma of the spine. Radiological study of 21 cases. J Radiol. 74: 135-42.
- Rosenthal DI, Hornicek FJ, Wolfe MW, Jennings LC, Gebhardt MC, et al. (1998) Percutaneous radiofrequency coagulation of osteoid osteoma compared with operative treatment. J Bone Joint Surg Am. 80: 815-21.
- Rosenthal DI, Alexander R, Rosenberg AE, Springfield D (1992) Ablation of osteoid osteomas with a percutaneously placed electrode: a new procedure. Radiology. 183: 29-33.
- De Berg JC, Pattynama PM, Obermann WR, Bode PJ, Vielvoye GJ, et al. (1995) Percutaneous computed-tomography guided thermocoagulation for osteoid osteomas. Lancet. 346: 350-1.
- Barbiera M (2002) Osteoma osteoide intrarticolare. La Radiologia Medica, 103: 464-473.
- Azouz EM, Korolowski K, Marton D, Sprague P, A Zerhouni A, et al. (1986) Osteoid osteoma and osteoblastoma of the spine in children: report of 22 cases with brief literature review. Pediatr Radiol. 16: 25-31.
- Barei DP, Moreau G, Scarborough MT, Neel MD (2000) Percutaneous radiofrequency ablation of osteoid osteoma. Clin Orthop. 373: 115-24.
- Boriani S, Weinstein JN (1997) Differential diagnosis and surgical treatment of primary benign and malignant neoplasms. The Adult Spine, 22: 950-87.
- Jackson RP, Reckling PW, Mants FA (1977) Osteoid Osteoma and osteoblastoma: similar histology lesions with different natural histories. Clin Orthop. 128: 303-13.
- Lindner NJ, Ozaki T, Roedl R, Gosheger G, Winkelmann W, et al. (2001) Percutaneous radiofrequency ablation in osteoid osteoma. J Bone Joint Surg Br. 83: 391-6.
Citation: Pinto EM, Teixeira A, Frada R, Silva H, Veigas T, et al. (2023) Spinal Osteoid Osteoma in L5 Vertebral Body-A Case Report and Literature Review. J Clin Stud Med Case Rep 10: 0153.
Copyright: © 2023 Eduardo Moreira Pinto, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

