
Telemedicine Satisfaction in Pregnant Women during the Covid-19 Pandemic
*Corresponding Author(s):
Eliana L GarciaUniversity Of New Mexico School Of Medicine, 915 Camino De Salud NE Albuquerque, NM 87106, United States
Tel:+1 5753024510,
Email:elianag@salud.unm.edu
Abstract
Objective: SARS-CoV-2 has drastically changed the way providers deliver care to obstetric patients. The aim of our study is to understand how telemedicine care has affected patient satisfaction and overall patient experiences.
Study design: Participants were recruited during a maternal-fetal medicine ultrasound appointment. A patient satisfaction and demographic survey were delivered either in person after their appointment via telephone interviews. The responses were graded on a 5-point Likert scale.
Results: The study population consisted of 152 adult women, of which 72% were Native American and 23% Hispanic. Half (50.68%) of the participants lived in rural areas. For the statement: “Overall, I am satisfied with the quality of service being provided via telemedicine,” 95% agreed or strongly agreed. In response to the statement: “I feel I could safely talk about my physical and emotional problems during my visit,” 92% of patients agreed or strongly agreed. When considering receiving telemedicine care in the future, 72% agreed or strongly agreed.
Conclusion: Telemedicine provides high satisfaction and a valuable patient experience in high-risk obstetric patients in rural and urban underserved areas. Future studies should investigate clinical outcomes with telehealth as well as limitations of the large-scale use of telemedicine and the quality of service it provides.
Keywords
COVID-19; Indigenous/ rural health; Obstetrics; Quality improvement; Telemedicine
Introduction
Pregnancy is a significant time in a woman's life. Generally, prenatal care has been given in-person, and weekly or semi-weekly appointments may be indicated. Obstetrical care through telemedicine was very uncommon before the COVID-19 pandemic. Routine obstetrical care is usually “bundled” - meaning that the number of patient visits does not impact the cost. Most providers schedule patient visits at prescribed intervals, with additional visits as clinically indicated according to the level of patient complexity. Pregnant patients generally receive a physical examination, blood pressure check, and urine-dip testing at each encounter to monitor for preeclampsia and other possible complications. Additionally, pregnant women require frequent laboratory testing to monitor common problems such as anemia, infections, and diabetes.
Pregnant women became an extremely vulnerable group during the SARS-CoV-2 Pandemic of 2019-20. Pregnant women diagnosed with COVID-19 are more likely to suffer from complications such as preterm delivery and are at a higher risk of maternal death than pregnant women without COVID-19 [1-3]. Additionally, many patients not presenting as obstetrically high risk experienced a reduction in antenatal care visits from an average of 10-15, down to six [4]. As the risk of COVID-19 exposure increased, the number of in-person visits to our health system was decreased to minimize exposures and travel for both patients and staff. Consequently, the Maternal-Fetal Medicine (MFM) division at our institution transitioned to “seeing” outreach patients who live one to five hours from the hospital via virtual video calls for the first time. However, patients were still required to come to a local community hospital or clinic where they received their obstetric ultrasound followed by a telemedicine visit with a physician.
Of particular importance, the New Mexico obstetrical population includes Indigenous and Hispanic women, many of whom are not English speakers [1]. These women commonly face even greater challenges to receiving care due to their race and cultural identity [5-7]. In addition, communication challenges between provider and patient, barriers to transportation, and low socioeconomic status may interfere with optimal care [8,9]. New Mexico also has a large rural population, and patients living in these areas may face barriers to accessing medical care and transportation. These additional factors only exacerbated the difficulty in providing care during the pandemic. Currently, the impact of telemedicine on underserved patients such as the women described above is unclear and warrants further investigation. At the same time, the implementation of telemedicine for prenatal care has become more ubiquitous. Widespread acceptance may be due to increasing comfort and familiarity with this modality both among patients and providers.
Many issues related to patient satisfaction with telemedicine remain unknown and warrant further review. We hypothesized that a telemedicine visit would be a safe and convenient alternative for pregnant women to attend prenatal appointments during the time of pandemic-caused uncertainty and social distancing. In addition, we anticipated that virtual obstetrical care would increase access for women who live in rural counties. Rural areas typically lack specialists, including obstetricians, which means patients must travel significant distances to receive certain types of care. A previous study of audio-only virtual visits found that many pregnant women preferred a combination of in-person and telemedicine visits. This finding was primarily attributed to decreased transportation times, cost of transportation, and less time spent away from employment and childcare [10]. However, as telemedicine rapidly emerges as a crucial form of healthcare delivery, little is known about patient satisfaction with virtual patient visits in place of regular in-office care. The decision to implement video visits in the care of pregnant women during the SARS-CoV-2 pandemic was a pragmatic one. Whether this impacted maternal and neonatal outcomes is unknown at this time. More information on patients’ opinions of telemedicine is also needed, particularly from underserved patient populations such as the Indigenous and Hispanic women living in New Mexico. The purpose of this study is to understand how providing telemedicine care during the SARS-CoV-2 pandemic influenced patient satisfaction and overall patient experience among pregnant women receiving care in New Mexico and surrounding rural areas.
Materials and Methods
This original research was approved by the local institution review board. A total of 152 high-risk English and Spanish-speaking obstetrical patients were interviewed via telephone or given a paper survey between April and December 2020. Surveys included items about satisfaction with telemedicine visits during the SARS-CoV-2 pandemic, use of technology for these visits, perceived privacy and quality of telemedicine visits, and demographics information. Telemedicine visits were defined as occurring between physician and patient via video or phone conferencing. During the telemedicine visit, physicians, midwives, and nurse practitioners identified antepartum and postpartum patients interested in participating in the study. Inclusion criteria focused on patients mainly receiving high-risk obstetric care through telemedicine after SARS-CoV-2 clinical visit restrictions were implemented. Only pregnant or postpartum women over the age of eighteen were consented to participate in the study.
Interested patients were contacted by telephone after their visit or were recruited in person once they arrived at the clinic. All consented study participants completed a two-part survey designed to take no longer than 10 minutes. The first survey addressed patient satisfaction with their most recent telemedicine visit. The second survey addressed demographics and socioeconomic status. Responses were recorded in de-identified survey forms in the secure REDCap data capture system. Patients who had at least one previous telemedicine encounter and were seen for follow-up ultrasounds at MFM outreach clinics were given the option to complete the surveys in paper form while waiting for their ultrasound. Participant responses to the survey were graded on a 5-point Likert scale.
Results
A total of 152 patients participated in the study over eight months. Of these patients, 72% (N=108) were Indigenous, 23% (N=35) were Hispanic/Latino, and 5% (N=7) were non-Hispanic white (Table 1). The mean age was 31 (SD=6), the mean household size was 4 (SD=2) and the average pregnancy number was 3 (SD=2). Based on Primary RUCA Codes, study participants' zip-code demographics were classified as 49% (N=72) urban and 51% (N=74) rural, with most patients living in northern and eastern New Mexico. The majority had an annual household income of less than $25,000 (65.9% [N=65.9]), and a significant number shared that they do not always have health insurance (39.1% [N=59]). Patients’ education levels split between some college or higher (59.6% [N=89]) and high school education or less (40.4 % [N=61]). Most (62.9% [N=95]) were unemployed, and 37.1% (N=56) were employed. For those who were employed, 53.6% (N=81) worked outside of the home, while 46.4% (N=70) worked from home.
|
Demographic |
N (%) |
Demographic |
N (%) |
|
Race/Ethnicity |
Residence |
||
|
NA/AI |
108 (72.0) |
Urban |
72 (49.3) |
|
Hispanic/Latino |
35 (23.3) |
Rural |
74 (50.7) |
|
White Non-Hispanic |
7 (4.7) |
Annual Household Income |
|
|
Education Level |
<$25,000 |
89 (65.9) |
|
|
High school or less |
61 (40.4) |
>$25,000 |
46 (34.1) |
|
Some college or more |
89 (59.6) |
Work Outside Home |
|
|
Employment status |
Yes |
81 (53.6) |
|
|
Employed |
56 (37.1) |
No |
70 (46.4) |
|
Unemployed |
95 (62.9) |
Continuous Variables |
Mean (SD) |
|
Insurance Status |
|
Age |
31 (6) |
|
Always Insured |
92 (60.9) |
Household Size |
4 (2) |
|
Not Always Insured |
59 (39.1) |
Pregnant with (#) child |
3 (2) |
Table 1: Demographic characteristics of the study population.
This table represents the patient's responses to a demographics survey.
A majority of the patient visits were conducted by video (90%). Participants responded to twelve items regarding their perceived satisfaction with their telemedicine visit (Table 2). An overwhelming majority (N=143) had a positive response towards telemedicine services provided (Figure 1). Most patients felt satisfied with the quality of service provided during the pandemic (54% [N=81] agreed, while 41% [N=62] strongly agreed). Less than 3% (N=5) disagreed that communication was clear during the visit and less than 5% (N=8) felt that technical difficulties were not satisfied. A total of 93% of patients found telemedicine to be useful and helpful during pregnancy, with 39% (N=59) strongly agreeing and 54% (N=81) agreeing. A total of 92% of patients felt that they could safely talk about their physical and emotional issues during the virtual visit, with 38% (N=58) strongly agreeing and 54% (N=82) agreeing. An overwhelming majority of patients (71% [N=108]) would consider receiving telemedicine care again in the future, a finding shared by Holcomb et al., [10]. Compared to those with an annual household income >$25,000, women with a yearly household income <$25,000 were more likely to prefer a telehealth visit over a traditional in-person visit (Figure 2).
|
Item |
Question |
|
1 |
My telemedicine visit started at the scheduled time. |
|
2 |
If any technical difficulties occurred, they were resolved to my satisfaction. |
|
3 |
Communication with my provider was clear during my visit. |
|
4 |
I consider this method of care to be adequate and safe considering the current Coronavirus pandemic. |
|
5 |
I feel comfortable using modern technology to access telemedicine care. |
|
6 |
My experience with the provider during my telemedicine visit felt personal and met my needs. |
|
7 |
My visit was private enough to discuss personal issues. |
|
8 |
I felt I could safely talk about my physical and emotional problems in my telemedicine visit. |
|
9 |
I found telemedicine to be useful and helpful during my pregnancy. |
|
10 |
I prefer a telemedicine visit over a traditional in-person visit. |
|
11 |
I would consider receiving telemedicine care in the future. |
|
12 |
Overall, I am satisfied with the quality of service being provided via telemedicine. |
Table 2: Telemedicine survey.
This table shows the 12 survey statements which were graded on a 5-point Likert scale.
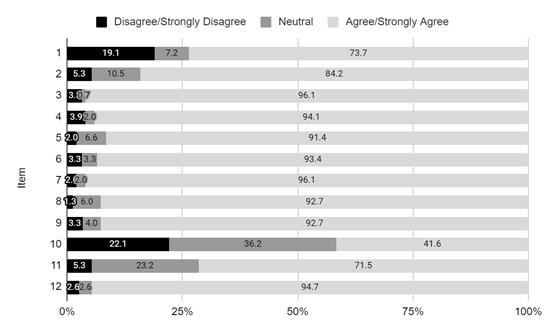 Figure 1: Patient Survey Responses on Telehealth Visits for High-risk Obstetrical Care.
Figure 1: Patient Survey Responses on Telehealth Visits for High-risk Obstetrical Care.
This figure shows the degree of satisfaction with telemedicine using the 12-item survey. See Table 2 for corresponding survey statements.
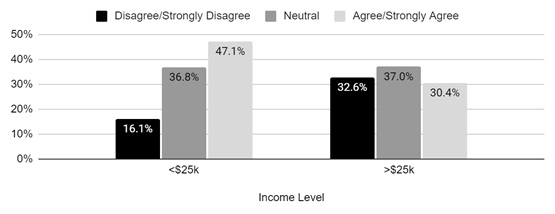 Figure 2: Economic Status and Telemedicine Preference.
Figure 2: Economic Status and Telemedicine Preference.
This figure represents the correlation between the annual income status of patients and their preferences for telemedicine visits over in-person visits. See Table 2 for statement 10.
Discussion
Study participants’ positive outlook on telemedicine and its convenience advocates for telemedicine as a viable source of healthcare and a complement to in-person care. As discussed by Leite et al., the COVID-19 pandemic has revealed the efficacy of telemedicine, especially for mothers who are concerned about the threat of the virus on their health and that of their baby [11]. Our results have shown that telemedicine has a high satisfaction rate (95%) and can help deliver quality healthcare to high-risk obstetric patients in rural and urban underserved areas and for racial and ethnic minorities. Telemedicine was acceptable to almost all patients and preferable to some patients. Our results suggest that a telemedicine visit can support a safe and comfortable environment for addressing a patient’s personal topics while maintaining privacy and security. Additionally, we found that pregnant women are very likely to consider receiving telemedicine care in the future. Women with an annual household income <$25,000 showed a preference toward telemedicine, demonstrating the importance of telemedicine in improving health equity.
Our study involved participants from an underserved population that commonly faces many challenges accessing care. Barriers such as low-income status, lack of education, and rurality make accessing health care, especially specialist care, very challenging. The demographic data supports telemedicine as beneficial and convenient for those without proper access to healthcare and those with lower household incomes. In addition, our patient interviews revealed that some women who lacked home internet services commonly used their local clinic to conduct their telemedicine visits with their specialty provider based in a distant urban setting. Many women interviewed also juggled additional childcare/family obligations and benefited from the convenience of telehealth visits. Thus, increased implementation and funding for telemedicine services in rural clinics may improve healthcare accessibility for patients, especially those without personal access to the internet and those with increased family obligations. Another benefit to telemedicine is that it allows the physician and patient to meet virtually and decide if an additional in-person visit is needed. This mode of healthcare delivery will minimize travel expenses and time. In addition, telemedicine’s convenience and cost-saving attributes could improve health provider satisfaction if patient compliance with scheduled appointments was increased.
Limitations
This study is small and involves a specific geographic region primarily populated by Indigenous and Hispanic/Latino women. Consequently, our results may not be generalizable to other rural areas in the U.S. Though our survey gives us a sense of how this group of women responded to telemedicine, their responses may reflect cultural bias. Though the surveys were anonymous, paper surveys were completed and collected at the clinical facility where the study participants received care. Patients may have been concerned that their responses were somehow linked to them and may not have been honest in their responses. Patients that were surveyed by phone were called by an investigator involved in the study. Patient’s responses may have been slanted by the desire not to offend or disappoint the person they were speaking to, resulting in more positive responses than they might otherwise have given.
The positive outlook on telemedicine and its convenience advocates for telemedicine as a viable source of healthcare. However, while our study has shown that pregnant patients are satisfied with telemedicine visits, less is known regarding patient outcomes. Follow-up studies are needed to determine the frequency of complications for patients seen via telemedicine versus patients seen at a traditional in-person visit. Additionally, our study focused on patient satisfaction with their telemedicine visit, and less is known about providers' satisfaction with using telemedicine to connect with patients. Studies that assess the logistics of use and satisfaction with telemedicine for both patients and providers are needed to optimize telemedicine. Finally, a population-based survey on interest in telemedicine in underserved regions would help assess the community’s need for these services. Protocols to provide widespread telemedicine care should be investigated and developed. In addition to evaluating patient outcomes and provider satisfaction with telemedicine, future studies should investigate the large-scale use of telemedicine and explore its limitations on the quality of service it provides.
Implications for Practice Policy
There are many implications for the use of telemedicine in future practice policy. First, there is a need to advocate for service and payment parity when utilizing prenatal telemedicine services. This would expand insured patient services and help incentivize physicians to use these services more frequently-additionally, our data advocates for greater at-home access to care for patients. Due to increased convenience and saving on transportation costs, telemedicine may facilitate patients’ participation in these services. Second, there is a need to advocate for more significant investment in infrastructure to support telemedicine, especially in rural and underserved areas. This entails expanding broadband internet access for rural areas and more significant direct funding for clinics that offer telemedicine visits. Finally, with the expansion of telemedicine, many institutions may require telemedicine training for physicians to ensure quality telemedicine and communication skills. These policy implications support telemedicine as a valuable source of outreach and health care expansion.
Conclusion
Our study shows that telemedicine can act as a compliment, and in some cases, an adequate alternative to in-person prenatal care in underserved rural and urban areas. Telemedicine can provide quality care and a valuable patient experience. Telemedicine for obstetric care is feasible in the pandemic setting and continues to gain advancements in technology. By understanding the experience and interests of our pregnant population, we can adapt our current practices to provide them with high-quality and more accessible care.
Acknowledgement
We want to thank the MFM Outreach Staff, Tim Petersen Ph.D., Martin Jurado MD, and Daniel A. Garcia for their contributions.
References
- Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, et al. (2020) Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ 370: 3320.
- Rubin R (2021) Pregnant People's Paradox-Excluded From Vaccine Trials Despite Having a Higher Risk of COVID-19 Complications. JAMA 325: 1027-1028.
- Rasmussen SA, Jamieson DJ (2021) Pregnancy, Postpartum Care, and COVID-19 Vaccination in 2021. JAMA 325: 1099-1100.
- Kotlar B, Gerson E, Petrillo S, Langer A, Tiemeier H (2021) The impact of the COVID-19 pandemic on maternal and perinatal health: A scoping review. Reprod Health 18: 10.
- Gampa V, Bernard K, Oldani MJ (2020) Racialization as a Barrier to Achieving Health Equity for Native Americans. AMA J Ethics 22: 874-881.
- Jones DS (2006) The persistence of American Indian health disparities. Am J Public Health 96: 2122-2134.
- Paz K, Massey KP (2016) Health Disparity among Latina Women: Comparison with Non-Latina Women: Supplementary Issue: Health Disparities in Women. Clin Med Insights Womens Health 9: 71-74.
- Hanson JD (2012) Understanding prenatal health care for American Indian women in a Northern Plains tribe. J Transcult Nurs 23: 29-37.
- Wille SM, Kemp KA, Greenfield BL, Walls ML (2017) Barriers to Healthcare for American Indians Experiencing Homelessness. J Soc Distress Homeless 26: 1-8.
- Holcomb D, Faucher MA, Bouzid J, Quint-Bouzid M, Nelson DB, et al. (2020) Patient Perspectives on Audio-Only Virtual Prenatal Visits Amidst the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Pandemic. Obstet Gynecol 136: 317-322.
- Leite H, Hodgkinson IR, Gruber T (2020) New development: ‘Healing at a distance’—telemedicine and COVID-19. Public Money & Management 40: 483-485.
Citation: Garcia EL, Link R, Ruckman R, Katukuri V, Izquierdo L, et al. (2022) Telemedicine Satisfaction in Pregnant Women during the Covid-19 Pandemic. J Reprod Med Gynecol Obstet 7: 095.
Copyright: © 2022 Eliana L Garcia, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

