
Streptococcus Pseudoporcinus and Cardiac Implantable Electronic Device: Do We Need To Worry?? A Case Report.
*Corresponding Author(s):
Anthoula PlevritakiCardiology Department, University Hospital Of Heraklion, Heraklion, Greece
Tel:+302810392706,
Email:anthiplevritaki@gmail.com
Abstract
Streptococcus pseudoporcinus was first recognized as a colonizer of the female genital tract but upcoming cases with no genitourinary infections have been reported since then. Here we report a case of an 81-year old male with a recently implanted cardiac device that was diagnosed with infective endocarditis caused by S. pseudoporcinus.
Keywords
Bacteremia; β-hemolytic Streptococcus; Cardiac implantable device; Endocarditis; Hardware removal; Radiolabeled leucocyte scintigraphy; Streptococcus pseudoporcinusv
Abbreviations
CIED: Cardiac Implantable Electronic Device
IE: Infective Endocarditis
CDRIE: Infective Endocarditis related to Cardiac Device
ECG: Electrocardiography
AVB: Atrioventricular block
RBBB: Right bundle branch block
TTE: Transthoracic echocardiogram
TEE: Transesophageal echocardiogram
History of Presentation
An 81-year-old gentleman presented with a 2-day history of fevers and chills. On admission, he was febrile, with a body temperature of 37.6°C, tachypneic (respiratory rate: 30 breaths/minute) with 97% oxygen saturation on room air, and hemodynamically stable.
ECG showed sinus rhythm at 65 beats/minute, 1st degree AVB and RBBB. His physical examination was unremarkable, except for mild, diffuse abdominal tenderness on palpation.
White blood cells count was 11,700 cells/μl (normal range: 3.8-10.5 cells/μl) with 73.4% neutrophils, hemoglobin was 9.4g/dl (14-18 g/dl), platelets were 96,000 K/μl (150-450), erythrocyte sediment rate was 107 mm/hr and C-reactive protein was 8.66 mg/dl ( < 0.5). Creatinine was 1.91 mg/dl (0.72-1.18mg/dl) and urea 66 mg/dl (17- 43 mg/dl). Urinalysis demonstrated proteinuria and increased RBCs.
Past Medical History
His medical history included hypertension, hyperlipidemia, cholecystectomy, past exposure to asbestos, Hodgkin lymphoma, portal hypertension with hepato/splenomegaly, angiectasias, colon polyps, and a recent 2-months-old pacemaker implantation due to 3rd degree of AVB.
Medications included ASA 100mg, bisoprolol 2,5mg, ramipril 5mg and acetaminophen as needed.
Differential diagnosis
His presentation was suspicious for abdominal infection. Non-infectious syndromes such as inflammatory bowel diseases, ischemic colitis, and malignancies can also present with fever and diffuse abdominal pain, though.
Investigations
His chest and abdomen radiography were unremarkable. Ultra-sound and Computed tomography of the abdomen did not reveal relevant abnormal findings. Blood cultures were obtained while the patient was febrile and empiric antibiotic treatment was initiated.
Blood cultures were soon reported to contain Gram-positive cocci in chains.
A TTE demonstrated a normal ejection fraction with mild aortic stenosis and regurgitation and no evidence of valvular or lead vegetation. A TEE did not reveal signs of cardiac infection either (Figure 1).
 Figure 1: Tranesophageal Echocardiogram. Transesophageal echocardiogram did not reveal any vegetation on valves or pacer’s leads.
Figure 1: Tranesophageal Echocardiogram. Transesophageal echocardiogram did not reveal any vegetation on valves or pacer’s leads.
Vascular and immunological phenomena were investigated and fundoscopy revealed a Roth spot in the left eye.
Due to his recent cardiac device implantation, a radiolabelled leucocyte scintigraphy was performed, which was positive for lead infection (Figure 2).
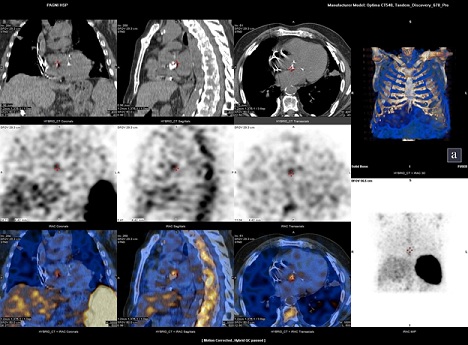 Figure 2: Radiolabelled Leucocyte Scintigraphy. 99mTc-HMPAO-WBC scintigraphy revealed the presence of CIED-associated infection.
Figure 2: Radiolabelled Leucocyte Scintigraphy. 99mTc-HMPAO-WBC scintigraphy revealed the presence of CIED-associated infection.
Streptococcus pseudoporcinus was later identified in three separate blood cultures.
Management
According to the existing guidelines, our patient met the modified Duke’s criteria for definitive endocarditis, one major (endocardial involvement) and three minor criteria (fever, Roth spot, and positive blood cultures with an organism not typically associated with endocarditis). The patient received 2gr intravenous ceftriaxone daily in accordance with the antimicrobial susceptibility testing.
Repeat blood cultures remained negative, and complete hardware removal (device and transvenous lead extraction) was performed after a prolonged (4-week) antibiotic therapy. Subsequent blood cultures along with hardware cultures were negative.
Optimal timing for reimplatantion of a new cardiac device was under consideration since there is a lack of experience regarding appropriate management of such infections. During his hospitalization, he experienced a new unprovoked episode of symptomatic 3rd degree AVB that was initially treated with isoproterenol.
Eventually, device reimplatantion was performed after 20days of hardware free interval and after 1-month antibiotic therapy completion.
Discussion
Streptococcus pseudoporcinus is a β-hemolytic Streptococcus first isolated from female genito-urinary tract in 2006; it can be CAMP- and Lancefield group B-positive and therefore can be misidentified as Streptococcus agalactiae. However S. agalactiae has a narrow zone of beta-hemolysis, is hippurate hydrolysis positive, is bile esculin hydrolysis negative, and does not produce acid from mannitol or sorbitol, unlike S. pseudoporcinus [1].
It was initially considered a colonizer of the female genital tract and cases of infection in men were associated with sexual activity [1-3].
First recordings demonstrated S.pseudoporcinus as an emerging pathogen for adverse maternal or neonatal outcomes in pregnancy [3-4]. Additionally, it has been reported as the virulent factor of soft tissue infections [1,5,15] or for more invasive infections, for instance bacteremia/infective endocarditis [6-9,13,15] and peritonitis [9]. In fact, 5 cases of S. pseudoporcinus related endocarditis have been identified through a thorough literature review [5-8], all involving native valves. No cardiac or other prosthetic device infection has been reported in the existing literature until now (Table 1).
|
Year of report |
Authors |
Patient Age(yrs)/Gender |
Type of Infection |
Site of isolation |
Antibiotic Regimen |
Outcome |
|
2009 |
Mahlen, Clarridge III |
33 M |
Thumb infection |
Wound purulence culture |
10d cephalexin |
Recovered |
|
2017 |
Fang, Gandhi |
77 M |
Subacute mitral valve endocarditis |
Blood cultures |
Ceftriaxone |
Unknown (Transferred to other hospital for valve replacement) |
|
2017 |
Gullet et al |
29 F |
Pregnancy complications/slow fetal growth/Preeclampsia |
Vaginorectal culture |
Nil |
Recovered |
|
2018 |
Sawamura et al |
94 F |
Cellulitis of left lower extremity |
Wound purulence culture |
Cefepime+Vancomycin due to multi drug resistance |
Recovered |
|
2019 |
Pierce et al |
41 F |
Singleton fetal demise/Acute necrotizing chorioamnionitis+acute umbilical vasculitis |
Urine, placenta, endometrium, 2 blood sets |
Ampicillin+gentamicin->D3 amoxicillin |
Recovered |
|
2020 |
Benzar |
35 M |
Aortic+mitral valve endocarditis/stroke_brain infracts |
2 blood sets |
Ceftriaxin+Vancomycin |
Deceased |
|
2020 |
Hai et al |
40 M |
Aortic valve infective endocarditis |
3 blood sets |
Cefepime 6gr+Ofloxacin 400mg |
Recovered+aortic valve replacement |
|
2020 |
Akagi et al |
40 M |
Pulmonary valve (CCTGA) encocarditis+ IgA vasculitis+septic pulmonary emboli |
2 blood sets |
Unknown+prednisolone |
Recoveredtransferred to the initial hospital |
|
2020 |
Khan et al |
81 M |
Cellulitis of right lower extremity /Aortic+mitral valve endocarditis |
Blood sets |
Ceftriaxone 2gr changed to Vancomycin |
Deceased |
|
2020 |
Khan et al |
72 F |
Pneumonia |
Lung tissue, pleural fluid |
Ceftriaxone 1gr changed to Ertapenem 1gr (coinfection) |
Recovered |
|
2020 |
Gupta et al |
43 M |
Bacteremia |
Blood sets |
Ceftriaxone 2gr |
Unknown |
|
2021 |
Vergadi et al |
9 M |
Cellulitis of right lower extremity/Bacteremia |
Blood sets |
Ceftriaxone+Vancomycin->Clindamycin+Vancomycin 14d |
Initially recovered-Cellulitis relapsed – discharged with 3-mo chemoprophylaxis |
|
2021 |
Liatsos et al |
56 M |
Spontaneous bacterial peritonitis (SBP) +bacteremia |
Blood+ascitic fluid cultures |
Meropenem 3gr+Daptomycin 350mg |
Deceased |
|
2022 |
Russo et al |
45days infant |
Relapsing cervical lymphadenitis |
Blood cultures |
Ceftriaxone and oxacillin changed to ampicillin, followed by oral amoxicillin |
Initially clinical improvement-disharged- cervical lymphadenitis. relapsed – workup for immunodeficiency- CD4 levels below 3rd percentile |
|
2022 |
Venincasa et al |
59 F |
Endophthalmitis – 3ws after a bilateral upper and lower blepharoplasty |
Vitreous culture |
Intravitreal injection of vancomycin and ceftazidime |
Postoperative vision improved to 5/200 but was limited by a full-thickness macular hole. |
|
2023 |
Birlutiu et al |
63 M |
Endocarditis / Mastocytosis and Spondylodiscitis |
Blood sets |
Ceftriaxone 2g +Vancomycin 2g |
Ceftriaxone for up to 4wks, levofloxacin 750 mg/d at discharge for 2 mo for spondylodiscitis |
|
2023 |
Dong, Tian |
Nil |
Orbital cellulitis -Corneal perforation |
Pus culture |
Nil |
aggressive anti-infection+surgical treatment |
|
2023 |
Papapanagiotou et al |
67 M |
Bacteremia - soft tissue infection of left lower limb |
2 Blood sets |
Ceftriaxone 2gr (2 weeks) |
Recovered |
|
2024 |
Plevritaki et al |
81 M |
Endocarditis due to Cardiac Implantable Electronic Device Infection |
3 Blood sets |
Ceftriaxone 2gr |
Recovered-New device was implanted |
Table 1: Review of cases in the literature.
Given the great similarities with Group B Streptococcus (Streptococcus agalactiae) [1] one could suppose a similar epidemiological and clinical behavior of both. Thus, they could represent an important cause of invasive infections in high-risk populations, especially in pregnant women, neonates, and the elderly and in individuals with underlying medical conditions such as diabetes, cirrhosis and cancer.
Although Streptococcus species are commonly associated with endocarditis, this is the first known report of Streptococcus pseudoporcinus causing infective endocarditis related to cardiac device.
S. pseudoporcinus can been isolated from human rectum, upper respiratory and genital tracts [3,5]. The definitive source of our patient’s S. pseudoporcinus is unclear. We postulate that it may have originated via gastrointestinal colonization and subsequent bacteremia due to his known angiectasias and splenomegaly.
Last but not least, according to ESC guidelines, clinical presentation of CDRIE is frequently ambiguous and echocardiography and blood cultures are the cornerstones of diagnosis. A normal TTE does not rule out CDRIE and high suspicion is needed in the presence of unexplained fever in a patient with a CIED, whereas additive tools may be needed, such as radiolabelled leucocyte scintigraphy and 18F-FDG PET/CT scanning [10].
Follow-up
His postoperative course was uneventful. A 3-month overall antibiotic therapy was completed without any adverse concerns.
Conclusion
This is the first reported case of Streptococcus pseudoporcinus causing Infective Endocarditis related to Cardiac Device.
Knowledge is limited regarding these recently differentiated novel species, and thus, reporting of previously unknown S.pseudoporcinus infection manifestations is of utmost importance. Accordingly, the present report extends current knowledge regarding the ability of S.pseudoporcinus to infect prosthetic materials and will, hopefully, raise the level of suspicion of cardiac or other prosthetic device infection in patients with persistent bacteremia. Moreover, given the lack of relevant experience and the successful outcome of the applied management course, this case could be used as a management/treatment guide, until consensus for such cases has been reached.
Learning Objectives
- To recognize Infective Endocarditis related to Cardiac Device and to raise the level of suspicion for IE in patients with a CIED and unexplained fever.
- To understand that normal echographic examination does not rule out CDRIE and additive tools may be needed (radiolabelled leucocyte scintigraphy, 18F-FDG PET/CT scanning).
- To discuss how bacteremia by an uncommon bacterium, Streptococcus pseudoporcinus can cause Infective Endocarditis related to Cardiac Device.
Disclosure
The authors have nothing to disclose.
Funding
No funding.
References
- Mahlen SD, Clarridge III JE (2009) Thumb infection caused by Streptococcus pseudoporcinus. J Clin Microbiol. 47: 3041.
- Gupta K, Mohanty M, Rath S (2020) Bacteremia because of Streptococcus pseudoporcinus in a Syphilis-HIV co-infected patient: A case report. J Family Med Prim Care. 9: 2119-2120.
- Grundy M, Suwantarat N, Rubin M, Harris R, Hanlon A, et al. (2019) Differentiating Streptococcus pseudoporcinus from GBS: could this have implications in pregnancy? Am J Obstet Gynecol. 220: 490.e1-490.e7.
- Pierce SL, Shibib DR, Robison D, Edwards RK (2019) A Case of Maternal Sepsis and Fetal Demise Associated with Streptococcus pseudoporcinus. Case Rep Obstet Gynecol. 2019: 4309191.
- Khan S, Wong TT, Prasad N, Lee B, Urban C, et al. (2020) Streptococcus pseudoporcinus: Case Reports and Review of the Literature. Case Rep Infect Dis. 22: 4135246.
- Benzar R (2020) 595: Streptococcus Pseudoporcinus: A Novel Pathogen In A Fatal Case Of Aortic And Mitral Endocarditis. Crit Care Med. 48: 278.
- Hai PD, Dung NM, Son PN, Phuong LL, Thuyet BT, et al. (2020) First report of infective endocarditis caused by Streptococcus pseudoporcinus in Vietnam. New microbes New infect. 34: 100643.
- Akagi M, Iwanaga N, Torisu Y, Fujita H, Kawahara C, et al. (2020) IgA Vasculitis Triggered by Infective Endocarditis of Pulmonary Artery with Congenitally Corrected Transposition of the Great Arteries. Int Heart. 61: 404-408.
- Liatsos GD, Tsiriga A, Dourakis SP (2021) Fatal Streptococcus pseudoporcinus disseminated infection in decompensated liver cirrhosis: a case report. J Med Case Rep. 15: 240.
- Delgado V, Ajmone Marsan N, de Waha S, Bonaros N, Brida M, et al. (2023) 2023 ESC Guidelines for the management of endocarditis: Developed by the task force on the management of endocarditis of the European Society of Cardiology (ESC) Endorsed by the European Association for Cardio-Thoracic Surgery (EACTS) and the European Association of Nuclear Medicine (EANM). Eur Heart J. 44: 3948-4042.
- Russo DO, Marques BA, Rodrigues TD, de Souza Fernandes G, do Nascimento PHO (2022) Extensive Relapsing Cervical Lymphadenitis Due to Streptococcus Pseudoporcinus in an Infant. Pediatr Infect Dis J. 41: e272-e274.
- Venincasa MJ, Shoji MK, Al-Khersan H, Maeng MM, Johnson TE, et al. (2022) Acute onset endophthalmitis following bilateral upper and lower eyelid blepharoplasty. Ophthalmic Plast Reconstr Surg. 38: e131-e133.
- Birlutiu V, Birlutiu RM, Teodoru M, Catana AC, Stoica CI (2023) Endocarditis with Streptococcus pseudoporcinus Associated with Mastocytosis and Spondylodiscitis-A Coincidental Association? A Case Report. Trop Med Infect Dis. 8: 247.
- Dong Y, Tian M (2023) Case Report: Corneal perforation secondary to orbital cellulitis caused by Streptococcus pseudoporcinus Eur J Ophthalmol. 33: NP66-NP69.
- Papapanagiotou M, Ioannou P, Alexakis K, Maraki S, Papadokostaki E, et al. (2023) Streptococcus pseudoporcinus bacteremia in a patient with skin and soft tissue infection. A case report and literature review. Infez Med. 31: 399-403.
Citation: Plevritaki A, Zervakis S, Patrianakos A, Bizymi N, Kapsoritakis N, et al. (2024) Streptococcus Pseudoporcinus and Cardiac Implantable Electronic Device: Do We Need To Worry?? A Case Report. J Clin Stud Med Case Rep 11:229
Copyright: © 2024 Anthoula Plevritaki, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

