
Statewide Prevalence of Stepping on, Tai Chi, and a Matter of Balance Community Fall Prevention Programs at Maryland Senior Centers in 2017 and 2020
*Corresponding Author(s):
Levan AtanelovSteady Strides: Fall Prevention And Stroke Rehabilitation Medical Institute; Johns Hopkins Physical Medicine And Rehabilitation, 9199 Reisterstown Rd Suit 101B, Owings Mills, MD 21117, Baltimore, Maryland, United States
Tel:+1 4438988160,
Email:latanelov@steadystridesmd.com
Abstract
Study background: Older adults suffer from fall-related injuries and deaths at disproportionate rates. One recommendation by the Center for Disease Control and Prevention to help prevent falls is that patients utilize Community Fall Prevention Programs (CFPPs). Little is known about the offering of these programs at Senior Centers (SCs).
Methods: We conducted a telephone-based survey to assess the statewide prevalence and underreporting in Maryland SCs of Stepping On (SO), Tai Chi (TC) and a Matter of Balance (MOB).
Results: 107 SCs were contacted in December 2017, and 111 in January 2020. 76.6% of SCs offered at least one of these three programs in 2017 but only 56.8% in 2020 (95% CI 6.7% to 33.0%; P=.003). SO was offered in 27 SCs (25.2%) in 2017 and 7 (6.3%) in 2020 (95% CI 8.6% to 29.2%; P<.001). TC was offered in 70 SCs (65.4%) in 2017 and 61 (55.0%) in 2020. MOB was offered in 12 SCs (11.2%) in 2017 and 2 (1.8%) in 2020 (95% CI 2.0 to 16.8%; P=.01). Furthermore, telephone operators did not volunteer availability of these programs 72.5% in 2017 and 95.7% in 2020 (95% CI 12.4% to 33.0%; P<.001). SO was underreported by 66.7% of SCs in 2017 and 100% in 2020. TC was underreported by 71.4% of SCs in 2017 and 95.1% in 2020 (95% CI 10.2 to 37.1, P<.001). MOB was underreported by 91.7% of SCs in 2017 and 100% in 2020.
Conclusion: There are geographical and temporal variations in these three CFPP offerings, with a downward trend in Maryland. Over the span of our study, the prevalence of these three programs has significantly decreased, while underreporting has significantly increased. Evidently, seniors may have difficulty finding CFPPs or receiving correct information about them from local SCs.
Keywords
Falls; Fall prevention; Geriatrics; Older adults; Senior center
Introduction
The Centers for Disease Control and Prevention (CDC) recommends evidence-based Community Fall Prevention Programs (CFPPs) to prevent fall-related injury in older adults [1]. Though access to healthcare is one of the five key areas of social determinants of health, little is known about the offering of CFPPs at Senior Centers (SCs). Prior studies indicate that Stepping On (SO), Tai Chi (TC), and A Matter of Balance (MOB) may be the most common CFPPs at SCs in the US. Prior prevalence literature only examined rural areas [2], or medical center vicinity [3], and did not assess trends over time. The current study assesses statewide availability of SO, TC and MOB in 2017 and 2020 (prior to the COVID19 pandemic) to help better understand access to CFPPs in Maryland.
Materials and Methods
Participants
111 SCs across the 24 counties listed in Maryland Department of Aging’s 2015 Database [4] were studied. Nursing homes, assisted living facilities, adult day care centers and community wellness programs were excluded.
Study design and survey method
We conducted telephone-based surveys in December 2017 and January 2020 to gather the data. SC telephone numbers were obtained from the 2015 Database [4] and were contacted on weekdays during normal business hours. SCs were excluded if no point of contact was established after three attempts on separate days. We did not differentiate between different types of TC interventions e.g., Tai Chi for Arthritis (TCA) or Tai Ji Quan: Moving for Better Balance (TJQ), since telephone operators only referred to any of these programs as TC. After reaching a SC, the telephone operator was asked two questions: 1) “For geriatrics, what fall prevention programs do you offer?;” and 2) “Does your senior center offer SO?, TC?, or MOB?” If the SC representative requested clarification, we detailed the nature of these programs.
Data measurement
For each question, presence or absence of the three CFPPs queried was noted for each SC in 2017 and 2020.
Additional measures
Median county income (in dollars), county population, and proportion of seniors (>65 years old) for each of the 24 counties were obtained from the 2016 and 2018 US Census Bureau Quick Facts [5]. We hypothesized that these variables may play a role in the prevalence and underreporting of SO, TC and MOB.
Statistical analysis
Descriptive statistics were used to analyze the survey results, and univariate and multivariate logistic models were used to analyze our additional measures. Statistical analysis was performed using R: A Language and Environment for Statistical Computing, version 3.6.3, available at http://www.R-project.org (The R Foundation for Statistical Computing). P values were 2-sided at .05 significance.
Results
Across the 24 counties in Maryland, 107 SCs were contacted in December 2017 and 111 in January 2020. 76.6% of SCs offered at least one of these three CFPPs in 2017 but only 56.8% in 2020, a statistically significant decrease of 19.9% (95% CI 6.7% to 33.0%; P=.003). TC was offered in 70 SCs (65.4%) in 2017 and 61 (55.0%) in 2020 (95% CI 3.4% to 24.3%; P=.15). SO offering significantly decreased by 18.9% (95% CI 8.6% to 29.2%; P <.001) from 27 SCs (25.2%) in 2017 to 7 (6.3%) in 2020, whereas MOB by 9.4% (95% CI 2.0 to 16.8%; P=.01) from 12 SCs (11.2%) in 2017 to 2 (1.8%) in 2020 (Figure 1). Table 1 demonstrates that there is both regional and temporal variation in offering these CFPPs. Univariate analysis yielded association between SO prevalence and median county income (P=.05); TC prevalence and median county income and county population (P <.001 and P=.004). Multivariate analysis showed that TC prevalence maintained its association with median county income and county population (P <.001 and P=.001). In both analyses, MOB prevalence was associated with county population (P=.05 and P=.04).
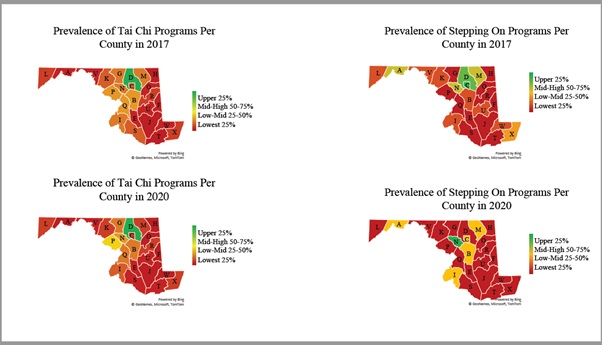 Figure 1: Prevalence of Tai Chi and stepping on programs per Baltimore County in 2017 and 2020.
Figure 1: Prevalence of Tai Chi and stepping on programs per Baltimore County in 2017 and 2020.
County abbreviations: A: Allegany, B: Anne Arundel, C: Baltimore City, D: Baltimore County, E: Calvert, F: Caroline, G: Carroll, H: Cecil, I: Charles, J: Dorchester, K: Frederick, L: Garrett, M: Harford, N: Howard, O: Kent, P: Montgomery, Q: Prince George's, R: Queen Anne's, S: St. Mary's, T: Somerset, U: Talbot, V: Washington, W: Wicomico, X: Worcester
|
|
Prevalence Number/Total Number of SC (%) |
Underreporting Number/Total Number of SC* (%) |
||||||||||
|
|
SO |
TC |
MOB |
SO |
TC |
MOB |
||||||
|
|
2017 |
2020 |
2017 |
2020 |
2017 |
2020 |
2017 |
2020 |
2017 |
2020 |
2017 |
2020 |
|
Allegany (n=4) |
3/4 (75) |
1/4 (25) |
1/4 (25) |
0/4 (0) |
0/4 (0) |
0/4 (0) |
0/3 (0) |
1/1 (100) |
0/1 (0) |
N/A |
N/A |
N/A |
|
Anne Arundel (n=8) |
1/8 (13) |
1/8 (13) |
5/8 (63) |
4/8 (50) |
1/8 (13) |
1/8 (13) |
1/1 (100) |
1/1 (100) |
4/5 (80) |
4/4 (100) |
1/1 (100) |
1/1 (100) |
|
Baltimore City (n=13) |
5/13 (38) |
1/13 (8) |
3/13 (23) |
2/13 (15) |
0/13 (0) |
1/13 (8) |
5/5 (100) |
1/1 (100) |
1/3 (33) |
2/2 (100) |
N/A |
1/1 (100) |
|
Baltimore County (n=19) |
4/19 (21) |
0/19 (0) |
17/19 (89) |
17/19 (89) |
0/19 (0) |
0/19 (0) |
3/4 (75) |
N/A |
13/17 (76) |
15/17 (88) |
N/A |
N/A |
|
Calvert (n=3) |
0/3 (0) |
0/3 (0) |
1/3 (33) |
1/3 (33) |
0/3 (0) |
0/3 (0) |
N/A |
N/A |
1/1 (100) |
1/1 (100) |
N/A |
N/A |
|
Caroline (n=2) |
0/2 (0) |
0/2 (0) |
1/2 (50) |
0/2 (0) |
0/2 (0) |
0/2 (0) |
N/A |
N/A |
0/1 (0) |
N/A |
N/A |
N/A |
|
Carroll (n=5) |
0/5 (0) |
0/5 (0) |
4/5 (80) |
4/5 (80) |
1/5 (20) |
0/5 (0) |
N/A |
N/A |
4/4 (100) |
4/4 (100) |
1/1 (100) |
N/A |
|
Cecil (n=1) |
0/1 (0) |
0/1 (0) |
0/1 (0) |
0/1 (0) |
0/1 (0) |
0/1 (0) |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
|
Charles (n=4) |
1/4 (25) |
1/4 (25) |
4/4 (100) |
3/4 (75) |
1/4 (25) |
0/4 (0) |
1/1 (100) |
1/1 (100) |
3/4 (75) |
3/3 (100) |
1/1 (100) |
N/A |
|
Dorchester (n=2) |
0/2 (0) |
0/2 (0) |
0/2 (0) |
0/2 (0) |
0/2 (0) |
0/2 (0) |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
|
Frederick (n=4) |
1/4 (25) |
0/4 (0) |
3/4 (75) |
2/4 (50) |
1/4 (25) |
0/4 (0) |
0/1 (0) |
N/A |
3/3 (100) |
2/2 (100) |
1/1 (100) |
N/A |
|
Garrett (n=3) |
1/3 (33) |
0/3 (0) |
2/3 (67) |
2/3 (67) |
0/3 (0) |
0/3 (0) |
1/1 (100) |
N/A |
1/2 (50) |
2/2 (100) |
N/A |
N/A |
|
Harford (n=6) |
3/6 (50) |
1/6 (17) |
4/6 (67) |
2/6 (33) |
0/6 (0) |
0/6 (0) |
1/3 (33) |
1/1 (100) |
3/4 (75) |
2/2 (100) |
N/A |
N/A |
|
Howard (n=7) |
3/7 (43) |
2/7 (29) |
4/7 (57) |
5/7 (71) |
0/7 (0) |
0/7 (0) |
3/3 (100) |
2/2 (100) |
4/4 (100) |
5/5 (100) |
N/A |
N/A |
|
Kent (n=1) |
0/1 (0) |
0/1 (0) |
1/1 (100) |
0/1 (0) |
1/1 (100) |
0/1 (0) |
N/A |
N/A |
1/1 (100) |
N/A |
1/1 (100) |
N/A |
|
Montgomery (n=7) |
0/7 (0) |
0/7 (0) |
5/7 (71) |
7/7 (100) |
1/7 (14) |
0/7 (0) |
N/A |
N/A |
2/5 (40) |
7/7 (100) |
1/1 (100) |
N/A |
|
Prince George's (n=8) |
0/8 (0) |
0/8 (0) |
5/8 (63) |
4/8 (50) |
0/8 (0) |
0/8 (0) |
N/A |
N/A |
5/5 (100) |
3/4 (100) |
N/A |
N/A |
|
Queen Anne's (n=3) |
0/3 (0) |
0/3 (0) |
2/3 (67) |
2/3 (67) |
1/3 (33) |
0/3 (0) |
N/A |
N/A |
1/2 (50) |
2/2 (100) |
1/1 (100) |
N/A |
|
St. Mary's (n=1) |
1/1 (100) |
0/1 (0) |
1/1 (100) |
1/1 (100) |
1/1 (100) |
0/1 (0) |
1/1 (100) |
N/A |
1/1 (100) |
1/1 (100) |
1/1 (100) |
N/A |
|
Somerset (n=3) |
0/3 (0) |
0/3 (0) |
3/3 (100) |
1/3 (33) |
2/3 (67) |
0/3 (0) |
N/A |
N/A |
1/3 (33) |
1/1 (100) |
1/2 (50) |
N/A |
|
Talbot (n=1) |
0/1 (0) |
0/1 (0) |
0/1 (0) |
1/1 (0) |
0/1 (0) |
0/1 (0) |
N/A |
N/A |
N/A |
1/1 (100) |
N/A |
N/A |
|
Washington (n=1) |
1/1 (100) |
0/1 (0) |
1/1 (100) |
1/1 (100) |
0/1 (0) |
0/1 (0) |
0/1 (0) |
N/A |
0/1 (0) |
1/1 (100) |
N/A |
N/A |
|
Wicomico (n=1) |
1/1 (100) |
0/1 (0) |
1/1 (100) |
0/1 (0) |
1/1 (100) |
0/1 (0) |
0/1 (0) |
N/A |
1/1 (100) |
N/A |
1/1 (100) |
N/A |
|
Worcester (n=4) |
2/4 (50) |
0/4 (0) |
2/4 (50) |
2/4 (50) |
1/4 (25) |
0/4 (0) |
2/2 (100) |
N/A |
1/2 (50) |
2/2 (100) |
1/1 (100) |
N/A |
Table 1: Telephone survey results collected in 2017 and 2020 by Maryland County.
*Total number of senior centers which offer the program.
N/A values are indicated for counties where the specific fall prevention program was not offered that year
Abbreviations: SC: Senior Center; SO: Stepping On, TC: Tai Chi, MOB: A Matter of Balance
Overall, telephone operators did not volunteer availability of CFPPs 72.5% in 2017 and 95.7% in 2020, a statistically significant increase of 23.2% (95% CI 12.4% to 33.0%; P<.001) (Figure 2). SO was underreported by 66.7% of SCs in 2017 and 100% in 2020 (95% CI6.6 to 60.1; P=.19). TC was underreported by 71.4% of SCs in 2017 and 95.1% in 2020, a statistically significant increase of 23.7% (95% CI 10.2 to 37.1; P<.001). MOB was underreported by 91.7% of SCs in 2017 and 100% in 2020 (95% CI -15.6 to 32.3; P>.99). In both univariate and multivariate analyses, TC underreporting was associated with median county income (P <.00 and P <.001) and county population (P=.02 and P=.01).
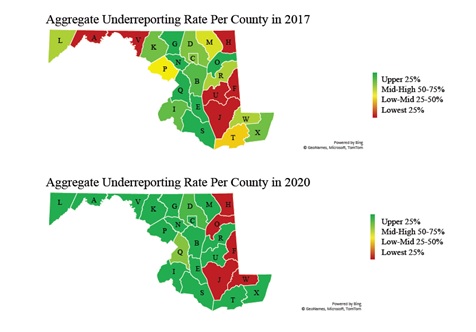 Figure 2: Aggregate underreporting rates of Tai Chi, stepping on, and a matter of balance programs per Baltimore County in 2017 and 2020.
Figure 2: Aggregate underreporting rates of Tai Chi, stepping on, and a matter of balance programs per Baltimore County in 2017 and 2020.
County abbreviations: A: Allegany, B: Anne Arundel, C: Baltimore City, D: Baltimore County, E: Calvert, F: Caroline, G: Carroll, H: Cecil, I: Charles, J: Dorchester, K: Frederick, L: Garrett, M: Harford, N: Howard, O: Kent, P: Montgomery, Q: Prince George's, R: Queen Anne's, S: St. Mary's, T: Somerset, U: Talbot, V: Washington, W: Wicomico, X: Worcester
Discussion
Though CFPPs are part of the CDC’s fall prevention algorithm [1], this is the first study to 1) provide a statewide survey of CFPPs at SCs; 2) assess for change in prevalence over time; and 3) document that telephone operators underreport CFPPs which they know to be offered. The current study examined the three nationally most common CFPPs [2,3] and found that at least half of the SCs offered at least one of them in 2017 and in 2020. That said, the prevalence of these programs decreased by 20% by 2020, even before the onset of the COVID19 pandemic, which caused closures of SCs nationally.
Our results indicate that there are regional and temporal variations. An older adult in Maryland who inquires about such programs at two senior centers is likely to find at least one of the three CFPPs. CFPP statewide prevalence data, combined with a clinical referral algorithm (e.g., Hamel et al., [6]), can help physicians more efficiently guide older adults to the local SC offering the appropriate CFPP. If our findings-which show significant temporal and geographical variation in the offering of CFPP-are nationally representative, then real-time online platforms should be developed to help clinicians direct patients to the SC offering the CFPP best suited to their needs.
Unfortunately, we found that making a phone call to inquire about these programs oftentimes results in receiving misleading information. In over 70% of cases, telephone operators at SCs who knew that a particular CFPP was offered failed to volunteer this information when asked about fall prevention programs at their facility. Now, amid further dissemination of the COVID19 vaccine and the positive prospects of opening SCs soon, a public health initiative may be undertaken to ensure that SC phone operators properly inform customers about the availability of their CFPPs. A national study on CFPP prevalence in SCs across the US near medical centers found that the most common CFPPs are (1) TC, (2) MOB and (3) SO [3]. A national rural-based study found that the most common CFPPs are (1) MOB, (2) SO and (3) TJQ (a type of TC) [2]. Our results indicate that the TC prevalence in Maryland is consistent with trends near medical centers and surpasses rural trends, and that MOB was not well represented in Maryland.
Limitations include only examining 3 CFPPs at SC in only one state and not differentiating between different types of TC. Although SCs are the most common places where CFPPs are delivered [7], our study did not evaluate other venues that may offer these programs. Additionally, this study only evaluated inquiries over the phone, whereas SCs may also communicate their programs in other ways, e.g., email. CFPP availability landscape may change in the post-COVID19 era. In summary, at least 50% of SCs offer CFPPs. There are geographical and temporal variations in CFPP offering, with a downward trend in Maryland. Telephone operators at SCs in Maryland do not commonly volunteer information about CFPP availability.
Statements
Acknowledgment
Ilan Lavian, New York University School of Law, provided comments and edits on the manuscript; Chaniesa Burnett, Steady Strides: Fall Prevention and Stroke Rehabilitation Medical Institute, assisted with data collection.
Conflicts of Interest
The authors have no conflicts of interests to declare.
Funding sources
The authors have no funding sources to declare.
Author contributions/commitments
LA: Study concept and design
NH, CH, DNY, MZ, BS, ME, LK, MN, MT, and LA: Acquisition of data, analysis and interpretation of data
MT: Statistical analysis
NH and CH: Preparation of manuscript
NH, CH, DNY, MZ, BS, ME, LK, MN, MT, and LA: Read and approved the final manuscript
Data Deposition: Not needed, Table 1 included
References
- Centers for Disease Control and Prevention (2020) Algorithm for Fall Risk Screening, Assessment, and Intervention. CDC, Atlanta, Georgia, USA.
- Smith ML, Towne SD, Herrera-Venson A, Cameron K, Horel SA, et al. (2018) Delivery of fall prevention interventions for at-risk older adults in rural areas: Findings from a national dissemination. Int J Environ Res Public Health 15: 2798.
- Hamel C, Hekmatjah N, Hakakian B, Banooni M, Lalezari J, et al. (2019) Evidence-Based Community Fall Prevention Programs at Senior Centers Near 10 US Academic Centers. J Am Geriatr Soc 67: 1484-1488.
- Maryland Department of Aging (2015) Maryland Senior Centers. Maryland Department of Aging, Baltimore, USA.
- US Census Bureau (2019) US Census Bureau Quick Facts. US Census Bureau Maryland, USA.
- Hamel C, Atanelov L (2020) Community-based programs to prevent the risk of elderly falls: mini review. J Card Pulm Rehabil 4: 129.
- National Council on Aging (2015) Get the Facts on Senior Centers. National Council on Aging, Virginia, USA.
Citation: Hekmatjah N, Hamel C, Younessi DN, Zargari M, Sedaghat B, et al. (2021) Statewide Prevalence of Stepping on, Tai Chi, and a Matter of Balance Community Fall Prevention Programs at Maryland Senior Centers in 2017 and 2020. J Gerontol Geriatr Med 7: 097.
Copyright: © 2021 Natan Hekmatjah, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

