
Surgical Management of Recurrent Giant Ameloblastoma of the Mandible: A Case Report
*Corresponding Author(s):
Akbar I KhasanovRepublican Specialized Scientific And Practical Medical Center Of Oncology And Radiology (RSSPMCOR), Ministry Of Health, Tashkent, Uzbekistan
Tel:+998935709321,
Email:akbarkhasanov@mail.ru
Abstract
Ameloblastoma is the most common odontogenic tumor, characterized by locally invasive growth and a high tendency for recurrence. This report describes the clinical case of a recurrent ameloblastoma of the mandible that developed over 14 years following three prior surgical interventions. Is of an extremely unusual case. The tumor reached a giant size (15×10 cm), causing significant deformity and functional impairment of the mandible. The patient was treated with a subtotal resection of the mandible with defect reconstruction using local tissues. This case highlights the importance of a comprehensive surgical approach and timely diagnosis to prevent the recurrence of ameloblastoma.
Keywords
Recurrent Mandibular Ameloblastoma; Surgical Treatment; The Tumor is Gigantic
Introduction
Ameloblastoma is recognized as the most common type of odontogenic tumor, with up to 80% of clinical cases located in the mandible [1]. A key feature of ameloblastoma is its locally aggressive growth, demonstrating an ability to infiltrate surrounding bone and soft tissues, which complicates therapy and necessitates a radical treatment approach. Despite its benign nature, it can transform into ameloblastic carcinoma. In most cases, the tumor presents as a multilocular lesion with cystic cavities, appearing on radiographs with a characteristic "soap bubble" pattern. Treatment depends on the size and type of the tumor; small, benign ameloblastomas may be removed by enucleation, but this approach is associated with a high risk of recurrence. For large tumors [2-4], segmental resection of the mandible is employed, which reduces the likelihood of recurrence, especially in cases involving soft tissue [5]. According to the 2017 World Health Organization (WHO) classification, ameloblastoma is a benign odontogenic tumor of epithelial origin, developing from cells of the dental lamina [2]. The fifth edition of the WHO Classification of Head and Neck Tumours, introduced in 2022 and updated in 2024, differentiates ameloblastoma into five clinical variants: conventional (solid/multicystic), unicystic, peripheral (extraosseous), metastasizing adenoid. These forms exhibit differences in morphological characteristics, clinical course, degree of aggressiveness and tendency to recur [2-4]. This case demonstrates the aggressive, recurrent course of a mandibular ameloblastoma, which, despite three previous surgeries, continued to progress, reaching a giant size with deformity of the mandible and oral cavity and impairment of its functions. The long-term growth of the tumor (since 2002) and previous non-radical surgeries necessitated a subtotal resection of the mandible with defect reconstruction, making this case a rare example of an advanced recurrent ameloblastoma. We present this clinical case of a patient who was successfully treated with surgery [6-10].
Case Presentation
A male patient, born in 1974, was admitted to the Department of Head and Neck Tumor Surgery with complaints of a giant mass in the mandible region, constant discharge from the lower part of the mass and weakness (Figure 1).
 Figure 1: Patient before treatment. Anterior and lateral projections.
Figure 1: Patient before treatment. Anterior and lateral projections.
History of Present Illness
According to the patient, the mass first appeared in 2002 and gradually increased in size. In 2003, 2006 and 2008, he underwent surgical removal of the tumor at a dental clinic in the Fergana region; histology confirmed ameloblastoma. Starting in 2014, a rapid growth of the neoplasm was observed, reaching a giant size for head and neck tumors and causing functional impairment of the mandible. Due to the progression of the disease, the patient sought specialized oncological care at the Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology in Tashkent on February 19, 2016.
Physical Examination
Examination revealed a giant tumor measuring 15×10 cm (Figure 1), located in the region of the mandible and chin and partially extending to the neck. The mass was of a dense, elastic consistency, with limited mobility and clear borders. The overlying skin was intact; however, a fistula with a diameter of 1×1.5 cm with constant, light-brown discharge was identified at the lower pole. Examination of the oral cavity revealed deformation of the floor of the mouth due to the mass, significant tooth mobility and restricted movement of the mandible. Nasal breathing was unimpeded. Food intake was difficult.
Imaging and Diagnosis
A CT scan from February 11, 2016, showed a large, 14.4x10 cm mass in the projection of the mandible with a heterogeneous structure and a cystic component of +9 to +24 to +41 Hounsfield Units with irregular contours (Figure 2). Preoperative histology (No 1123 b/16) confirmed Ameloblastoma.Based on the research data obtained, the following preoperative diagnosis was established: Ameloblastoma of the mandible (Solid type). Status post three surgeries (2003, 2006, 2008 in Fergana). Recurrence, locally advanced form.
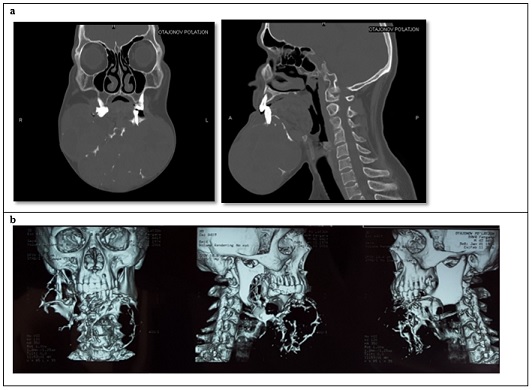 Figure 2a: CT scan in two projections. Large formation in the mandible region. 2b. Three-dimensional reconstruction of the patient's computed tomography scan.
Figure 2a: CT scan in two projections. Large formation in the mandible region. 2b. Three-dimensional reconstruction of the patient's computed tomography scan.
Surgical Planning and Procedure
Considering the clinical and diagnostic data, the giant size of the tumor and its recurrence (and also taking into account the absence of an operating microscope in the clinic), a two-stage treatment was planned:
- Stage I:Subtotal resection of the mandible with reconstruction of the postoperative oral defect using local tissues.
- Stage II:(Planned for 1-2 months later) Reconstructive plastic surgery using titanium plates and vascularized free fibula bone grafts.
On March 2, 2016, the patient underwent Stage I surgery: subtotal resection of the mandible with reconstruction of the oral defect using local tissues. The surgical approach was achieved by excising a skin-subcutaneous flap 22 cm in length from the right ear to the angle of the left side of the mandible (Figure 3). The tumor involved the right half of the mandible up to its ramus and extended to the left angle, causing destruction of the bone tissue.
 Figure 3: Surgical incisions marked with brilliant green, necessary for exposure of the mandible with the tumor.
Figure 3: Surgical incisions marked with brilliant green, necessary for exposure of the mandible with the tumor.
Given the massive involvement, the mandible was removed as a single block with the adjacent tissues (Figure 4a, 4b &4c).
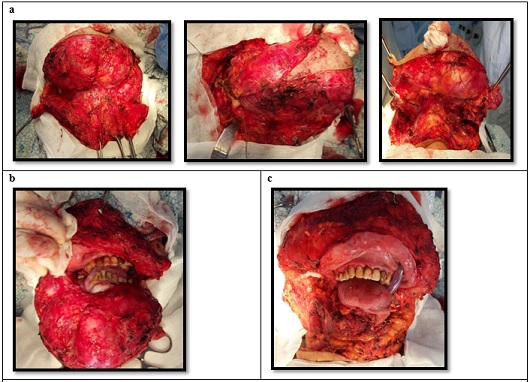 Figure 4: a – stages of tumor exposure; b – dissected tumor; c – surgical defect after subtotal resection of the mandible.
Figure 4: a – stages of tumor exposure; b – dissected tumor; c – surgical defect after subtotal resection of the mandible.
The mandibular defect was repaired with local tissues, ensuring a watertight seal of the mucous membrane (Figure 5).
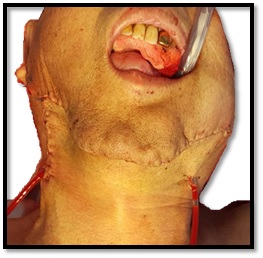 Figure 5: Condition after reconstruction of the postoperative bed with local tissues.
Figure 5: Condition after reconstruction of the postoperative bed with local tissues.
Pathology
On gross examination, the tumor had the shape of the mandible and was convex. On sectioning, the tumor showed a heterogeneous structure with a cystic component containing light-brown transparent fluid. The tumor measured 15×12×10 cm and was sent for histological examination (Figure 6).
 Figure 6: Gross specimen. Resected tumor.
Figure 6: Gross specimen. Resected tumor.
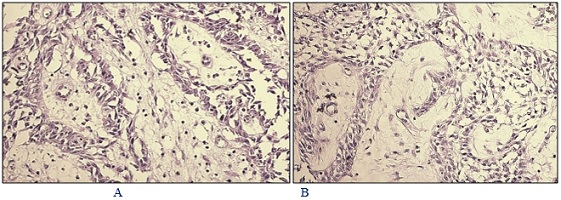 Figure 7: Postoperative Histology (No 2530-33 o/16): Ameloblastoma, Follicular type.
Figure 7: Postoperative Histology (No 2530-33 o/16): Ameloblastoma, Follicular type.
Microscopic Description (Figure 7): (A-B) Follicular type tumor with discrete islands of epithelial cells located in a connective tissue stroma. The central portions of the follicles consist of clusters of polygonal cells resembling the pulp of a dental organ. The cells of the outer epithelial layer of the follicles are of various sizes. In the central zones of the follicles, there is an accumulation of reticular cells. H&E stain. Magnification 100x.
Postoperative Course
The postoperative course was satisfactory, with primary wound healing (Figure 8). The aesthetic result was improved, but due to the absence of the mandible, a defect in the lower facial zones was noted. The patient was discharged home. The patient did not appear for the second reconstructive stage of the operation after 1-2 months.
 Figure 8: Condition 10 days after removal of drainage tubes.
Figure 8: Condition 10 days after removal of drainage tubes.
Discussion
Ameloblastoma is an odontogenic tumor with locally destructive growth, often leading to recurrence. The risk of recurrence largely depends on the morphological variant of the tumor [1,11]. The choice of surgical tactics for ameloblastomas is dictated by their localized but aggressive growth pattern and the high frequency of recurrence with inadequate resection [12]. The optimal treatment method is considered to be resection with a mandatory margin of at least 1–1.5 cm from the visible borders of the neoplasm, which includes segmental resection of the mandible or maxillectomy in cases of corresponding involvement [13]. The use of conservative interventions—such as enucleation, curettage, or marsupialization—is associated with a risk of leaving residual tumor cells and is not considered a definitive treatment approach [14]. Recurrence of ameloblastoma depends on the treatment method and the morphological characteristics of the tumor. With curettage and enucleation, it reaches 90%, whereas after radical resection with an adequate margin, it is less than 15%. Even with radical intervention, late recurrences are possible (15–25%), which necessitates long-term follow-up. Key factors for recurrence are residual tumor, follicular or plexiform structure, invasion into soft tissues and maxillary location. The embryonic origin of the tumor enhances its tendency for regrowth [5,10]. In our case, the ameloblastoma was of the follicular variant morphologically, which contributed to the high frequency of recurrences. The patient had undergone three surgeries for ameloblastoma of the mandible in 2003, 2006 and 2008 at his local clinic, which involved enucleation of the tumor while preserving the integrity of the mandible. As is known, such a scope of operation is accompanied by a high risk of recurrence (55–90%), whereas radical removal can lead to significant aesthetic and functional deficits requiring reconstruction with free flaps.
Diagnosis of ameloblastoma is based on histological and radiological examination. The most common location of the tumor is the body, angle and ramus of the mandible, where it is easily detected by Orthopantomography (OPG) and Computed Tomography (CT). In most cases, ameloblastoma appears as a multilocular radiolucent area (55.73% of cases according to OPG data) [8]. Ameloblastoma demonstrates a wide range of sizes—from 1 to 16 cm, with average values varying between 4–7 cm. It most often presents as a slowly enlarging neoplasm, causing deformation of the jaw arch and progressive destruction of the adjacent bone tissues. Solid and multicystic variants are the most common and can involve a significant portion of the jaw, including the body and ramus of the mandible. The typical location is the posterior segment of the mandible, with possible extension to the coronoid and condylar processes. Without timely treatment or in cases of late detection, the tumor can reach significant volumes, destroying neighboring anatomical structures [7]. In this clinical case, the patient's tumor measured 15×10 cm, causing discomfort during eating and speech, as well as functional impairment of the mandible.
With conservative treatment of ameloblastoma, the recurrence rate is twice as high as with radical surgical treatment [5]. The problem of ameloblastoma recurrence begins at the diagnostic stage when the treatment strategy is decided. In some cases, a biopsy is performed before surgical intervention to confirm the diagnosis and determine the histological type of the tumor, which allows for a choice between radical and conservative approaches. In other cases, a conservative resection biopsy is performed without the possibility of a full intraoperative histological analysis and the need for radical treatment is determined either by the results of the final histological examination or after a period of dynamic observation [5]. If there is perforation of the cortical layer and infiltration of soft tissues by the ameloblastoma, it is necessary to carefully determine the boundaries for their removal. Despite the presence of a connective tissue barrier between the tumor and surrounding tissues, it cannot be considered a true capsule, which requires excision of the affected soft tissues up to the nearest anatomical boundary [7,13]. The presence of a fistulous tract, as well as the size of the tumor and its growth into the surrounding skin, necessitated the excision of soft tissues with subsequent reconstruction.
Segmental resection of the mandible with immediate reconstruction is considered the optimal approach in the treatment of ameloblastoma, as it significantly reduces the probability of recurrence, helps restore masticatory function and improves the patient's overall quality of life. Early reconstruction plays a key role in preventing the formation of cavities with the risk of infectious complications, as well as soft tissue deformity that can negatively affect the ability to eat, swallow and articulate [6,12,15]. In this case, a subtotal resection of the mandible was performed with defect reconstruction using local tissues. Thus, for the successful treatment of ameloblastoma, it is necessary to consider the morphological variant of the tumor, conduct a thorough histological diagnosis and apply radical surgical methods in the presence of aggressive forms of the tumor. This allows for a reduction in the risk of recurrence and ensures a favorable prognosis for the patient.
Conclusion
Ameloblastoma possesses high aggressiveness and a tendency to recur, which demands precise histological diagnosis and careful selection of treatment tactics. Conservative methods (marsupialization, enucleation, curettage) preserve bone integrity but are accompanied by a high risk of recurrence (55–90%), whereas radical removal can lead to significant aesthetic and functional impairments requiring reconstruction with free flaps.
References
- Shah JP, Patel SG, Singh B, Wong R (2020) Jatin Shah’s Head and Neck Surgery and Oncology.
- Speight PM, Takata T (2017) New tumour entities in the 4th edition of the World Health Organization Classification of Head and Neck tumours: odontogenic and maxillofacial bone tumours. Virchows Arch 472: 331-339.
- Nosé V, Lazar AJ (2022) Update from the 5th Edition of the World Health Organization Classification of Head and Neck Tumors: Familial Tumor Syndromes. Head Neck Pathol 16:143-157.
- WHO Classification of Tumours Editorial Board (2024). Head and Neck Tumours. WHO Classification of Tumours, 5th ed. Vol. 9. IARC WHO; Lyon, France: 2024.
- Laborde A, Nicot R, Wojcik T, Ferri J, Raoul G (2017) Ameloblastoma of the jaws: Management and recurrence rate. European Annals of Otorhinolaryngology, Head and Neck Diseases 134: 7–11.
- Vayvada H, Mola F, Menderes A, Yilmaz M (2006) Surgical Management of Ameloblastoma in the Mandible: Segmental Mandibulectomy and Immediate Reconstruction With Free Fibula or Deep Circumflex Iliac Artery Flap (Evaluation of the Long-Term Esthetic and Functional Results). J Oral Maxillo Surg 64: 1532–1539.
- Chae MP, Smoll NR., Hunter-Smith DJ, Rozen WM (2015) Establishing the natural history and growth rate of ameloblastoma with implications for management: systematic review and meta-analysis. PLoS One
- Rahman AFMS, Haider IA (2022) Ameloblastoma of the Jaws: A Retrospective Observational Study of 131 Cases at a Tertiary Level Hospital in Bangladesh. J Den Res Rev 9: 59-65.
- Mishra, Darshana P, Kumar R, Govind N, Kumar A, et al. (2022) Desmoplastic ameloblastoma of maxilla - A case report. SRM Journal of Research in Dental Sci 13: 76-79
- Almeida RDAC, Andrade ESDS, Barbalho JC, Vajgel A, Vasconcelos BCD (2016) Recurrence rate following treatment for primary multicystic ameloblastoma: systematic review and meta-analysis. Int J Oral Maxillofac Surg 45:359-367
- Shen W, Xu C, Wang P, Chen J, Yu D, et al. (2023) Giant Mandibular Ameloblastoma with Rare Hypercalcemia: A Case Report and Literature Review. Medicina (Kaunas) 59: 1956.
- Wu K, Luo H, Yuan Z, Qui X, et al. (2022) Clinical evaluation of fenestration decompression combined with secondary curettage for ameloblastoma of the jaw: retrospective radiographic analysis. BMC Oral Health22: 443
- Ghai S (2022) Ameloblastoma: An Updated Narrative Review of an Enigmatic Tumor. Cureus 14:27734.
- Rayamajhi S, Shrestha S, Shakya S, Bhandari S, Twayana AR, et al. (2022) Unicystic Ameloblastoma of Mandible: A Case Report. JNMA J Nepal Med Assoc 60: 657-660.
- Zhang J, Shan Y, Zhang Y, Ye X, Song Y, et al. (2025) Analysis of factors influencing the psychological status and cognitive function of postoperative head and neck tumor patients. Sci Rep 15: 9072.
Citation: Khasanov AI, Khasanov AI, Nishonboyev L, Akhror Madaliev AY, Hafizova D, et al. (2025) Surgical Management of Recurrent Giant Ameloblastoma of the Mandible: A Case Report. HSOA J Otolaryngol Head Neck Surg 11: 113.
Copyright: © 2025 Akbar I Khasanov, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

