
The Incidence Rate of Bacteremia in Patients with Enterocutaneous Fistula and its Influencing Factors
*Corresponding Author(s):
Guosheng GuDepartment Of General Surgery, Anhui No. 2 Provincial Peoples’ Hospital, Hefei, Anhui, China
Email:995340746@qq.com
Abstract
Background
Enterocutaneous fistulae are usually accompanied by abdominal infections, and bacteraemia is a major complication affecting disease regression in the treatment of enterocutaneous fistulae as well as abdominal infections. The aim of this study was to investigate the incidence of bacteraemia in patients with enterocutaneous fistula during the course of treatment and to analyze the factors that potentially influence it.
Methods
Clinical data of patients presenting with enterocutaneous fistulae between September 2022 and September 2023 were retrospectively collected. One-way ANOVA and binary logistic stepwise regression analysis were conducted to investigate the relationship between enterocutaneous fistula and bacteraemia.
Results
A total of 188 patients who met the criteria for enterocutaneous fistulae were included in this study, of which 42 developed bacteraemia during treatment. The presence of a central venous catheter, electrolyte disturbances, low haemoglobin and multiple fistulas are risk factors for bacteraemia.
Conclusion
This study suggests that central venous catheters and electrolyte disturbances increase the incidence of bacteraemia in patients with enterocutaneous fistulae. According to this study, reduction of unnecessary central venous catheterisation and timely correction of electrolyte disorders are effective response strategies to reduce the incidence of bacteraemia.
Keywords
Enterocutaneous Fistula; Bacteremia; Central Venous Catheter; Parenteral nutrition; Cross-sectional Study.
Introduction
An enterocutaneous fistula has been commonly recognized as an abnormal passage, emerging between the gastrointestinal tract and adjacent viscera or extraperitoneal domain, facilitating the unwarranted egress of intestinal contents. This pathological state engenders a spectrum of clinical presentations, encompassing intra-abdominal infections, electrolyte perturbations, and organ dysfunction. In its nascent phase, afflicted individuals frequently contend with profound abdominal sepsis alongside cutaneous and subcutaneous tissue involvement, precipitated by the discharge of enteric contents. Until infection has been adequately managed and a proficient drainage pathway has been established, numerous patients, particularly those harboring high fistula placements and enduring digestive fluid losses exceeding 500 ml daily, have suffered substantial depletion of nutrients and electrolytes alongside their digestive exudates. Following infection resolution and digestive fluid loss, many individuals afflicted with enterocutaneous fistulae have succumbed to malnutrition, anemia, hypoproteinemia, and electrolyte imbalances [1].
Bacteremia has been commonly recognized as a systemic infection instigated by the infiltration of pathogens into the bloodstream, typically heralded by symptoms such as chills, malaise, and fever, its occurrence intricately intertwined with the location and magnitude of the patient's lesion and the body's inherent resilience. Bacteremia often surges in cases of patient malnutrition and invasive medical interventions. The advent of bacteremia exacerbates patient distress, protracts hospital stays, inflates healthcare expenditures, and amplifies mortality rates, particularly among critically ill individuals. Amongst critically ill patients grappling with enterocutaneous fistulas, the prevalence of bacteremia has been instrumental in yielding a mortality rate of 19.81% [2]. Therefore, it is important to understand the risk factors for bacteremia in patients with enterocutaneous fistulae and to intervene early to reduce its occurrence.
Given the inherent characteristics of enterocutaneous fistulas, some patients may develop bacteremia during treatment, introducing additional risks. Therefore, early identification of risk factors for bacteremia in patients with enterocutaneous fistulas is crucial. The timely initiation of preventive antimicrobial therapy holds paramount significance in reducing the incidence of bacteremia and facilitating the effective management of enterocutaneous fistulas. The objective of this study was to examine the incidence of bacteremia during the treatment of patients with enterocutaneous fistulas, as well as to explore potential influencing factors contributing to the occurrence of bacteremia.
Materials And Methods
Design
This study is a cross-sectional design. The study has been conducted in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies [3].
Study setting and sampling
A retrospective selection of enterocutaneous fistula patients has been conducted, covering the period between 1 September 2022 and 1 September 2023, by querying the medical records system. The patients' medical records have been collected to gather the following information: age, gender, hemoglobin levels, BMI, electrolyte levels at the time of admission, the etiology of the enterocutaneous fistula, the number of fistulas, whether central venous cannulation was performed, and the presence of any comorbidities with chronic diseases. The study has been approved by the Hospital Ethics Committee under approval number (R) 2024-033.
Inclusion and exclusion criteria
The inclusion criteria are as follows:
- Diagnosed with intestinal fistula through imaging studies: Patients must have a confirmed diagnosis of intestinal fistula based on imaging studies (Figure 1).
- Complete medical records available: Only patients with comprehensive and accessible medical records are included in the study.
- Initial control of abdominal infection on admission: The patient must have a temperature of ≤ 37.5°C for at least 3 consecutive days after admission and have a CRP of ≤ 10 mg/L and a WBC of ≤ 10*10^9 to demonstrate initial control of the abdominal infection.
- All febrile patients undergo blood culture examination: Blood culture examination is a mandatory criterion for individuals presenting with fever.
Exclusion criteria are as follows:
- Presence of infections in other locations besides the intestinal fistula: Patients with infections in locations other than the intestinal fistula, such as pulmonary or urinary tract infections, will be excluded;
- Withdrawal from treatment for reasons unrelated to intestinal fistula: Individuals who withdraw from treatment for reasons unrelated to their intestinal fistula or those with an actual hospitalization duration less than 7 days will be excluded.
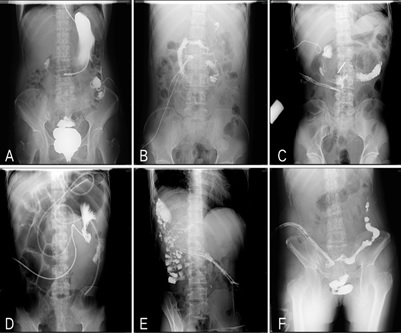 Figure 1: Imaging pictures of several cases of typical intestinal fistulas. A: Fistulae in the stomach and splenic flexure of the colon. B: Fistula in descending part of duodenum.C: Fistula in horizontal part of duodenum. D: Fistula in the jejunum.E: Fistula in the hepatic flexure of the colon.F: Fistula in the sigmoid colon.
Figure 1: Imaging pictures of several cases of typical intestinal fistulas. A: Fistulae in the stomach and splenic flexure of the colon. B: Fistula in descending part of duodenum.C: Fistula in horizontal part of duodenum. D: Fistula in the jejunum.E: Fistula in the hepatic flexure of the colon.F: Fistula in the sigmoid colon.
Variables
The potential confounders involved in this study are defined below:
- Age (years), hemoglobin (g/L), and BMI are values at the first day of the patient's admission.
- Causes of intestinal fistula: (1) Surgery and trauma: These include enterocutaneous fistulae caused by intraoperative accidents or poorly healed postoperative anastomoses after the patient has undergone surgical treatment, and enterocutaneous fistulae caused by traumatic injuries, such as traffic accidents and falls from a height; (2) Tumor: This refers to an intestinal fistula resulting from the invasion of the digestive tract by a progressing tumor, or an intestinal fistula resulting from non-surgical treatment of a patient with a tumor. (3) Other: This mainly includes enterocutaneous fistulae due to diseases such as acute severe pancreatitis, Crohn's disease, and ulcerative colitis.
- Chronic disease: This refers to patients with hypertension, coronary heart disease and chronic renal insufficiency who have been diagnosed in hospital and are/have been treated.
- Central venous catheters: The refers to catheters whose tips are located in the superior or inferior vena cava, and this study mainly included central venous catheters (CVCs) placed via the internal jugular/subclavian veins and peripherally inserted central catheters (PICCs).
- Number of fistulae: The number of fistulas is determined by imaging, and more than 1 fistula is referred to as multiple fistulas.
- Electrolyte disturbances: This refers to K+ > 5.5 mmol/L or < 3.5 mmol/L; Na+ >145 mmol/L or < 135 mmol/L; Cl- > 106 mmol/L or < 96 mmol/L.
Data collection
These data were collected by two long-time enterocutaneous fistula practitioners who retrospectively collected enterocutaneous fistula patients seen between September 2022 and September 2023 by reviewing case systems and imaging systems. All patients with enterocutaneous fistula were imaged to clarify the diagnosis of enterocutaneous fistula.
Data analysis
Statistical analysis of the data was performed using SPSS 20.0 software. In univariate analysis, categorical data were expressed as frequencies and percentages (%), and comparisons between groups were made using the χ2 test. Continuous data were expressed as mean ± standard deviation (x ± s) and t-test was used for comparison between groups. The level of significance for all analyses was α = 0.05. In binary logistic stepwise regression analyses, the presence of bacteraemia was used as the dependent variable, and variables with p < 0. 05 in univariate analyses were used as covariates, with the following specific assignments of the categorical covariates (supplementary Table): cause of fistula (surgery or trauma = 0, tumor = 1, other = 2), central venous catheter (none = 0, yes = 1), number of fistulae (single fistulae = 0, multiple fistulas = 1), and electrolyte disorders (none = 0, yes = 1). The "Forward: Condition" variable entry method was selected, with an input step probability of 0.10 and a deletion step probability of 0.15. These statistical methods were used to assess and compare various factors between groups of patients to ensure a reliable and comprehensive analysis of the data collected during the study.
Results
Univariate Analysis of Bacteremia Occurrence in Intestinal Fistula Patients
As shown in Table 1, a total of 188 patients with enterocutaneous fistulae were investigated in this study, all of them had the location and number of fistulae clarified by X-ray, out of which 42 were diagnosed with bacteraemia during hospitalization, the incidence of bacteraemia was 22.34%. When comparing patients who developed bacteremia with those who did not, no statistically significant differences were found in terms of gender, BMI at admission, and the presence of underlying diseases (p > 0.05).
However, notable variations were identified in age, hemoglobin levels, presence of electrolyte disorders, causes of intestinal fistula, number of fistula sites, and central venous catheterization, all of which exhibited statistically significant differences (p < 0.05). These findings underscore the importance of considering these factors in assessing the risk and occurrence of bacteremia in intestinal fistula patients.
Binary logistic stepwise regression analysis of bacteremia occurrence in patients with enterocutaneous fistula
Binary logistic stepwise regression analysis was performed with the incidence of bacteraemia in patients with enterocutaneous fistulae as the dependent variable. Independent variables were selected based on factors with p < 0.05 in univariate analysis (Table 1) and coded accordingly.
|
|
bacteremia n=146 |
no bacteremia n=42 |
χ2 |
p |
|
Age(years) |
51.32±15.80 |
57.24±15.09 |
|
0.032 |
|
Hemoglobin(g/L) |
107.84±19.66 |
94.32±20.57 |
|
0.003 |
|
BMI |
19.961±3.91 |
19.936±3.53 |
|
0.977 |
|
Sex |
|
|
|
|
|
male |
87(59.59) |
26(61.90) |
0.073 |
0.787 |
|
female |
59(40.41) |
16(38.10) |
||
|
Causes of fistula |
|
|
|
|
|
surgery or trauma |
83(56.85) |
19(45.24) |
11.961 |
0.003 |
|
tumor |
21(14.38) |
16(38.10) |
||
|
other |
42(28.77) |
7(16.67) |
||
|
Chronic disease |
|
|
|
|
|
N |
121(82.88) |
30(71.43) |
2.704 |
0.100 |
|
Y |
25(17.12) |
12(28.57) |
||
|
Central venous catheters |
|
|
|
|
|
N |
67(45.89) |
2(4.76) |
23.794 |
0.000 |
|
Y |
79(54.11) |
40(95.24) |
||
|
Number of fistulae |
|
|
|
|
|
single |
116(79.45) |
27(64.29) |
4.121 |
0.042 |
|
multiple |
30(20.55) |
15(35.71) |
||
|
Electrolyte disturbances |
|
|
|
|
|
N |
104(71.23) |
19(45.24) |
9.743 |
0.002 |
|
Y |
42(28.77) |
23(54.79) |
Table 1: Characteristics of patients with enterocutaneous fistula
The results of the analysis showed that low haemoglobin on admission, electrolyte disturbances, central venous catheterisation during the course of the disease, and more than 1 fistula were identified as risk factors for the development of bacteraemia, with p < 0.05 for electrolyte disturbances and central venous catheterisation. These results further emphasise the importance of these specific factors in predicting and understanding the likelihood of bacteraemia in patients with enterocutaneous fistulae (Table 2).
|
|
Regression coefficient |
Standard error |
p-value |
OR |
95%CI |
|
Hemoglobin |
-0.028 |
0.015 |
0.068 |
0.972 |
0.943∼1.002 |
|
Central venous catheters |
1.973 |
0.801 |
0.014 |
0.139 |
0.029∼0.668 |
|
Number of fistulae |
0.891 |
0.547 |
0.103 |
0.410 |
0.141∼1.198 |
|
Electrolyte disturbances |
1.728 |
0.544 |
0.001 |
0.178 |
0.061∼0.516 |
Table 2: Binary logistic stepwise regression analysis of the bacteremia in patients with enterocutaneous fistula
To further explore which potential causative factor was most associated with the development of bacteraemia, we compared the area under the ROC curve (supplementary Figure), where the greatest impact on the development of bacteraemia was water electrolyte disturbances with an area under the curve of 0.749, followed by central venous catheterisation with an area under the curve of 0.690 (Table 3).
|
|
Area |
Standard error |
p-value |
95%CI |
|
Hemoglobin |
0.681 |
0.064 |
0.004 |
0.556∼0.806 |
|
Central venous catheters |
0.690 |
0.050 |
0.003 |
0.591∼0.788 |
|
Number of fistulae |
0.618 |
0.065 |
0.065 |
0.490∼0.746 |
|
Electrolyte disturbances |
0.749 |
0.055 |
0.000 |
0.642∼0.856 |
Table 3: Area under the ROC curve for each variable
Discussion
Bacteremia in Enterocutaneous Fistula Patients and Central Venous Catheterization
Given the inherent characteristics of enterocutaneous fistula, which often coexists with intra-abdominal infection and malnutrition, effective management poses unique challenges [4]. In the early stages of treatment, parenteral nutrition becomes imperative. Since the introduction of total parenteral nutrition (TPN) in the 1970s, there has been a noteworthy reduction in the mortality rate among intestinal fistula patients, emphasizing the critical role of parenteral nutrition in their treatment [5,6].
However, the use of parenteral nutrition, being a hypertonic solution, can lead to complications such as swelling, pain, thrombosis, and phlebitis when administered through peripheral veins over an extended period. Consequently, central venous catheterization becomes a necessary intervention during parenteral nutrition in intestinal fistula patients. Despite its utility, central venous catheterization is an invasive procedure associated with various complications, with catheter-related bloodstream infections (CLABSI) being the most prevalent. Studies have reported an incidence of CLABSI in central venous catheterization as 29.2% [7].
In the context of enterocutaneous fistula patients, the presence of concurrent intra-abdominal infection complicates the clinical picture. Symptoms like chills, rigors, and fever, coupled with positive blood cultures, can sometimes pose a diagnostic challenge, making it difficult to distinguish whether the origin is intra-abdominal infection or catheter-related [8,9]. In such instances, the term "bacteremia" is employed without specifying the source [10]. Our study corroborates existing evidence, highlighting central venous catheterization as an independent risk factor for bacteremia in intestinal fistula patients, as supported by a significant P-value of 0.014. These findings underscore the importance of careful consideration and management of central venous catheterization to minimize the risk of bacteremia in this patient population.
Bacteremia in Enterocutaneous Fistula Patients and Electrolyte Disorders
Intestinal fistulas, categorized based on digestive fluid volume as high-output (>500 ml/day) and low-output (<500 ml/day), present unique challenges related to electrolyte imbalance [11-13]. Gastric, duodenal, and proximal jejunal fistulas, characterized by the loss of gastric juice, pancreatic juice, bile, and small intestine fluid, often result in substantial electrolyte depletion, including K+, Na+, Cl-, and others. Consequently, electrolyte disorders emerge as a common complication in intestinal fistula patients [14-16].
Our study revealed a significant association between bacteremia incidence and electrolyte disorders at admission, with patients exhibiting abnormal electrolyte levels experiencing a higher frequency of bacteremia compared to those with normal levels. Multivariate analysis further identified electrolyte disorders as a significant risk factor for bacteremia. This underscores the critical role of timely correction of electrolyte disorders in intestinal fistula patients, particularly those with high-output fistulas.
To mitigate the risk of electrolyte disorders, regular monitoring of electrolyte levels is essential. Establishing effective drainage and reinfusion pathways proves crucial in managing electrolyte balance in these patients [17,18] For those lacking reinfusion pathways or with high fistula output, the use of acid-suppressing drugs and somatostatin to inhibit digestive fluid secretion becomes increasingly important. These findings emphasize the importance of a comprehensive approach, encompassing regular assessments and targeted interventions to optimize electrolyte management in intestinal fistula patients, ultimately contributing to a reduction in the incidence of bacteremia.
Bacteremia in Enterocutaneous Fistula Patients and number of fistulas
The number of fistula sites emerged as a crucial factor influencing the treatment of enterocutaneous fistula patients. A higher number of fistulas often signifies greater disease complexity and increased difficulty in managing complications such as intra-abdominal infection and electrolyte disorders.
Our findings indicated that patients with two or more fistulas had a higher proportion of bacteremia compared to those with a single fistula, and this difference was statistically significant (p = 0.042). This emphasizes the impact of the number of fistula sites on the overall clinical complexity and underscores the need for a tailored and comprehensive approach in managing enterocutaneous fistula patients, especially those with multiple fistulas, to minimize the risk of bacteremia and optimize treatment outcomes.
Baseline Conditions in Enterocutaneous Fistula Patients and Bacteremia
The occurrence of bacteremia is partly due to uncontrolled sources of infection and partly due to the patient's own resistance. In our study, the age of patients in the bacteremia group was higher than in the non-bacteremia group, with statistical significance in univariate analysis (p = 0.032). Regarding underlying diseases, we mainly recorded whether patients had hypertension, diabetes, or coronary heart disease, finding no significant difference between the two groups (p = 0.100). Enterocutaneous fistula patients, due to disease consumption and loss of digestive fluids, are often in a state of malnutrition. We used hemoglobin and BMI as indicators to assess the nutritional status of patients. In our study, there were statistically significant differences between the bacteremia and non-bacteremia groups in terms of hemoglobin (p=0.003) levels, while there was no significant difference in BMI (p = 0.977).
Type of Enterocutaneous Fistula and Bacteremia
Enterocutaneous fistulas have diverse etiologies, with common clinical types including postoperative fistulas resulting from poor healing at anastomosis sites or accidental injury during surgery, tumor-related fistulas caused by tumor necrosis or radiation-induced intestinal injury, and trauma-related fistulas resulting from accidents and injuries [19,20]. Other causes encompass acute severe pancreatitis, inflammatory bowel disease, and diverticular perforation. Each etiology gives rise to distinct baseline states in patients and varying pathophysiological conditions around the fistula [21]. In this study, our primary focus was the analysis and comparison of the incidence of bacteremia in fistulas related to surgery, trauma, tumors, and other causes. Univariate analysis revealed statistically significant differences among these groups (p = 0.003).
Conclusion
This study showed that the incidence of bacteremia in patients with enterocutaneous fistula during treatment was 22.34%. Additionally, this study presented that age, hemoglobin, central venous catheter, electrolyte disorders, cause of enterocutaneous fistulae, and number of fistulae had an effect on the development of bacteremia in patients with enterocutaneous fistulae. The presence of a central venous catheter and electrolyte disturbances are among the independent risk factors for the development of bacteremia.
Author Contribution
Ting Gong and Yong Peng were involved in conceptualization, data curation, formal analysis, investigation, methodology, validation, writing—original draft and writing—review & editing; Shu Zhang, Fang fang Cao, Zheng Zhou, Jianbin Wang were involved in data curation, formal analysis, methodology, project administration, resources, supervision, validation; Canwen Chen and Guosheng Gu contributed to project conceptualization, supervision, writing—review & editing.
Funding
This research was funded by the Key Program of Natural Science Research Projects of Colleges and Universities of the Department of Education of Anhui Province (2022AH052319), and Key Scientific Research Projects of Anhui Provincial Health Commission (AHWJ2022a026).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the institutional review board of Anhui No. 2 Provincial Peoples’ Hospital (Approval number: 2022a026).
Informed Consent Statement
Due to the retrospective nature of the study, informed conssent was waived.
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to patient privacy concerns.
Acknowledgments
We thank all the participants and healthcare professionals who made this study possible at department of general surgery of the Second People's Hospital of Anhui Province and the department of general surgery of the Affiliated BenQ Hospital of Nanjing Medical University.
Conflicts of Interest
The authors have declared no conflict of interest.
References
- Aguilar-Espinosa F, Barba-Jaramillo ED, Sánchez-Muñoz MP, Camba-Gutiérrez IS, Lincango-Naranjo EP (2023) Management of High Output Enterocutaneous Fistula due to Richter's Hernia After Gastric Bypass: Video Demonstration. Obes Surg 33: 687-690.
- Dokmak A, Sweigart B, Orekondy NS, Jangi S, Weinstock JV, et al. (2024). Efficacy and Safety of Hyperbaric Oxygen Therapy in Fistulizing Crohn's Disease: A Systematic Review and Meta-analysis. J Clin Gastroenterol 58: 120-130.
- Fajardo R, Núñez-Rocha RE, Gómez-Carrillo D, Pedraza JD, López R, et al. (2023) Giant squamous cell carcinoma developed on a mesh-related enterocutaneous fistula: A case report: Int J Surg Case Rep 109: 108581.
- Fukushima S, Hagiya H, Fujita K, Kamiyama S, Yamada H, et al. (2022) Clinical and microbiological characteristics of polymicrobial bacteremia: a retrospective, multicenter study. Infection 50: 1233-1242.
- Gefen R, Garoufalia Z, Zhou P, Watson K, Emile SH, et al. (2022) Treatment of enterocutaneous fistula: a systematic review and meta-analysis. Tech Coloproctol, 26: 863-874.
- Ghimire P (2022) Management of Enterocutaneous Fistula: A Review. JNMA J Nepal Med Assoc 60: 93-100.
- Grainger JT, Maeda Y, Donnelly SC, Vaizey CJ (2018) Assessment and management of patients with intestinal failure: a multidisciplinary approach. Clin Exp Gastroenterol 11: 233-241.
- Islam MS, Gafur MA, Mahmud AA, Mahiuddin M, Khan SA, et al. (2018) Clinicopathological Study of Enterocutaneous Fistula in Mymensingh Medical College Hospital. Mymensingh Med J 27: 513-519.
- Kay TJ, Gallagher PJ (2023) A case of acute pancreatitis and enterocutaneous fistula formation following extended right hemicolectomy: J Surg Case Rep 122.
- Kumar P, Maroju NK, Kate V (2011) Enterocutaneous fistulae: etiology, treatment, and outcome - a study from South India. Saudi J Gastroenterol 17: 391-395.
- Lee RA, Stripling JT, Spellberg B, Centor RM (2023) Short-course antibiotics for common infections: what do we know and where do we go from here? Clin Microbiol Infect 29: 150-159.
- Lloyd DA, Gabe SM, Windsor AC (2006) Nutrition and management of enterocutaneous fistula. Br J Surg 93: 1045-1055.
- Lorente L, Galvan R, Martín MM, García C, Huidobro S, et al. (2003) Bacteremia mortality according to microorganism responsible and origin source of bacteremia in critically ill patients.
- Mahoney EJ, Bugaev N, Appelbaum R, Goldenberg-Sandau A, Baltazar GA, et al. (2022) Management of the open abdomen: A systematic review with meta-analysis and practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg 93: e110-e118.
- Newman N, Issa A, Greenberg D, Kapelushnik J, Cohen Z, et al. (2012) Central venous catheter-associated bloodstream infections. Pediatr Blood Cancer 59: 410-414.
- Novy E, Roger C, Roberts JA, Cotta MO (2023) Pharmacokinetic and pharmacodynamic considerations for antifungal therapy optimisation in the treatment of intra-abdominal candidiasis. Crit Care 27: 023-04742.
- Rizka H, Diyah EA (2023) Route delivery of nutrition in patients with enterocutaneous fistula. Med J Malaysia 78: 541-546.
- Struchkov VY, Berelavichus SV, Dvuhzhilov MV, Akhtanin EA, Kriger AG (2023) Complex treatment of multiple high-output enterocutaneous fistulas (gastric, jejunum, transversum) after bariatric surgery: J Surg Case Rep 7: rjad096.
- Tan DW, Yan CL, Yeh DD, Thakkar-Rivera N (2023) Enterocutaneous fistula formation after cardiac transplantation due to injury from LVAD driveline migration. BMJ Case Rep 16: e254696.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, et al. (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370: 1453-1457.
- Wright A, Wright M (2011) Bedside management of an abdominal wound containing an enteroatmospheric fistula: a case report. Ostomy Wound Manage 57: 28-32.
Citation: Gong T, Peng Y, Zhang S, Cao F, Zhou Z, et al. (2025) The Incidence Rate of Bacteremia in Patients with Enterocutaneous Fistula and its Influencing Factors. Archiv Surg S Educ 7: 056.
Copyright: © 2025 Ting Gong, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

