Survival Following Endovascular Aneurysm Repair in the Octogenarian
*Corresponding Author(s):
Dominic PangDepartment Of Vascular Surgery, Ward 507, Aberdeen Royal Infirmary, Aberdeen Scotland, Ab252zn , United Kingdom
Tel:+07540372780,
Email:Dominic.Pang@Nhs.Net
Abstract
Survival following elective Endovascular Aneurysm Repair (EVAR) in the Octogenarian
Aim: Increasing age is a recognized independent predictor of mortality in aneurysm surgery. However, the long term survival benefit in octogenarians following Endovascular Aneurysm Repair (EVAR) remains unclear despite supporting evidence of safe use.
Methods: Consecutive subjects who underwent elective EVAR for AAA in a single tertiary centre between 1st July 2000 and 31st January 2015 were identified and survival data extracted through hospital electronic records. Subjects were categorized into two cohorts based on age, Group 1 (G1): < 80 years and Group 2 (G2): ≥80 years. Primary endpoints of interest were (i) 30-day mortality; (ii) early and late aneurysm related deaths; (iii) overall survival at follow up at 31 March 2015.
Results: 266 patients (235 male, 88.3%) were included in the study. G1 comprised 195 patients (180 male, 92.0%), mean age 71.9 years (Standard Deviation (SD) 5.7) whilst G2 comprised 71 patients (55 male, 77%), mean age 83.2 years (SD 2.1).The mean AAA sac diameter were similar between groups (6.5cm v 6.3cm, p > 0.05). G2 had higher proportion of patients with chronic kidney disease (32% v 12%, p < 0.001). Thirty-day mortality: 3 deaths occurred in G1 and 1 in G2. The odds ratio for octogenarians developing post-operative 30-day complications was 1.99 (95% confidence interval (CI) 1.11- 3.61, p = 0.02).
At follow up, 81 deaths occurred (G1: 55, G2: 26). Overall median survival was 91 months (Standard Error (SE) 4.6). Median survival in G1 = 92 (SE 16.6) months and G2 = 87 (SE 14.8) months. No survival differences were observed between groups on Kaplan Meier analysis (Log Rank, p > 0.05). Multivariate Cox proportional hazards model demonstrated that ASA scores more than 3 significantly predicted risk of mortality during follow up with hazard ratio of 3.97 (95% confidence interval 2.06 - 7.65).
Conclusion: Survival of selected octogenarian patients undergoing elective EVAR is comparable to younger co-hort of patients undergoing EVAR.
Keywords
INTRODUCTION
Abdominal Aortic Aneurysms (AAA) is generally a disease of the ageing population where its prevalence increases significantly with age [2]. Increasingly as the nation ages, the demands on vascular services to provide treatment for non-rupture AAA in octogenarians too rises. This poses a clinical dilemma to clinicians. On one hand, we rec-ognize increasing age as an independent predictor of mortality, postoperative complications, and the need for dis-charge to an extended care facility for both treatment options of AAA, open and Endovascular Aneurysm Repair (EVAR) not to mention the limited potential in remaining life years [3,4]. On the other hand, current evidences through randomized controlled trials do suggest safe EVAR use in octogenarians [5-8]. Although some controver-sies do remain regarding the generalisability of these evidences, this is enough to cause split opinions amongst field experts. Now, there are also epidemiological evidences which suggest a shift in incidence of AAA towards those over 75 years of age towards non-rupture [9]. With the uncertainty in choice of management in non-ruptured AAA in this cohort of patients, what remains certain is that understanding the potential gain in life years in these selected older patients post EVAR will guide future management pathways. We performed this study to evaluate the out-come of EVAR in the selected octogenarian patients in the north of Scotland.
METHODS
For these patients, data including patient demographics, aneurysm morphology, post-operative morbidity, mortality and late mortality, and re-intervention were retrieved from hospital electronic records. Where available on hospital records, the cause of death was recorded for deceased subjects to assess whether death was directly related to aneurysm disease. Those where cause of death was unavailable were defaulted to have deaths unrelated to aneurismal disease.
Primary endpoints of interest were (i) 30-day mortality; (ii) early and late aneurysm related deaths; (iii) overall survival at follow up censored at 31 March 2015. Secondary endpoints identified include 30-days postoperative morbidity and the rate for re-intervention. Postoperative morbidity in this study included graft-related complication, myocardial infarction, respiratory tract infection, acute kidney injury and ischemic complications.
For statistical analysis, SPSS version 22 was used. Student’s T test was used to analyze categorical variables. Chi square test was used to analyze difference between proportions. Kaplan-Meier method was used to analyze survival differences and cox proportional hazard ratios were used to analyze pre-operative covariates significantly affecting long-term survival. P value of < 0.05 was considered statistically significant.
RESULTS
Patient demographics
The mean AAA sac diameter were similar between both groups (6.5cm v 6.3cm, p > 0.05), as proportion of pa-tients with ASA greater than 3 (4% v 7%, p >0.05) (Table 1).
| Variable | Group 1 (n = 195) | Group 2 (n = 71) | p value |
| Males (%) | 180 (92%) | 55 (77%) | 0.001 |
| Mean age (SD) | 71.9 (5.7) | 83.2 (2.1) | - |
| ASA*>3 (%) | 14 (7%) | 3 (4%) | NS |
| Preoperative CKD** | 24 (12%) | 23 (32%) | <0.001 |
| Mean AAA Sac Diameter (SD), cm | 6.3 (1.0) | 6.5 (1.1) | NS |
**CKD - Chronic Kidney Disease, patients with eGFR of < 60 ml/min/1.73 m2
Intra-operative details
| Group 1 | Group 2 | p value | |
| General anesthesia (%) | 158 (81%) | 54 (76%) | NS |
| Operative time (SD), min | 141 (48) | 150 (51) | NS |
Perioperative (30-days) mortality and morbidity
| Variable | Group 1 (n = 195) | Group 2 (n = 71) | p value |
| Median postoperative stay (IQR), days | 3 (2 - 4) | 4 (2 - 6) | <0.001 |
| Graft complications (%) | 6 (3.1%) | 3 (4.2%) | NS |
| Myocardial Infarction (%) | 2 (1%) | 3 (4.2%) | NS |
| Respiratory tract complications (%) | 7 (3.6%) | 8 (11.2%) | 0.02 |
| Acute kidney injury (%) | 15 (7.6%) | 10 (14.1%) | 0.09 |
| Ischaemic complications (%) | 1 (0.5%) | 0 (0%) | NS |
| Missing data (%) | 2 (1%) | 0 (0%) | NS |
| Total morbidity (%) | 33 (16.9%) | 24 (33.8%) | <0.001 |
Late follow up and survival analysis
| Group 1 | Group 2 | p value | |
| Embolisation | 9 | 3 | - |
| Extension | 4 | 1 | - |
| ReEVAR | 2 | 0 | - |
| Total reintervened (%) | 15 (7%) | 4 (6%) | NS |
| Multiple reinterventions | 9 | 4 | - |
For the entire cohort, median Survival (SE) was 89 months (12.3) with survival in G1: 92 (16.6) months and G2: 87 (14.8) months. Early and late survival analysis using Kaplan Meier method did not demonstrate any significant survival difference between the groups (Log Rank, p > 0.05) (Figure 1). One patient died of an aneurysm-related complication at 60 months due to a peri-aortic graft infection (Table 5).
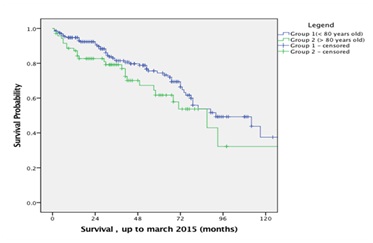
Group 1 178 163 152 143 141
Group 2 59 53 48 46 46
| Variables | Group 1 | Group 2 | p value |
| 30 day mortality | 3 | 1 | NS |
| Non-aneurysm related deaths at follow up | 51 | 25 | NS |
| Aneurysm related deaths at follow up | 1 | 0 | NS |
| Total deaths | 55 | 26 | NS |
| Hazard ratios | 95% confidence interval | |
| Age > 80 years old | 1.50 | 0.92 - 2.45 |
| ASA score > 3 | 3.98 | 2.06 - 7.65 |
| Chronic Kidney Disease | 1.06 | 0.58 - 1.93 |
| Re-intervention | 3.60 | 0.88 - 14.74 |
DISCUSSION
In the UK, national screening program implemented offer routine AAA screening to men aged 65 years, where the disease is recognized to be most prevalent and screening most cost effective. In contrast, AAA in females of this age cohort is rare and therefore, found to not cost effective for a national screening programmed. Building on this, one observation noted in our study is the higher proportion of female within the octogenarian group. This shares the observation of others in the literature [10,11]. At a superficial level, this may simply represent an upward trend of AAA in female octogenarians. However, given the obvious absence of AAA screening in females, this is more likely to be a representation of a major selection bias in the population as a result of a male only national AAA screening programmed. Certainly, further epidemiological studies may be required to demonstrate this causal rela-tionship.
Whilst there was no clear survival advantage observed in the octogenarian population, they had a significantly higher rate of developing postoperative complications than younger patients. This is in keeping with the findings reported in previous series and is considered to reflect the general level of co-morbidities and reduced physiological reserve [3,4]. Postoperative renal dysfunction is a significant complication following EVAR and represents the most common post-operative complication in patients under and over 80 years of age (8.4% vs 14.6%) [13,14]. These figures are higher than currently reported in the literature which may be due to underreporting in the litera-ture and a lack of a standardized definition on the subject [14-16]. However, these complications did not translate into a higher 30-day mortality rate in octogenarian patients. Post-operative length of hospital stay amongst octogenarians was significantly longer than in the younger population, and is considered to be the result of both an increased rate of complications and also social circumstances.
In this study, we report comparable post EVAR survival rates in selected octogenarian patients to younger patient cohorts. It is important to highlight that the octogenarians included in the study (mean age (SD): 83 (2.1) years) were significantly older than the EVAR trial 2 participants. Octogenarian patients, representing 27% of our total EVAR cohort, were considered surgically fit following careful anaesthetic evaluation. This included routine blood tests, pulmonary function tests, electrocardiogram and/or myocardial perfusion scans followed by a consultant anaesthetist assessment. Further investigations or pre-operative interventions were carried out as necessary. Fifty-eight percent of our octogenarian population survived beyond 5 years, which compares favourably with general life expectancy amongst the population in our region although it is notably less than the 64 - 92% 5-year survival reported in other studies (3,4,11,12).
Another important aspect of EVAR is the necessity for continual post procedural lifelong surveillance and the possible need for re-intervention. For octogenarians whose lifespan is limited, survival free of intervention is of greater significance. This is challenging to achieve given poorer AAA anatomical suitability for EVAR in octogenarians to begin with [17]. In our study, we did not observe any difference of rate of re-intervention for endoleaks between both groups. Where quality of life post EVAR is concern, this represents an encouraging observation for octogenarians, where further re-interventions add on to the risk of morbidity. However, we also aware that this may be a representation of selection bias in our study, mainly due to the patient selection process for initial EVAR procedure.
We acknowledge that our study includes a carefully selected group of octogenarian subjects evaluated in a struc-tured preoperative process that evolved over time without data available for those declined treatment. This is be-cause no formal register was kept for patients declined of treatment. Despite this, we believe that our study is gene-ralisable to other UK or European centers where patient sélection processes are similar. Our experience continues to support a structured multidisciplinary team approach in the selection of octogenarians to proceed to EVAR for AAA. We strongly support the statement from AAA patient groups in the UK that chronological age should not be the only factor affecting decision to treat [18].
CONCLUSION
CONGRESS
CONFLICT OF INTEREST
ACKNOWLEDGEMENT
REFERENCES
- Office for National Statistics (2012) Population Ageing in the United Kingdom, its Constituent Countries and the European Union. Office for National Statistics, UK.
- Savji N, Rockman CB, Skolnick AH, Guo Y, Adelman MA, et al. (2013) Association between advanced age and vascular disease in different arterial territories: a population database of over 3.6 million subjects. J Am Coll Car-diol 61: 1736-1743.
- Giles KA, Schermerhorn ML, O'Malley AJ, Cotterill P, Jhaveri A, et al. (2009) Risk prediction for perioperative mortality of endovascular vs open repair of abdominal aortic aneurysms using the Medicare population. J Vasc Surg 50: 256-262.
- Park BD, Azefor NM, Huang CC, Ricotta JJ (2014) Elective endovascular aneurysm repair in the elderly: trends and outcomes from the Nationwide Inpatient Sample. Ann Vasc Surg 28: 798-807.
- Hay N, McCracken F, Richardson J, George E, Barnett D (2009) Endovascular stent-grafts for the treatment of abdominal aortic aneurysms: NICE technology appraisal guidance. Heart 95: 1798-1800.
- Greenhalgh RM, Brown LC, Kwong GP, Powell JT, Thompson SG, et al. (2004) Comparison of endovascular aneurysm repair with open repair in patients with abdominal aortic aneurysm (EVAR trial 1), 30-day operative mortality results: randomised controlled trial. Lancet 364: 843-848.
- De Bruin JL, Baas AF, Buth J, Prinssen M, Verhoeven EL, et al. (2010) Long-term outcome of open or endovas-cular repair of abdominal aortic aneurysm. N Engl J Med 362: 1881-1889.
- Lederle FA, Freischlag JA, Kyriakides TC, Padberg FT Jr, Matsumura JS, et al. (2009) Outcomes following en-dovascular vs open repair of abdominal aortic aneurysm: a randomized trial. JAMA 302: 1535-1542.
- Choke E, Vijaynagar B, Thompson J, Nasim A, Bown MJ, et al. (2012) Changing epidemiology of abdominal aortic aneurysms in England and Wales: older and more benign? Circulation 125: 1617-1625.
- Fonseca R, Rockman C, Pitti A, Cayne N, Maldonado TS, et al. (2010) Intermediate-term EVAR outcomes in octogenarians. J Vasc Surg 52: 556-560.
- Prenner SB, Turnbull IC, Malik R, Salloum A, Ellozy SH, et al. (2010) Outcome of elective endovascular ab-dominal aortic aneurysm repair in octogenarians and nonagenarians. J Vasc Surg 51: 1354-1359.
- National Records of Scotland (2014). Life Expectancy for Areas within Scotland 2011-2013. Including revised estimates for 2001-2003 to 2008-2010 for Community Health Partnerships, by Urban Rural and Scottish Index of Multiple Deprivation. National Statistics, Scotland.
- Zarins CK, White RA, Schwarten D, Kinney E, Diethrich EB, Hodgson KJ, et al. (1999) AneuRx stent graft versus open surgical repair of abdominal aortic aneurysms: multicenter prospective clinical trial. J Vasc Surg 29: 292-305
- Blum U, Voshage G, Lammer J, Beyersdorf F, Töllner D, et al. (1997) Endoluminal stent-grafts for infrarenal abdominal aortic aneurysms. N Engl J Med 336: 13-20.
- Brinkman WT, Terramani TT, Najibi S, Weiss VJ, Salam AA, et al. (2004) Endovascular abdominal aortic aneurysm repair in the octogenarian. Ann Vasc Surg 18: 401-407.
- Karthikesalingam A, Bahia SS, Patel SR, Azhar B, Jackson D, et al. (2015) A systematic review and meta-analysis indicates underreporting of renal dysfunction following endovascular aneurysm repair. Kidney Int 87: 442-451.
- Pol RA, Zeebregts C, van Sterkenburg SM, Reijnen MM, Ferreira LM, (2014) Outcome and quality of life after endovascular abdominal aortic aneurysm repair in octogenarians. J Vasc Surg 60: 308-317.
- Wyatt MG (2011) National Abdominal Aortic Aneurysm Quality Improvement Programme (AAAQIP) Interim Report 2011. Abdominal Aortic Aneurysm Quality Improvement Programme, Abdominal Aortic Aneurysm Quali-ty Improvement Programme Staff, Vascular Society of Great Britain & Ireland, Vascular Society of Great Britain & Ireland Staff, Health Foundation (Great Britain), Health Foundation (Great Britain) Staff.
Citation: Pang D, Hildebrand D, Bachoo P (2017) Survival Following Endovascular Aneurysm Repair in the Octogenarian. J Angiol Vasc Surg 2: 007.
Copyright: © 2017 Dominic Pang, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.