
Stratifying Risk for Post-Operative Hormone Replacement Therapy (HRT): Pre-Operative Factors Predicting Hypothyroidism after Hemithyroidectomy
*Corresponding Author(s):
Justin GauthierDepartment Of Surgery, Mount Sinai - South Nassau, One Healthy Way, Oceanside, Long Island, New York, United States
Tel:860-912-3454,
Email:Justin.Gauthier@snch.org
Abstract
Background: Patients undergoing thyroid lobectomy require preoperative counseling on the potential development of postoperative hypothyroidism and therefore the need for subsequent thyroxine Hormone Replacement Therapy (HRT), potentially lifelong. Currently, preoperative TSH measurements are the standard of care for assessing the risk for postoperative hypothyroidism; however there are no quantified guidelines for pre-operatively counseling patients about this risk.
Objectives: The goal of this study is to evaluate what factors can be utilized preoperatively in order to accurately predict the need for HRT postoperatively. By correlating these factors, we hope to assist the surgeon in preoperative counseling of patients undergoing partial thyroidectomy or unilateral lobectomy.
Methods: Data from one hundred (100) thyroid specimens, between January 2011 and September 2016, were obtained from the Pathology department. Pre-operative TSH levels, thyroglobulin levels, presence of thyroiditis and microsomal antibodies were compared against post-operative TSH level, HRT requirement (and levothyroxine dosing if applicable), resected thyroid volume and specimen pathology.
Results: Of the patients with pre-operative TSH levels <2.0mIU/L, 96.2% (51/53) patients did not require post-operative HRT. While in the group with pre-operative TSH of >2.5, every patient required lifetime HRT. Results varied in patients with pre-operative TSH levels between 2.0-2.5, though the majority (63%, 5/8) did not require HRT. When further stratified into three groups, based on preoperative TSH measurements (<2.0, 2.0-2.5, >2.5), the rate of postoperative hypothyroidism significantly increased at each level.
Conclusion: Prior to thyroid lobectomy, preoperative TSH levels of >2.5 and presence of thyroiditis directly correlate to a significantly increased risk for HRT postoperatively. Conversely, TSH levels <2.0 predicts that it very unlikely that patient will require post-operative HRT. Therefore, in pre-operative counseling, surgeons can stratify the risk for post-operative HRT and thus more accurately inform their patients based on these high, moderate, and low risk categories.
BACKGROUND
Patients undergoing thyroid lobectomy require preoperative counseling on the potential development of postoperative hypothyroidism and therefore the need for subsequent thyroxine Hormone Replacement Therapy (HRT), potentially lifelong [1-3]. Multiple pre-operative factors have been postulated to influence postoperative thyroid function including, but not limited to, Thyroid Stimulating Hormone (TSH), thyroglobulin and microsomal antibodies [3-6]. Studies have also shown that individuals with lymphocytic infiltration preoperatively may be at increased risk for post-thyroid lobectomy hypothyroidism [5]. Furthermore, thyroiditis on preoperative ultrasound has been shown to aid in the prediction of HRT status post lobectomy [7]. Overall though, thyroid function can most accurately be accessed through TSH levels [1,4]. Currently, preoperative TSH measurements are the standard of care for assessing the risk for postoperative hypothyroidism [3]. However there are no quantified guidelines for counseling patients about their levothyroxine need based on TSH levels or other high risk characteristics. In summary, we identified a strong correlation with stratified preoperative TSH levels and development of postoperative levothyroxine need. This finding will allow surgeons to counsel patients more effectively about this potential postop complication.
OBJECTIVES
The goal of this study is to evaluate what factors can be utilized preoperatively in order to accurately predict the need for HRT postoperatively. By correlating these factors, we hope to assist the surgeon in preoperative counseling of patients undergoing partial thyroidectomy or unilateral lobectomy. If the patient is found to be high risk for HRT during pre-lobectomy testing, the surgeon may be able to more accurately predict the patient’s risk for hypothyroidism. Conversely, if the patient is deemed low risk, they can be reliably reassured of their minimal lifetime risk. By accurately predicting the potential need for postoperative HRT, surgeons can perform a more informed consent while concomitantly satisfying a patient's anxiety about their previously unknown risk.
DESIGN
This is a retrospective comparison of prospectively collected data. Hormone Replacement Therapy (HRT) was defined by administration of Levothyroxine, Synthroid®, prescribed by the Endocrinologists, based on TSH levels >4.5mIU/L at 6 weeks post-operatively.
Settings
The study was conducted at a 455-bed community hospital with a surgical training program in a suburban community. Patients were derived from the cases of one surgical oncology group, specializing in head and neck, performing thyroid resection weekly on average, over studied period.
Participants
Data from one hundred (100) thyroid specimens, between January 2011 and September 2016, were obtained from the Pathology department. Thirty-three (33) were excluded from study due to eventual completion thyroidectomy (20), pre-operative thyroid hormone therapy (5) and inadequate serological data (8 patients namely without pre-operative TSH levels), leaving a cohort of 67 patients for analysis (Figure 1).
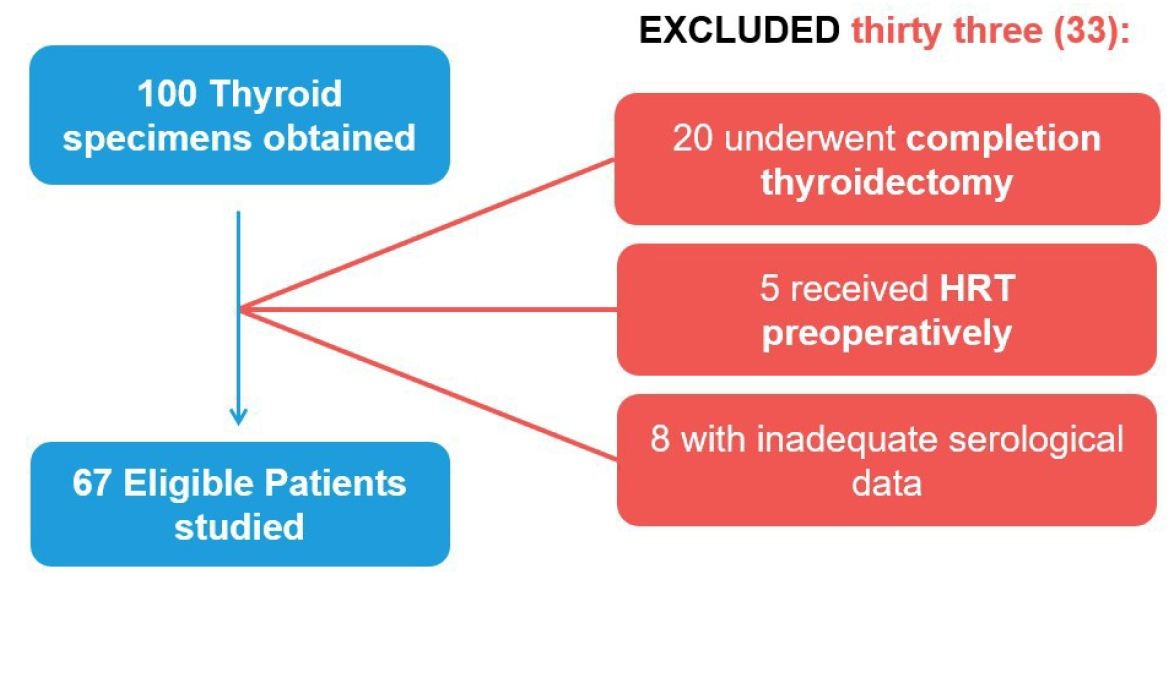 Figure 1: Flow Diagram showing exclusion criteria and resultant participants included.
Figure 1: Flow Diagram showing exclusion criteria and resultant participants included.
Patient and Public involvement
Patients were not involved in our study.
Primary and Secondary Outcome Measures
Primary outcome measure was post-operative TSH levels. Pre-operative factors assessed were TSH levels, thyroglobulin levels, and the presence of thyroiditis, microsomal antibodies, age, gender, ultrasound findings, and FNA biopsy results. The secondary outcome measures were HRT requirement (and levothyroxine dosing if applicable), resected thyroid volume and specimen pathology (Figure 2).
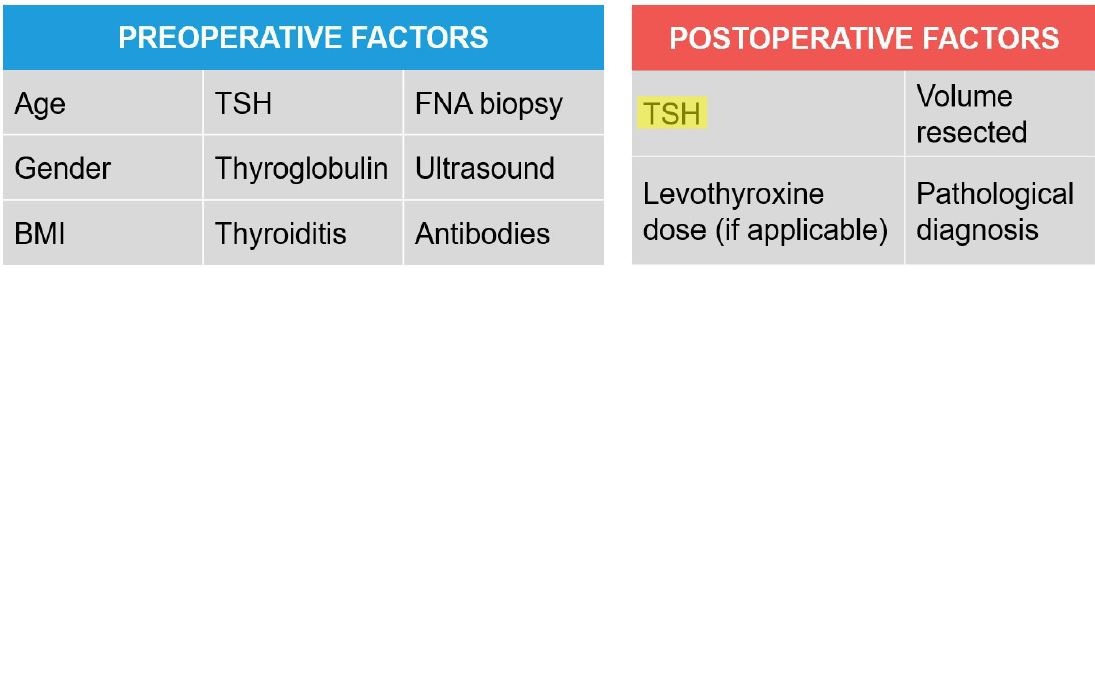 Figure 2: Primary and secondary outcome measures analyzed (primary highlighted).
Figure 2: Primary and secondary outcome measures analyzed (primary highlighted).
RESULTS
Hypothyroidism was diagnosed in 20.9% (14/67) patients post-operatively. Of the patients with pre-operative TSH levels <2.0mIU/L, 96.2% (51/53) patients did not require post-operative HRT. While in the group with pre-operative TSH of >2.5, every patient required lifetime HRT, at an average Synthroid® dose of 70mcg. Results varied in patients with pre-operative TSH levels between 2.0-2.5, though the majority (63%, 5/8) did not require HRT (Figure 3).
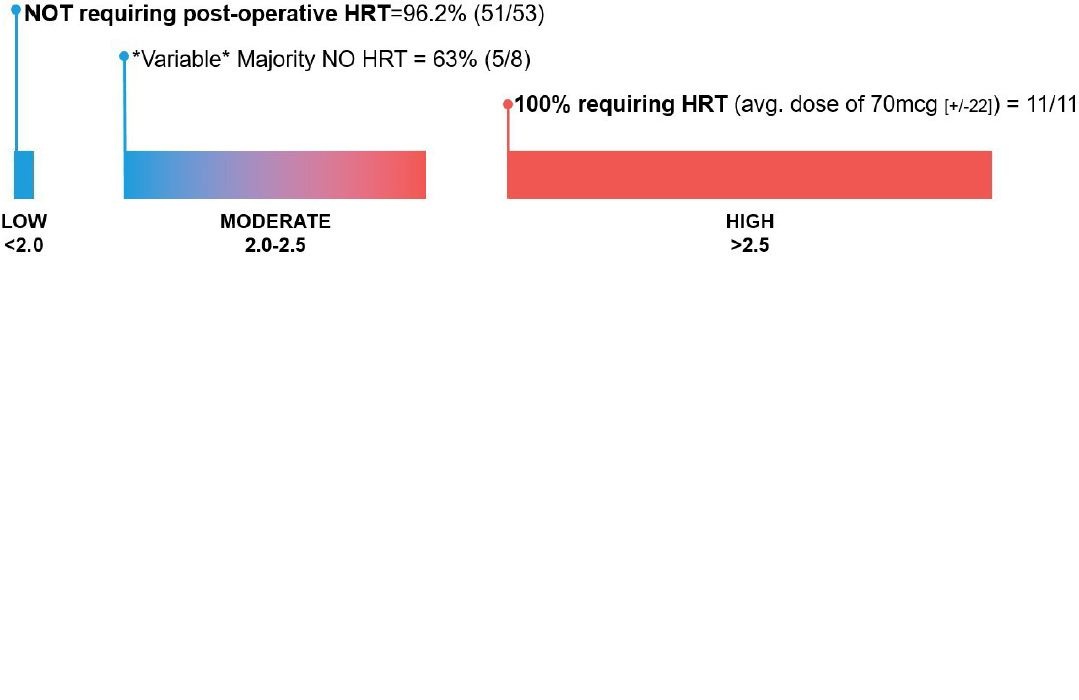 Figure 3: Flow Diagram identifying risk of Hormone Replacement Therapy (HRT) based on pre-operative TSH.
Figure 3: Flow Diagram identifying risk of Hormone Replacement Therapy (HRT) based on pre-operative TSH.
When further stratified into three groups, based on preoperative TSH measurements (<2.0, 2.0-2.5, >2.5), the rate of postoperative hypothyroidism significantly increased at each level (Figure 4).
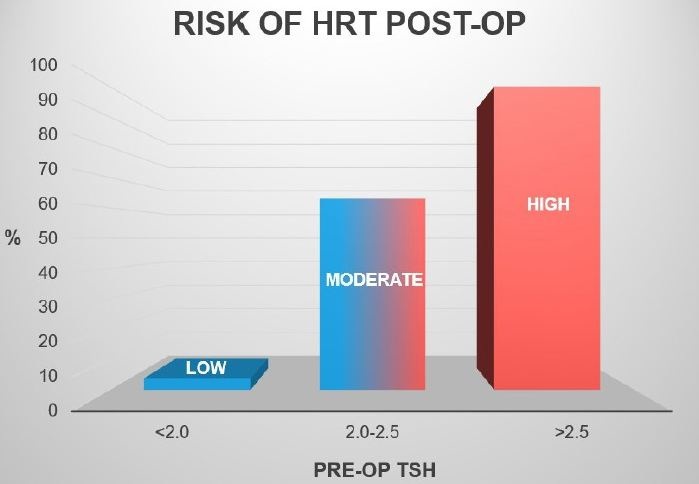 Figure 4: Bar Graph categorizing three groups of pre-operative TSH levels and subsequent post-operative HRT risk.
Figure 4: Bar Graph categorizing three groups of pre-operative TSH levels and subsequent post-operative HRT risk.
One patient in the HRT-requiring group was positive for anti-thyroglobulin antibodies and was diagnosed on pathology with Hashimoto’s disease. With data showing that most common pathology resulting as follicular multinodular goiter and only four cases of micropapillary carcinoma, to date of this publishing, no patient has required subsequent completion thyroidectomy. In the HRT-requiring patient population, thyroiditis was more prevalent compared to the group not receiving HRT post-op (67% to 22%). Average age was 55 years old with a roughly 4:1 female prevalence (76%). Age, gender, family history of thyroid disease, thyroid pathology, and weight of resected tissue were proven not clinically significant risk factors for hypothyroidism.
DISCUSSION
When patients present pre-operatively, prior to thyroid lobectomy, surgeons are obligated to discuss the potential post-operative complications, most relevantly hypothyroidism. In obtaining informed consent, this risk of lifelong HRT commonly yields the inquiry about what their individual chances of developing this life altering complication are. Currently, when presented with this inquiry, surgeons have no standardized guidelines or literature reference available to them to accurately answer this pertinent question. With our results, and our stratified risk categories, surgeons can more accurately explain to their patients, in the pre-operative period, about their potential risk for hypothyroidism, now with supported evidence.
Categorizing patients into three categories based solely on TSH levels, systematically predicts each individual’s probability of requiring HRT (Figure 5). Pre-operative TSH levels >2.5 were shown to be directly linked to a patient’s hypothyroidism risk, nearly 100% in our small sample size study. Thus these patients should be fully informed of their high risk status, emphasizing that lifelong HRT is very likely. Conversely, TSH levels <2.0 predicts it very unlikely that the patient will require HRT post-operatively and thus reassurance of their low risk status should be expressed. Though the potential is still present, patient anxiety can be better alleviated by detailing their low risk category. For those falling in the intermediate category (TSH levels 2.0-2.5), other factors (including but not limited to presence of thyroiditis, thyroglobulin, microsomal antibodies, etc), should be implored in order to better articulate their patient’s risk stratification.
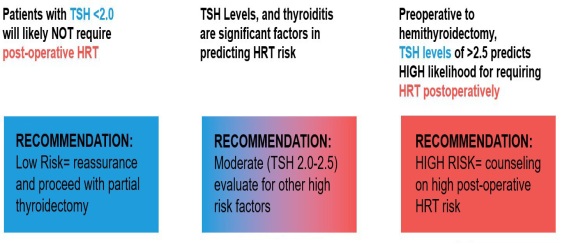 Figure 5: Figure correlating study conclusions with pre-operative counseling recommendations.
Figure 5: Figure correlating study conclusions with pre-operative counseling recommendations.
Our study was based on only 100 retrospective thyroid surgeries performed in a single academic medical center and might not be generalized beyond similar patients. We did not evaluate the predictive value of preoperative TSH level in regards to patient’s complications. Further studies including larger sample cohorts are essential to define the statistically significant predictors of postoperative hypothyroidism and HRT need. Although Bethesda classification, molecular testing and FNA pathology remain the guiding force in thyroid operative planning, our TSH-HRT risk categorization allows thyroid surgeons to perform a more informed consent, namely in regards to the development of post-operative hypothyroidism. By receiving their specific risk category, in prepping for future thyroid lobectomy, the patient can more reliably appreciate their chances of requiring lifetime HRT supplementation post-operatively.
CONCLUSION
Prior to thyroid lobectomy, preoperative TSH levels of >2.5 and presence of thyroiditis directly correlate to a significantly increased risk for HRT postoperatively. Conversely, TSH levels <2.0 predicts that it very unlikely that patient will require post-operative HRT. Therefore, in pre-operative counseling, surgeons can stratify the risk for post-operative HRT and thus more accurately inform their patients based on these high, moderate, and low risk categories. Our study was based on 100 retrospective thyroid surgeries performed in a single academic medical center and might not be generalized beyond similar patients. We did not evaluate the predictive value of preop TSH level in patient’s complication. Further studies including larger sample patient’s cohorts are essential to define the statistically significant predictors of postoperative hypothyroidism and HRT need.
ACKNOWLEDGEMENT
The authors would like to thank Dr. Susan Wu of South Nassau Communities Hospital Department of Pathology for providing specimens for data collection.
CONTRIBUTORS
JG conceived the study idea and performed the systematic review. RD designed the research strategy and evaluated risk of bias. YS reviewed abstracts and texts and helped conjoin submission. JG acquired the data and performed the data analysis. All authors reviewed the data analysis and critically revised the manuscript. All authors had the opportunity to review the final manuscript and gave their permission to publish the manuscript. All authors consent to take responsibility for the work. The corresponding author confirms that all listed authors meet authorship criteria.
DISCLOSURE OF POTENTIAL CONFLICTS OF INTERESTS
No Potential Conflicts of interest was disclosed.
FUNDING
This Guideline was not funded.
DATA SHARING
The lead author acknowledges that the manuscript is an honest and accurate study being reported; that no important features of the study have been excluded. This is an Open Access article which permits others to distribute, reproduce and modify this work non-commercially, and permits their derivative works, given the original work is properly cited and used is non-commercially.
REFERENCES
- Park HK, Kim DW, Ha TK, Choo HJ, Park YM, et al. (2015) Factors associated with postoperative hypothyroidism after lobectomy in papillary thyroid microcarcinoma patients. Endocr Res 40: 49-53.
- Jin J, Allemang MT, McHenry CR (2013) Levothyroxine replacement dosage determination after thyroidectomy. Am J Surg 205: 360-363.
- Stoll SJ, Pitt SC, Liu J, Schaefer S, Sippel RS, et al. (2009) Thyroid hormone replacement after thyroid lobectomy. Surgery 146: 554-558.
- Lee DY, Seok J, Jeong WJ, Ahn SH (2015) Prediction of thyroid hormone supplementation after thyroid lobectomy. J Surg Res 193: 273-278.
- Johner A, Griffith OL, Walker B, Wood L, Piper H, et al. (2011) Detection and management of hypothyroidism following thyroid lobectomy: evaluation of a clinical algorithm. Ann Surg Oncol 8: 2548-2554.
- Moon HG, Jung EJ, Park ST, Jung TS, Jeong CY, et al. (2008) Thyrotropin level and thyroid volume for prediction of hypothyroidism following hemithyroidectomy in an Asian patient cohort. World J Surg 32: 2503-2508.
- Morris LF, Iupe IM, Edeiken-Monroe BS, Warneke CL, Hansen MO, et al. (2013) Pre-operative ultrasound identification of thyroiditis helps predict the need for thyroid hormone replacement after thyroid lobectomy. Endocr Pract 19: 1015-1020.
Citation: Gauthier J, Shafizadeh Y, Datta R, D’cruz J, Seitelman E (2019) Stratifying Risk for Post-Operative Hormone Replacement Therapy (HRT): Pre-Operative Factors Predicting Hypothyroidism after Hemithyroidectomy. J Community Med Public Health Care 6: 058.
Copyright: © 2019 Justin Gauthier, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

