
Surgical Treatment of Malignant Transformation Tumors of the Parotid Salivary Gland of the Large Size from 30 Years Ago
*Corresponding Author(s):
Akbar I. KhasanovHead Of The Department Of The Head And Neck Cancers Department, Republican Specialized Scientific Practical Medical Center Of Oncology And Radiology (RSSPMCO&R) MoH RUz, Tashkent, Uzbekistan
Tel:+998935709321,
Email:akbarkhasanov@mail.ru
Abstract
Tumors of the parotid salivary gland are associated with facial deformity. Large tumors can lead to significant facial disfigurement. Some tumors can also damage the facial nerve, leading to facial nerve palsy and interfering with functions such as eye movements and talking. This case is about a 73-year-old woman with a tumor of the left parotid salivary gland, which appeared approximately 30 years ago and was untreated. Considering the patient's age and concomitant comorbid conditions, subtotal resection of the large parotid salivary gland was performed. Postoperative histology revealed that the tumor cells were consistent with Pleomorphic adenoma with malignant transformation. Although rare, malignant transformation in this patient likely arose from the long history of the tumor. Our clinical example is corroborated by available research data.
Keywords
Malignant transformation; Parotid salivary gland, Pleomorphic adenoma; Surgical treatment
Introduction
New salivary gland formations are rare and account for approximately 3-6% of all head and neck tumors. The incidence of salivary gland cancer in the United States is approximately 2.5-3 cases per 100,000 populations per year [1].
In 2021, for the first time, 125 cases of malignant tumors of the salivary glands were recorded in the Republic of Uzbekistan, with an incidence of 0.4 per 100,000 populations [2].
Pleomorphic adenoma is the most common benign neoplasm of the salivary glands [3]. However, pleomorphic adenoma can undergo malignant transformation into ex pleomorphic adenoma [4-6]. The risk of malignant transformation increases with longstanding tumors.
Untreated large parotid salivary gland tumors are rare, and this clinical case highlights a patient with a 30 year-old pleomorphic parotid salivary gland adenoma with malignant transformation who successfully underwent surgery.
Case Report
This is a 73-year-old patient who contacted the Ferghana regional branch of RSSPMCO&R MoH RUz, Ferghana, Uzbekistan, in May 2022 with complaints of a large hanging mass in the left parotid region and the presence of a bloody wound on the skin of the inferior side of the mass (Figure 1).
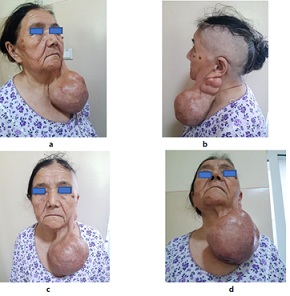 Figure 1: Patient 73 years before treatment.
Figure 1: Patient 73 years before treatment.
From history, the tumor appeared 30 years ago and initially grew slowly. Recently, however, the tumor began to grow quickly. Since it was painless, the patient did not visit a physician for evaluation. Between April-May 2022, an open wound appeared on the inferior side of the tumor and had associated intermittent bleeding, prompting the patient to seek medical care. Preoperative clearance was obtained, and the patient was scheduled for surgery a month in advance, keeping in consideration factors such as older age, continuous bleeding from the tumor, and history of poorly controlled hypertension. After the bleeding wound healed and hypertension was successfully treated, the patient underwent surgical resection.
Preoperative Multiple-Slice Computed Tomography (MSCT) of head, dated 05.11.2022 (Figure 2), showed parotid and cervical region on the left with multiple formations of a rounded irregular mass, measuring from 18×24 mm to 93×108 mm. Density + 34+64 µN. The contours are uneven. Conclusion: CT signs of multiple parotid salivary gland lesions on the left.
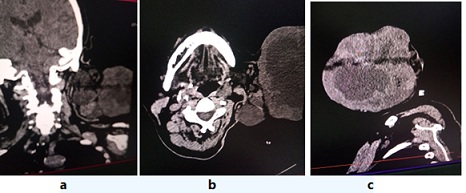 Figure 2: CT in 3 projections. A large tumor emanating from the left parotid salivary gland.
Figure 2: CT in 3 projections. A large tumor emanating from the left parotid salivary gland.
Fine-needle aspiration cytology (FNAC) revealed a salivary gland tumor that is uncertainly benign (Milan classification 4b). Suspicion for salivary gland pleomorphic adenoma.
Ultrasound examination of the left parotid region on 05.11.2022 revealed a mixed echogenic multiple formations of sizes ranging from 20×25 mm to 95×120 mm. Nodes of the ear area with dimensions of 35 x 26 mm are also defined. Peripheral lymph nodes are not visualized.
Status localis: on the left parotid region there is a large hanging tumor and on the inferior side of the tumor a healed wound is identified (Figure 1). The overall tumor size is 22×12×12cm and consists of several parts. The largest tumor formation resembles the shape of a hanging ball. Despite the large size of the tumor, there was no weakness (paresis) of facial muscles innervated by the facial nerve. Regional lymph nodes were not palpable.
After FNAC, the patient was diagnosed with pleomorphic adenoma of the left parotid salivary gland and underwent subtotal resection of the left parotid salivary gland in June 2022. Tumor was resected carefully to avoid integrity of the branches of the facial nerve. In the postoperative period, a satisfactory aesthetic and functional result was achieved without signs of facial paralysis, and the patient was discharged home. Figure 3 shows the gradual removal of the parotid salivary gland.
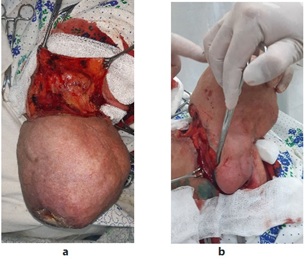 Figure 3: Phased removal of the left parotid salivary gland.
Figure 3: Phased removal of the left parotid salivary gland.
When examining the macro-preparation, the tumor has an oval shape measuring 22×12×12 cm. The middle section revealed tumor decay with hemorrhagic fluid (Figure 4).
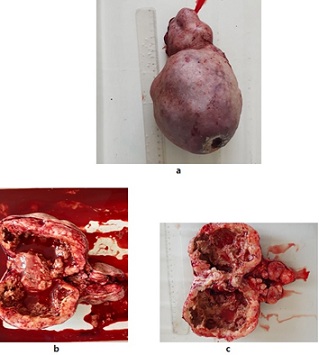 Figure 4: Macro-preparation: a. Resected tumor, b. Tumor in the section view, c. Tumor in the sectional view after removal of hemorrhagic contents.
Figure 4: Macro-preparation: a. Resected tumor, b. Tumor in the section view, c. Tumor in the sectional view after removal of hemorrhagic contents.
Histopathological examination reported two components of the tumor - epithelial and mesenchymal (myxoid); ducts from epithelial, located in several layers dissolve in the myxoid stroma. Evidence of foci of extensive inflammation and necrosis, angular fusiform nuclei, some hyperchromicity with an increase in mitotic figures and some cellular atypia.
Postoperative Histology 5798-5809/2022: Pleomorphic adenoma with malignization (Figure 5).
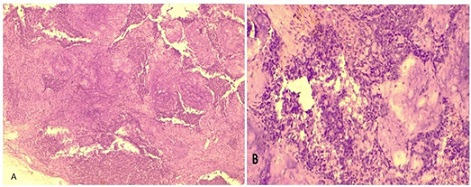 Figure 5: A. Histopathology. Ducts from epithelial cells, located in several layers, dissolve in the myxoid stroma. Uv.200. H&E. B. sites with extensive inflammation and necrosis, angular fusiform nuclei, enlargement of mitotic figures, and some cellular atypia. Uv.400. H&E.
Figure 5: A. Histopathology. Ducts from epithelial cells, located in several layers, dissolve in the myxoid stroma. Uv.200. H&E. B. sites with extensive inflammation and necrosis, angular fusiform nuclei, enlargement of mitotic figures, and some cellular atypia. Uv.400. H&E.
The postoperative course was uneventful (Figure 6).
 Figure 6: Same patient 20 days after surgery.
Figure 6: Same patient 20 days after surgery.
Discussion
Patients with a long-existing pleomorphic adenoma that begins to grow rapidly or become painful are rare, suggesting the development of cancer growing in the primary tumor via malignant transformation of the pleomorphic adenoma. Histologically, it will be a clearly malignant tumor, usually a low-differentiated adenocarcinoma, mucoepidermoid cancer, or another type of malignant tumor [1]. In this case, the histology results suggested that the pleomorphic adenoma had a malignant transformation over time.
Salivary gland tumors can be complex and vary in terms of their morphological spectrum. Although this type of tumor is most frequently encountered, it is still rare (European Standardized rate: 4.5/100,000 as opposed to 62/100,000 seen in breast cancer) [7]. The diagnosis can be challenging owing to its morphological similarity with features of other 22 salivary gland carcinomas [8-10].
However, a notorious feature among these cancers is the malignant transformation of the most common salivary gland tumor, pleomorphic adenoma, to carcinoma ex-pleomorphic adenoma, which is the fifth most common salivary gland tumor [10-12]. This diagnosis is made based on finding pleomorphic adenoma components in the malignant tumors and are therefore classified as carcinoma ex-pleomorphic adenoma. The morphological as well as molecular transitions are seen from the benign pleomorphic adenoma component to the malignant carcinoma component [10,13-17].
This type of neoplasm can lead to dilemmas in both pathological diagnosis and surgical/adjuvant radiation treatment of primary and recurrent pleomorphic adenoma. This risk of malignant transformation is, however, rare, as only 3% of salivary pleomorphic adenomas recur at 12.5-year follow-up, of which approximately 6% seem to show malignant transformation [11]. Furthermore, Valstar MH, et al noted that a malignant transformation occurred in 1.1% of primary and 0.15% of secondary salivary gland pleomorphic adenomas after 5 years of dynamic follow-up (3.2% of all relapses) [7]. Similar results were seen from a study in Denmark, showing 1.7% malignant transformation with a mean 6.2% risk, but the data was acquired from a single-center study, which can reflect a referral bias [10,18,19].
Conclusion
Malignant transformation of pleomorphic adenoma of parotid gland can occur over a long period of time. Left untreated, pleomorphic adenomas can continue growing in size, increasing the risk of malignant transformation. The frequency of malignant transformation, however, varies, based on different study results. This case report highlights that within 30 years of untreated tumor growth, malignant transformation occurred as was evidenced by morphological features of the tumor as well as histological examination. The main method of treatment is surgical removal of the tumor.
References
- Shah J, Patel S, Singh B (2016) Jatin Shah's Head and Neck Surgery and Oncology. Pp. 812.
- Tillyashaykhov MN, Ibragimov SN, Dzhanklich SM (2022) State of cancer care for the population of the Republic of Uzbekistan in 2021. Tashkent pp. 175.
- Reiland MD, Koutlas IG, Gopalakrishnan R, Pearson AG, Basi DL (2012) Metastasizing pleomorphic adenoma presents intraorally: a case report and review of the literatur. J Oral Maxillofac Surg 70: 531-540.
- Hay MA, Witterick IJ, Mock D (2001) Recurrent pleomorphic adenoma of the parotid gland with cervical metastasis. J Otolaryngol 30: 361-365.
- Nouraei SA, Ferguson MS, Clarke PM (2006) Metastasizing pleomorphic salivary adenoma. Arch Otolaryngol Head Neck Surg 132: 788-793.
- Knight J, Ratnasingham K (2015) Metastasising pleomorphic adenoma: Systematic review. Int J Surg 19: 137-145.
- Valstar MH, de Ridder M, van den Broek EC, Stuiver MM, van Dijk BAC, et al. (2017) Salivary gland pleomorphic adenoma in the Netherlands: a nationwide observational study of primary tumor incidence, malignant transformation, recurrence, and risk factors for recurrence. Oral Oncol 66: 93-99.
- El-Naggar A, Chan J, Takata T, Slootweg PJ (2017) WHO Classification of Tumours. Pathology and Genetics of Head and Neck Tumours. 4th edn, IARC Press, Lyon, 2017.
- Hernandez-Prera JC, Skálová A, Franchi A, Rinaldo A, Poorten VV, et al. (2020) Pleomorphic adenoma: the great mimicker of malignancy. Histopathology 79: 279-290.
- Valstar MH, Mast H, Hove I, Moonen LR, Balm AJ, et al. (2021) Malignant transformation of salivary gland pleomorphic adenoma: proof of principle. J Pathol Clin Res 7: 432-437.
- Valstar MH, Andreasen S, Bhairosing PA, McGurk M (2020) Natural history of recurrent pleomorphic adenoma: implications on management. Head Neck 42: 2058-2066.
- de Ridder M, Balm AJM, Smeele LE, et al. (2015) An epidemiological evaluation of salivary gland cancer in the Netherlands (1989-2010). Cancer Epidemiol 39: 14-20.
- Ihrler S, Guntinas-Lichius O, Agaimy A, Wolf A, Mollenhauer M (2017) Histological, immunohistological and molecular characteristics of intraductal precursor of carcinoma ex pleomorphic adenoma support a multistep carcinogenic process. Virchows Arch 470: 601-609.
- Stenman G (2013) Fusion oncogenes in salivary gland tumors: molecular and clinical consequences. Head Neck Pathol 7: 12-19.
- Bell D, Myers JN, Rao PH, El-Naggar AK (2012) t(3;8) as the sole chromosomal abnormality in a myoepithelial carcinoma ex pleomorphic adenoma: a putative progression event. Head Neck 35: 181-183.
- Di Palma S (2013) Carcinoma ex pleomorphic adenoma, with particular emphasis on early lesions. Head Neck Pathol 7: 68-76.
- Grünewald I, Vollbrecht C, Meinrath J, Meyer MF, Heukamp LC, et al. (2015) Targeted next generation sequencing of parotid gland cancer uncovers genetic heterogeneity. Oncotarget 6: 18224-18237.
- Andreasen S, Therkildsen MH, Bjørndal K, Homøe P (2016) Pleomorphic adenoma of the parotid gland 1985-2010: a Danish nationwide study of incidence, recurrence rate, and malignant transformation. Head Neck 38: 1364-1369.
- Antony J, Gopalan V, Smith Ra, Lam AKY (2012) Carcinoma ex pleomorphic adenoma: a comprehensive review of clinical, pathological and molecular data. Head Neck Pathol 6 :1-9.
Citation: Khasanov AI, Nishonboyev LS, Primkulov BK, Karimov OM, Khasanov AI, et al. (2022) Surgical Treatment of Malignant Transformation Tumors of the Parotid Salivary Gland of the Large Size from 30 Years Ago. J Otolaryng Head Neck Surg 8: 73
Copyright: © 2022 Akbar I. Khasanov, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

