Takotsubo Cardiomyopathy: A Recognizable Phenotype: Mid-Cavity Variant
*Corresponding Author(s):
Timothy E PaterickDepartment Of Cardiology, Bay Care Clinic Green Bay, Wisconsin, United States
Tel:+1 9044764233,
Email:tpaterick@gmail.com
Abstract
Takotsubo cardiomyopathy is an important differential consideration when a patient presents with an acute coronary syndrome. Patients typically present with chest pain/pressure, shortness of breath, electrocardiographic changes, elevated biomarkers, normal or near normal coronary arteries, and wall motion abnormalities that are not consistent with a single coronary vascular bed. This constellation of findings is often associated with a precipitating emotional or physical stressor.
Variants of the classic left ventricular apical ballooning syndrome, including mid- and basal left ventricular wall motion abnormalities, are being more frequently recognized. The recognition and diagnosis of takotsubo cardiomyopathy has important implications for clinical management initially and in follow up. A small subset of patients may experience life-threatening complication during initial presentation, however, most patient recover and have a favorable long-term prognosis. The pathophysiology of takotsubo cardiomyopathy remains an enigma, but a surfeit of catecholamines seems pertinent to the underlying pathophysiology.
Keywords
Acute and long-term treatment; Acute coronary syndrome; Angiography; Electrocardiography; Mid-ventricular variant of takotsubo cardiomyopathy; Takotsubo cardiomyopathy phenotypes.
INTRODUCTION
Takotsubo Cardiomyopathy (TC) is a unique cardiomyopathy that is an important etiologic consideration in the differential diagnosis of acute coronary syndrome. The presenting symptoms and signs are similar to acute coronary syndrome after plaque rupture, but important distinctions include absence of coronary occlusion and wall motion abnormalities that do fit with a single vascular territory. TC usually has an emotional or physical stressor. The acute presentation of TC can include life-threatening hemodynamic compromise, but the long-term prognosis is better than the prognosis associated with acute coronary syndrome [1]. There are several morphological variants of TC that include apical segment, mid-ventricular, and basal involvement. Apical and mid segment involvement may occur together. Echocardiography is fundamental to identifying the various phenotypes of TC. The mid-ventricular variant of TC is characterized by transient hypokinesis, akinesis or dyskinesis of the left ventricular mid segments with normal to hyperkinesia of apical and basal segments. There is no acute plaque rupture. There are new electrocardiographic changes including: ST elevation and/or t wave inversion and modest elevation of cardiac biomarkers [2].
CASE REPORT
59 year-old female presents with chest tightness and dyspnea. Symptoms occurred after a stressful conversation about the custody of her disabled 37-year-old son. On arrival to the emergency room she had an immediate ECG revealing t wave inversion V1-6 (Figure 1). This was compared to a normal ECG one year earlier (Figure 2).
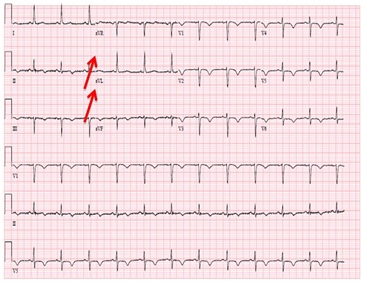
Figure 1: ECG revealing t wave inversion across the pericardium (Red arrows pointing to inverted t waves).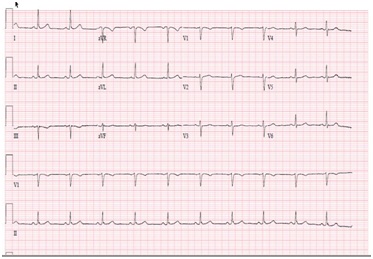
Figure 2: Normal ECG one year before when the patient was free of symptoms.
The initial troponin was elevated at 0.13ng/ml (< 0.05ng/ml). The patient was taken to the cardiac catheterization and found to have mild coronary artery disease manifest has a proximal 40% left anterior descending narrowing (Figure 3).
Figure 3: 40% LAD narrowing (red arrow pointing to the LAD lesion).
Contrast LV ventriculography did not reveal any segmental abnormalities (Figure 4). Post cardiac catheterization echocardiography revealed reduced Left Ventricular (LV) systolic function with mid LV cavity segment hypokinesis with normal thickening of the apical and basal segments (Figure 5). The troponin level peaked at 0.38ng/ml (< 0.05ng/ml). The patient recovered in the hospital without hemodynamic or electrical disturbance.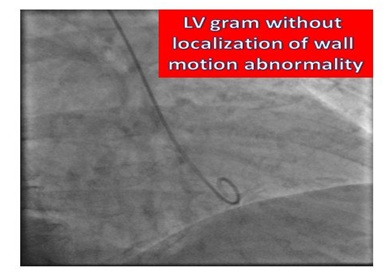
Figure 4: LV Gram: RAO.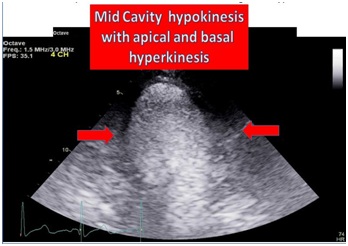
Figure 5: Modified apical 4 chambers: Mid-ventricular segment hypokinesis.
The patient returned 6 weeks later and she was free of symptoms with robust activities. Echocardiography revealed normal LV systolic function with normal wall motion of all segments (Figure 6). A nuclear stress test revealed normal perfusion. The patient had all the classic features of mid-cavity variant of TS cardiomyopathy.
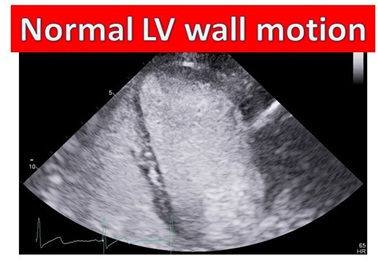
Figure 6: Modified apical 4 chamber: Recovery of LV function 6 weeks post acute presentation.
CLASSIC FEATURES OF TAKOTSUBO CARDIOMYOPATHY
Presentation
Prevalence
Typically apical or mid-ventricular segment akinesia of the left ventricle (or both) is present. Also, not common is isolated mid-ventricular segment akinesia with apical sparing (Our case). It has been reported that as many as 40% of the TC cases are the mid-ventricular variant [4]. Basal akinesia with mid cavity and apical sparing has been identified [5]. There is no evidence identifying different pathophysiologic mechanisms for the phenotypic variant of TC.
Electrocardiography and coronary angiography
Cardiac biomarkers
TREATMENT: ACUTE, SUB-ACUTE AND LONG-TERM
Acute treatment
Sub-acute and long-term treatment
CONCLUSION
Mid-ventricular variant of takotsubo cardiomyopathy is a recognizable phenotype that requires a high index of clinical suspicion and meticulous echocardiographic imaging. Echocardiography is the imaging modality of choice to clearly delineate the mid cavity hypokinesis.
REFERENCES
- Sharkey SW, Lesser JR, Zenovich AG, Maron MS, Lindberg J, et al. (2005) Acute and reversible cardiomyopathy provoked by stress in women from the United States. Circulation 111: 472-479.
- Prasad A, Lerman A, Rihal CS (2008) Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): A mimic of acute myocardial infarction. Am Heart J 155: 408-417.
- Roseberry BJ, Paterick TE (2009) Takotsubo cardiomyopathy resulting in left ventricle thrombus. Cardiology Review 26: 45-47.
- Kurowski V, Kaiser A, von Hof K, Killerman DP, Mayer B, et al. (2007) Apical and midventricular transient left ventricular dysfunction syndrome (tako-tsubo cardiomyopathy): Frequency, mechanisms, and prognosis. Chest 132: 809-816.
- Reuss CS, Lester SJ, Hurst RT, Askew JW, Nagor P, et al. (2007) Isolated left ventricular basal ballooning phenotype of transient cardiomyopathy in young women. Am J Cardiol 99: 1451-1453.
- Wittenstein IS, Thiemann DR, Lima JAC, Baughman KL, Schulman SP, et al. (2005) Neurohumoral features of myocardial stunning due to sudden emotional stress. The New England Journal of Medicine 352: 539-548.
- Yoshioka T, Hashimoto A, Tsuchihashi K, Nagao K, Kyuma M, et al. (2008) Clinical implications of midventricular obstruction and intravenous propranolol use in transient left ventricular apical ballooning (Tako-tsubo cardiomyopathy). Am Heart J 155: 526.
- Akashi YJ, Tejima T, Sakurada H, Matsuda H, Suzuki K, et al. (2004) Left ventricular rupture associated with Takotsubo cardiomyopathy. Mayo Clin Proc 79: 821-824.
- Raddino R, Pedrinazzi C, Zanini G, Robba D, Portera C, et al. (2008) Out-of-hospital cardiac arrest caused by transient left ventricular apical ballooning syndrome. Int J Cardiol 128: 31-33.
- Bybee KA, Prasad A, Barsness GW, Lerman A, Jaffe AS, et al. (2004) Clinical characteristics and thrombolysis in myocardial infarction frame counts in women with transient left ventricular apical ballooning syndrome. Am J Cardiol 94: 343-346.
Citation: Patel NJ, Paterick TE (2018) Takotsubo Cardiomyopathy: A Recognizable Phenotype: Mid-Cavity Variant. J Cardiol Stud Res 4: 013.
Copyright: © 2018 Nachiket J Patel, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.