
The Effect of Pilates and Stabilization Techniques on Pain and Function for Patients with Lumbar Radiculopathy
*Corresponding Author(s):
Julija AndrejevaRehabilitation And Aesthetic Therapy Department, Faculty Of Health Sciences, Klaipedos Valstybine Kolegija/ Higher Education Institution, Klaipeda, Lithuania
Tel:+370 65965131,
Email:ktgtkatedra@kvk.lt
Abstract
Research aim: To assess the effects of Pilates, stabilization, and conventional physiotherapy on lumbar spine pain and function.
Research methods: Participants 34-60 years old (45 ± 6.4 years) experiencing neuropathic pain in the lumbar spine and lower limb, with reduced lumbar mobility, were randomly divided into three groups. Sessions were conducted five times a week for 12 weeks. Pain was assessed using the Numeric Visual Analog Scale (VAS), Oswestry Low Back Pain Disability Questionnaire, and the Straight Leg Raise test (Lasegue test) to evaluate pain from lumbar and sacral nerve root irritation. Lumbar mobility was measured using the " fingertip-to-floor " test, and muscle strength was evaluated using the Lovett scale.
Results: Research data show that both Pilates and Stabilization exercises positively affected participants' functional conditions in lumbar spine radiculopathy (p > 0.05). When assessing lumbar spine mobility before and after exercise, significant changes were observed in all three groups (p < 0.05). Pain intensity decreased significantly in all three groups (p < 0.05).
Conclusion: The evidence supports that incorporating Pilates and core stabilization approaches into physiotherapy regimens can significantly improve pain levels, functional capacity, and spinal flexibility in patients with lumbar radiculopathy.
Keywords
Lumbar Spine; Pain; Pilates; Radiculopathy; Stabilization Exercises
Introduction
Lumbar radiculopathy is a common cause of back pain. It is characterized by pain due to compression or irritation of the nerve roots in the lumbosacral spine, accompanied by numbness and weakness [1]. There is limited evidence regarding the efficacy of rehabilitation and physiotherapy interventions for patients with lumbar radiculopathy, as most studies focus on medication and interventional pain management. Multidimensional approaches, including physiotherapy techniques, psychological support, and physical modalities, are recommended; however, optimal strategies are still under research [2]. The uniqueness of Pilates exercises lies in the fact that performing small-amplitude movements can strengthen deep muscles, reduce back pain, increase flexibility, and improve posture [3]. The application of basic Pilates exercises requires an understanding of biomechanics, exercise methods, and techniques. Pilates exercises strengthen the abdominal, back, and pelvic floor muscles, helping to prevent back pain [3]. Stabilization exercises for the spine develop core muscle function and increase the accuracy of sensory integration. Poor muscle coordination and improper muscle recruitment methods can decrease spinal stability [4]. The main goals of physiotherapy are to improve function and prevent the progression of disability. Therapeutic exercises reduce pain intensity, improve muscle strength, and enhance quality of life [5].
Patients and Methods
Participants were 34 - 60 years old (45 ± 6.4 years) and experienced neuropathic pain in the lumbar spine and lower limbs, as well as reduced lumbar spine mobility. The inclusion criteria were as follows: diagnosis of lumbar radiculopathy and verbal consent to participate in the study. The exclusion criteria were previous surgery and refusal to participate in the study.
- Research Instruments
Digital Visual Analog Scale (VAS) [6]: The respondents selected an integer from 0 to 10 that best described their level of pain. An 11-point numeric scale from 0 (indicating the least amount of pain, e.g., "no pain") to 10 (indicating the greatest amount of pain) [7].
The Oswestry Low Back Pain Disability Questionnaire [8]: consists of 10 questions on different topics: pain intensity, lifting, ability to care for oneself, walking, sitting, sexual function, standing, social life, sleep quality, and ability to travel. For each topic, six statements are provided describing possible patient life situations, from which the patient selects the most appropriate statement [7]. Each question is scored from 0–5, with a maximum score of 50. The total score was converted to a percentage by multiplying it by two [9]. Scores are categorized according to the severity of dysfunction: 0-20 – minimal, 21-40 – moderate, 41-60 – severe, 61-80 – disability, 81-100 – the patient is either bed-bound or exaggerating symptoms.
Straight leg raise test (Lasegue test): The aim was to identify pain caused by irritation of the lumbar and sacral nerve roots [10]. The patient lies on their back, and the physiotherapist holds the leg by the heel and lifts it until resistance is met, or the patient reports pain. The test was considered positive when pain was felt at an angle of 30-70°, radiating along the nerve. If pain is felt only in the lumbar region, it may indicate muscle tension. This test is used to diagnose nerve root lesions, most commonly at the L5 or S1 level.
Assessment of lumbar flexibility is performed using the “Fingertip-to-Floor” test [11]: The patient stands with straight legs and bends forward, attempting to touch their toe. The distance was measured from the tip of the middle finger to the floor. Owing to its high reliability, this test is often used in clinical practice [12].
Manual muscle strength assessment [13]: Muscle strength was assessed to determine the affected nerve root based on myotomal movements, which are the activities of muscles that receive signals from specific nerve roots. Flexion and extension of the foot and flexion of the big toe were evaluated in both legs. The assessment included myotomal movements: L4 – foot flexion, L5 – big toe flexion, and S1 – foot extension. The physiotherapist asks the patient to perform these movements and evaluates for weakness or inability to perform them. Weakness or inability to perform a movement may indicate nerve root damage; inability to flex the foot indicates L4 root involvement, whereas inability to extend the foot indicates S1 root involvement. This assessment is used to diagnose lumbar radiculopathy and helps identify the affected disc and the potential causes of pain.
- Research Design
The study was conducted between February 3, 2025, and April 25, 2025. Thirty individuals participated in the study, including 15 women and 15 men, all of whom experienced lower back pain. The participants' psychological condition was adequate, and they were working, mature age—women aged 34-55 and men aged 36-60. Participants were randomly divided into three groups. The first group (Group 1) performed Pilates exercises, the second group (Group 2) performed stabilization exercises, and the third group (Group 3) followed a conventional physiotherapy exercise program without additional equipment, with exercises performed using their own body weight. Physiotherapy sessions were administered to the study participants five times per week for 30 min each. The physiotherapy sessions lasted 12 weeks. All therapeutic technique exercises were performed on a fitness mat from various body positions according to the established physical exercise program and technique. Yoga asanas: Cat-Cow Pose (Marjaryasana-Bitilasana); Child’s Pose (Balasana); Sphinx Pose (Salamba Bhujangasana); Supine Twist (Supta Matsyendrasana); Legs-Up-the-Wall Pose (Viparita Karani); Bridge Pose (Setu Bandhasana); Cobra Pose (Bhujangasana); Half Lord of the Fishes Pose (Ardha Matsyendrasana); Reclined Pigeon Pose (Supta Kapotasana); Anuloma Viloma (Alternate Nostril Breathing) [14]. Diaphragmatic breathing and maintenance of a neutral position were emphasized for all groups. The participants were taught to stabilize their spines and feel in control of them. It is very important to maintain a neutral lumbar spine (to avoid increased lordosis) and learn how to activate and relax the abdominal muscles. Pelvic control during static and dynamic movements has received considerable attention. For each exercise, efforts were made to maintain balance as well as possible and perform the spine stabilization exercises as correctly as possible. In the introductory part, participants performed a general body warm-up (in both static and dynamic positions); in the main part, stabilization strength exercises were performed (maintaining static positions) for 10-15 minutes; and at the end, relaxation exercises were performed. The exercises were performed to strengthen the abdominal, back, and lateral trunk muscles (left and right sides). Muscle endurance is important. In the final part, participants performed light breathing and body relaxation. Assessments were performed before and on the last day of the study. Before testing, the patients agreed to participate in the study. On the first day of the physiotherapy sessions, the participants were acquainted with the aims and course of the study. Three different exercise programs were created for each group and randomly assigned to each group.
- Statistical Analysis
The three groups were compared to assess the effectiveness of the different methods, and the research data were processed using Microsoft Office Excel 16. The software was used to calculate the arithmetic means, rates, standard deviations and mean errors. The statistical data reliability was evaluated using Student’s T criterion (where p > 0.05 indicates that the difference is statistically insignificant and p < 0.05 indicates that the difference is statistically significant).
- Ethical Considerations
The study was approved by Ethics Committee in September 9th 2024, No SSV5-13 and conducted in accordance with the All European Academies [ALLEA] 2017 and the Declaration of Helsinki. Thirty female and male participants who provided informed consent were included in the study, and their confidentiality was ensured. Assessments were conducted at the beginning of the study and after the research intervention in a safe and comfortable environment. Before signing the consent forms, all participants received an information letter concerning the study, the voluntariness of participation, confidentiality, and the right to withdraw from the study at any time. The personal information of the participants was not disclosed to protect their privacy of the participants. The principle of the right to accurate information means that participation in the study does not pose any risk to participants’ personal information. Permissions to use the instruments were obtained from copyright holders.
Results
Lumbar spine flexibility was assessed by “Fingertip-to-Floor” test [11]: After conducting tests on the participants to assess lumbar spine mobility before and after the exercise program, significant changes were observed in all three groups. This table presents the average measured fingertip-to-floor distance indicators, reflecting the level of lumbar flexibility before and after the intervention. In the Pilates group, the average distance before applying the exercise program was 9.6 ±3.03 cm, and after the intervention, it was 8 ±2.75 cm, indicating an improvement. In the stabilization group, the average before the exercises was 10.1 ±2.88 cm, and after implementing the methods, the average decreased to 8.4 ±2.76 cm. In the third control group, the average before the study was 10.3 ±3.86 cm, and after the study, it decreased to 8.3 ±3.80 cm (Figure 1).
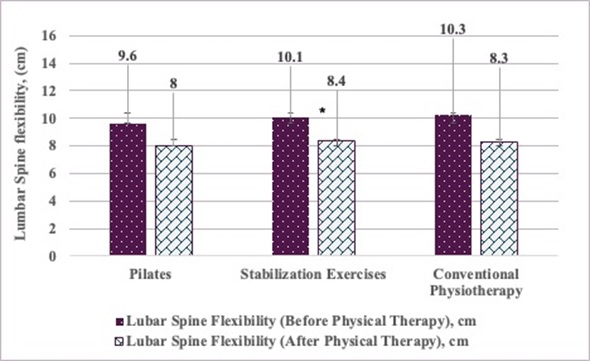 Figure 1: Lumar Spine Flexibility comparition between the groups.
Figure 1: Lumar Spine Flexibility comparition between the groups.
Statistical significance (p ≤ 0.05). Values are presented as arithmetic means ( x ) ± standard error of the mean ( Sx ).
Pain intensity was assessed using a digital visual analog scale (VAS) [6,7]: This table presents the average pain intensity assessment results before and after the intervention using different exercise methods. The first group applied the Pilates method, the second group performed stabilization exercises, and the third group (control group) received physiotherapy. The subjects in the Pilates group had an average pain score of 7.1 ±0.99 before the intervention, and after the sessions, with a repeated assessment, the pain intensity decreased to 4.5 ±1.08 points—a difference of 2.6 points. The subjects in the stabilization group had an average pain score of 7.2 ±1.03 before performing the exercises, which decreased to 5.1 ±0.88 after the exercises, amounting to a change of 2.1 points. The control group subjects had an average pain score of 7.4 ±1.26 before the application of physiotherapy methods, and afterthe treatment, the intensity decreased to 5 ±1.15 points, amounting to a difference of 2.4 points (Figure 2).
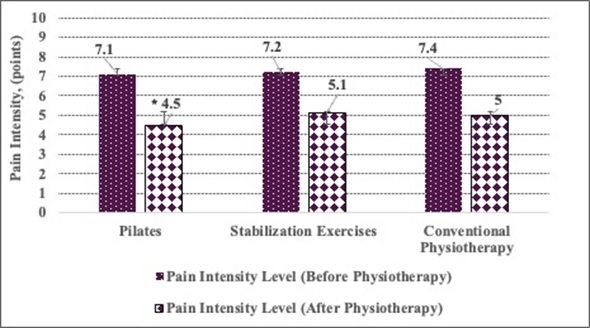 Figure 2: Pain intensity assessment between the groups.
Figure 2: Pain intensity assessment between the groups.
Statistical significance (p ≤ 0.05). Values are presented as arithmetic means ( x ) ± standard error of the mean ( Sx ).
The participants’ lower back functional level was assessed using The Oswestry Low Back Pain Disability Questionnaire [8]: This table presents the functional status results according to the Oswestry questionnaire, comparing the participants’ scores before and after the exercise program. The Oswestry questionnaire results for the Pilates group participants were 12.8±2.35% before the exercise program, and after the intervention, the average functional status improved to 9±1.94%, representing an improvement of 3.8%. The results for the stabilization exercise group participants were 13±3.68% before the program, and after application, the mean decreased to 9.8±2.89%, corresponding to a 3.2% improvement in the mean score. The control group, which received physiotherapy, had results of 14±4.42% before, and after application, the score decreased to 10.4±3.98%, a 3.6% change. Based on this data, it can be stated that all groups demonstrated a positive effect on improving functional status. However, the Pilates method achieved the greatest average improvement, which was 3.7%; therefore, it can be said that the Pilates method was slightly more effective than the other therapies (Figure 3).
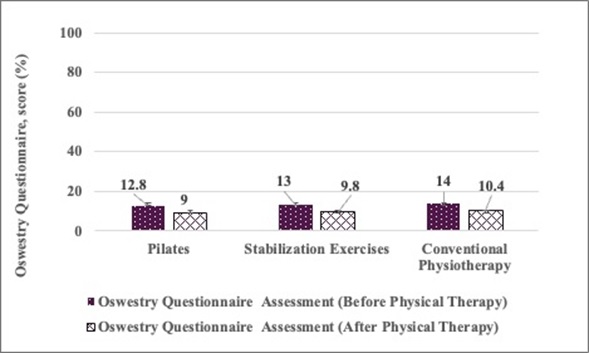 Figure 3: Patient's permanent functional low back disability assessed between the groups.
Figure 3: Patient's permanent functional low back disability assessed between the groups.
Statistical significance (p ≤ 0.05). Values are presented as arithmetic means ( x ) ± standard error of the mean ( Sx ).
Discussion
Our study showed that all three methods positively affected lumbar mobility (Figure 1). Significant improvements in lumbar flexibility were observed across all groups, with conventional physiotherapy yielding the greatest increase in lumbar spine flexibility. A greater improvement in mobility was recorded in the control group, which engaged in physiotherapy exercises, including strengthening and stretching. This finding aligns with previous studies, indicating that combining stretching and strengthening exercises enhances lumbar spine flexibility [15]. Based on our research results, all three intervention methods—Pilates, stabilization exercises, and conventional physiotherapy—positively affected lumbar spine mobility. The results suggest that a twelve-week intervention involving Pilates, stabilization exercises, and physiotherapy can effectively reduce pain, improve function, and increase lumbar mobility in patients with chronic low back pain (Figure 2). These findings are consistent with those of a study by [16], which reported significant pain reduction and functional improvement over four weeks. Short-term interventions may yield transient effects, necessitating sustained exercise for enduring results. Examining research by other researchers, these approaches have demonstrated efficacy in addressing lumbar radiculopathy [17]. Found that lumbar stabilization can reduce pain intensity and enhance function in individuals with lumbar radiculopathy. Stabilization exercises activate deep muscles and improve stability, reducing the lumbar load and increasing the range of motion. These findings are pertinent to our study, which observed improvements in lumbar flexibility in the yoga group. Both Pilates and stabilization exercises improved postural control and core muscle strength, thereby enhancing spinal function. Although both [17] and our study reported improvements in pain and functionality, longer studies would better evaluate the long-term effects of stabilization exercises on these outcomes. According to [18], all interventions had a positive impact, with the most significant effect in the Pilates group. Compared to our study implementing Pilates, stabilization, and physiotherapy interventions, the results showed similar trends, with improvements across all groups and the most pronounced change in the Pilates group. The Pilates method may be advantageous for patients with chronic low back pain because of its focus on body stabilization and movement control. While Bhadauria and Gurudut conducted programs over six weeks, our twelve-week study showed positive outcomes. Our research revealed that conventional physiotherapy was the most effective for lumbar spine mobility. All methods provided clinical benefits. The Pilates, stabilization, and physiotherapy groups showed improvements, as these approaches strengthened the deep stabilizing muscles and enhanced muscle balance in the lumbar region. Functional low back assessment results indicated that stabilization exercises and physiotherapy methods improved the participants’ functional condition, although their effectiveness was lower (Figure 3). This suggests that Pilate’s methods could be considered more effective for reducing disability and improving function in lumbar spine issues. All intervention groups experienced a significant reduction in lumbar pain intensity over the 12-week program. The results showed that the Pilates method yielded the most pronounced reduction in pain, exceeding the changes in the other groups. Other interventions, such as stabilization exercises and physical therapy, also contributed to reducing pain intensity, albeit to a lesser extent. Previous research has shown that Pilates alleviates pain and enhances quality of life and lumbar function [19,20] affirmed that Pilates methods improve functional status and mitigate pain [21]. Observed that Pilates exercises effectively diminished pain in patients with lower back pain. A systematic review by Miyamoto, G. C., with collogues, concluded that the Pilates method is effective in reducing short-term pain in patients with lumbar back disorders [22]. Fernandes and Oliveira [23] systematically evaluated the efficacy of Pilates exercises in alleviating back pain. Fernandes and Oliveira found that Pilates exercises effectively alleviated pain and enhanced lumbar function. These outcomes are consistent with those of the current study. Similarly, Wahyuni and Kurnia's [24] meta-analysis demonstrated that stabilization exercises significantly reduced pain intensity, corroborating the findings of the present study, in which both groups reported pain reduction. Drawing from this study and other sources, Pilates, stabilization, and physiotherapy exercises are efficacious in mitigating lumbar pain and enhancing functional status. Despite variations in exercise type and duration across studies, all interventions yielded positive outcomes. The Pilates method, which integrates muscle control, flexibility, and stability training, produced the most favorable results. Regular stabilization exercises contribute to pain reduction and improved muscle activation. While short-term programs yield significant benefits, long-term interventions ensure more enduring improvement. Consistent lumbar exercises are crucial for treatment, with optimal results achieved through sustained practice. In the future, it would be worthwhile to investigate whether these positive changes persist over a longer period of time.
Key Points
What is already known on this topic:
- Lumbar radiculopathy causes pain and disability; rehab methods are under debate.
- Pilates and stabilization may help pain and function, but evidence is limited.
What this study adds:
- Pilates and stabilization effectively reduce pain and improve function in radiculopathy.
- Pilates showed slightly better results for pain reduction and disability than other methods.
How this study might affect research, practice, or policy:
- Multimodal rehab with Pilates/stabilization should be considered for radiculopathy.
- Sustained home-based exercise and ergonomic advice maximize long-term results.
Conclusion
The core conclusion of this study is that both Pilates and stabilization techniques are effective in reducing pain and improving function in patients with lumbar radiculopathy, with Pilates showing slightly greater efficacy in pain reduction and functional improvement, while conventional physiotherapy most improved lumbar mobility.
- Practical Recommendations
For rehabilitation professionals managing lumbar radiculopathy, a multimodal program, including Pilates and stabilization exercises, is recommended to maximize pain relief, functional recovery, and spinal mobility. Patients should be encouraged to continue home-based exercise and maintain ergonomic behaviors.
- Recommendations
For physiotherapists: When working with patients suffering from lumbar radiculopathy, apply a program that combines Pilates and stabilization exercises to achieve better results. These methods help strengthen the core muscles, improve spinal mobility, and reduce pain. Special attention should be paid to fostering ergonomic movement and correct posture.
For patients: It is recommended to continue the prescribed exercise program at home, focusing on strengthening the abdominal and lower back muscles. In addition, patients are advised to follow ergonomic principles in daily activities—use correct body mechanics when lifting objects.
Limitations
Further investigation is needed on long-term efficiency and maintenance of benefits, as the current study period was 12 weeks. Longer studies are needed to clarify the sustained impact of Pilates and stabilization exercises.
Acknowledgement
We sincerely thank the study participants for their cooperation.
Disclosure of AI usage
In this assignment, I used Paperpal tool https://www.paperpal.com/ for grammar correction and language editing. The outputs were reviewed, adapted, and integrated into my own work, which reflects my personal understanding and complies with the academic integrity policy of my institution.
Conflict of Interest
The authors declare no conflicts of interest.
Funding
This study received no funding.
References
- Alexander CE, Weisbrod LJ, Varacello MA (2025) Lumbosacral radiculopathy. NCBI Bookshelf, USA.
- Trevlaki E, Panagiotopoulou E, Trevlakis E, Chalkia A, Xristara-Papadopoulou A (2023) Neuropathic Pain and Lumbar Spinal Column Injuries: A Chronic Perspective. EJMED 5: 81-86.
- Zaicenkoviene K, Mankšta P (2016) Kaunas: Lietuvos sporto universitetas ISBN: 9786098040982.
- Hlaing SS, Puntumetakul R, Khine EE, Boucaut R (2021) Effects of core stabilization exercise and strengthening exercise on proprioception, balance, muscle thickness and pain-related outcomes in patients with subacute nonspecific low back pain: a randomized controlled trial. BMC Musculoskelet Disord 22: 746.
- Miftari S, Rrecaj-Malaj S, Murtezani A, Ismajli B, Aliu M (2024) Comparative analysis of two different physiotherapy intervention programs in individuals experiencing chronic lower back pain. Rom J Med Pract 19.
- Hayes MHS, Patterson DG (1921) Experimental development of the graphic rating method. Psychol Bull 18: 98-99.
- Islam M, Ahmed S, Rahman M, Chowdhury R, Khatun M (2022) Effectiveness of core stabilization exercise along with conventional physiotherapy on pain, proprioception and disability in patients with chronic low back pain: a randomized control trial protocol. Fortune Journals 4: 205-210.
- Fairbank JCT, Pynsent PB (2000) The Oswestry Disability Index. Spine 25: 2940-2952.
- Yates M, Shastri-Hurst N (2017) The Oswestry Disability Index. Occup Med (Lond) 67: 241-242.
- Willhuber GOC, Piuzzi NS (2025) Straight Leg Raise Test. StatPearls Publishing, USA.
- Mier CM, Gibson AL (1997) Evaluation of a novel body flexibility assessment using the fingertip-to-floor test. Res Q Exerc Sport 68: 156-160.
- Becker L, Schomig F, Cordes LMS, Duda GN, Pumberger M, et al. (2023) Finger-floor distance is not a valid parameter for the assessment of lumbar mobility. Diagnostics 13: 638.
- Kendall FP, McCreary EK, Provance PG (1993) Muscles: Testing and function. Williams & Wilkins, USA.
- Cronkleton E (2020) 10 yoga poses for back pain. Healthline, USA.
- Bussell DL, McCarthy DM, Strauss JP (2016) The effects of combined strengthening and stretching exercises on flexibility in individuals with chronic low back pain. J Rehabil Res Dev 53: 215-223.
- Sakulsriprasert P, Vachalathiti R, Kingcha P (2020) Responsiveness of pain, functional capacity tests, and disability level in individuals with chronic nonspecific low back pain. Hong Kong Physiother J 40: 11-17.
- Kostadinovic S, Milovanovic N, Jovanovic J, Tomaševic-Todorovic S (2020) Efficacy of the lumbar stabilization and thoracic mobilization exercise program on pain intensity and functional disability reduction in chronic low back pain patients with lumbar radiculopathy: a randomized controlled trial. J Back Musculoskelet Rehabil 33: 975-983.
- Bhadauria EA, Gurudut P (2017) Comparative effectiveness of lumbar stabilization, dynamic strengthening, and Pilates on chronic low back pain: randomized clinical trial. J Exerc Rehabil 13: 477-485.
- Natour J, Cazotti LA, Ribeiro LH, Baptista AS, Jones A (2015) Pilates improves pain, function and quality of life in patients with chronic low back pain: a randomized controlled trial. Clin Rehabil 29: 59-68.
- Cruz-Díaz D, Romeu M, Velasco-González C, Martínez-Amat A, Hita-Contreras F (2018) The effectiveness of 12 weeks of Pilates intervention on disability, pain and kinesiophobia in patients with chronic low back pain: a randomized controlled trial. Clin Rehabil 32: 1249-1257.
- Eliks M, Zgorzalewicz-Stachowiak M, Zenczak-Praga K (2019) Application of Pilates-based exercises in the treatment of chronic non-specific low back pain: State of the art. Postgrad Med J 95: 567-572.
- Miyamoto GC, Costa LOP, Cabral CMN (2013) Efficacy of the Pilates method for pain and disability in patients with chronic nonspecific low back pain: a systematic review with meta-analysis. Braz J Phys Ther 17: 517-532.
- Fernandes SF, Oliveira AR (2023) Effectiveness of Pilates exercise on low back pain: a systematic review with meta-analysis. J Back Musculoskelet Rehabil 36: 295-306.
- Wahyuni W, Kurnia NE (2023) The effectiveness of core stability exercises on pain in patients with low back pain: a meta-analysis. Phys Ther J Indones 4: 1-9.v
Citation: Andrejeva J, Ulinskaite A, Dubey VP, Piekuviene V (2025) The Effect of Pilates and Stabilization Techniques on Pain and Function for Patients with Lumbar Radiculopathy. HSOA J Altern Complement Integr Med 11: 651.
Copyright: © 2025 Julija Andrejeva, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

