
The Link between Lipid Profile, Cardiovascular Risk and Mood Disorders Appearance in Older Patients
*Corresponding Author(s):
Rozeta Draghici“Ana Aslan” National Institute Of Gerontology And Geriatrics, Bucharest, Romania
Tel:+40 744673819,
Email:rozetadraghici@gmail.com
Abstract
Several studies established that there is a relationship between serum lipid profile and various psychopathological conditions. Aim of the study was to investigate a possible association between lipid changes, cardiovascular risk and mood disorders appearance in older patients. Observational cross-sectional study included 242 patients over 55 years old: 134 with mood disorders and 108 control group. Atherogenic index was computed as log (triglycerides/HDL-cholesterol) and HeartScore from a cardiovascular disease risk assessment system.
Study data revealed that patients with mood disorders have low HDL-cholesterol (p<0.05) and high atherogenic index and HeartScore (p
Keywords
Atherogenic index; HeartScore; Mood disorders; Older patients
Introduction
Mood Disorders (MD), also called affective disorders, consist of a variety of conditions characterized by a disturbance in mood as the main feature. Any disturbance in emotional states that causes discomfort or hinders our ability to function properly is a form of mood disorder. Symptoms vary by individual, and can range from mild to severe. If mild or occasional changes mood may be normal, if more severe they may be a sign of a major depressive disorder, a dysthymic reaction or be symptomatic of a bipolar disorder. Also, other mood disorders may be caused by a general medication condition. According of new DSM-5 classification the main types of affective disorders are bipolar disorders and depressive disorders [1].
The late life depression is an important public health problem, because is associated with increased risk of morbidity, decreased physical, cognitive and social functioning, and greater self-neglect, all of which are in turn associated with increased mortality. Clinically significant depressive symptoms are present in approximately 15% of community-dwelling older adults [2]. Especially in the elderly, the multidimensional approach allows a larger and more complete evaluation of the patient, of him sociological, biological and psychological dimensions, in their own dynamic assembly, like a total human [3].
The most of the literature showed that changes in serum lipids levels are correlated with several psychopathological conditions like schizophrenia, depression, posttraumatic stress disorder and other anxiety disorders, aggressiveness, impulsiveness and suicide. Moreover, it has been suggested that total cholesterol might be useful biomarker for detecting the risk of suicide and a prognostic value in managing severely depressed patients [4,5]. However, involvement of serum cholesterol in pathogenesis of psychiatric disorders has been doubted by few authors on the basis of their studies that have not found any correlation between serum cholesterol and psychiatric disorders [6]. Other results do not support the use of biological indicators such as serum lipids either to predict the psychiatric outcome or any association between the two. There are very few studies showing no significant association between low lipid profile and psychiatric disorders [7].
The study conducted by Ancelin et al., [8] observed a relationship between reduced LDL-cholesterol level in plasma and decreased brain cell membrane cholesterol, which in consequence might lead to changes in density and functioning of serotoninergic transporters or receptors. Other researcher in several studies [9,10] noted statistically significant lower levels of HDL-cholesterol in patients with chronic depression than in control group and also higher atherogenic indices than control group. Community studies have shown that 25% of the elderly report depressive symptoms and 1% to 9% meet the criteria of having major depression [11,12]. Also, Morgan et al., [13] reported that depressive symptomatology was 3 times more common in elderly persons with lowered cholesterol levels, study confirmed by Aijanseppa et al., [14]. However, studies linking the lipid profile to depression are inconsistent, from direct to inverse or no correlation. Nevertheless, MD is clearly associated with increased atherogenicity. Taking into account all the above, the aim of the study was to investigate a possible association between lipid changes (by lipid serum panel and atherogenic index), cardiovascular risk (by HeartScore) and mood disorders appearance in older patients.
Methods
Patients and procedures
Observational cross-sectional study comprised a number of 242 patients over 55 years old, hospitalized in ”Ana Aslan” National Institute of Gerontology and Geriatrics; 134 with MD vs. 108 control group. The subjects’ selection for the study was made respecting the inclusion and exclusion criteria that were initially set.
Inclusion criteria: Patients that were diagnosed with different mood disorders based on International Classification of Mental and Behavioural Disorders, 10th edition [15]. According to international diagnostic criteria (DSM-5, ICD-10), an independent team of clinicians with extensive experience established the clinical diagnosis based on data sets from gerontopsychiatric and neurological clinical examinations and laboratory investigations. Investigation, psychological assessment of patients and assessing the results imposed selecting and applying specific gerontopsychological methods to achieve the intended purpose. We take into account only the presence/absence of MD.
Exclusion criteria: Patients with co-morbid conditions which may affect the values of the laboratory parameters of the study: like hormone-related disorders, diabetes mellitus, cardiovascular diseases, stroke, acute and chronic inflammatory state, neoplasia, and liver dysfunction.
Study has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki). Written informed consent was obtained from all the study participants prior to their enrollment. For assessing the cognitive function of patient it has been used the screening test MMSE - Mini Mental State Examination. Any score equal or greater than 24 points (out of 30) indicates a normal cognition functioning [16].
For depression assessment it has been used Geriatric Depression Scale - Long Form (GDS-LF), with 30 items [17]. This test contains no somatic items that can introduce age bias into the depression screening scale among the elderly population.
The cut-off score for GDF-LF is:
- Normal (0-9)
- Mild depression (10-19)
- Severe depression (20-30)
All the patients received physical examination, laboratory tests and comprehensive psychological evaluations. We retrieved demographic information (age, sex, ethnicity and smoking) and clinical information (height, weight, body mass index, blood pressure, glucose serum levels and a lipid panel serum). Also other clinical information was included as psychological diagnosis, medications intake and other clinical illness. Body mass index was calculated as weight divided by square of height (kg/m2).
Blood samples were taken from all participants after 12-14 hours fasting, by venopuncture into vacutainers without anticoagulant. Lipid serum profile (total cholesterol, HDL-cholesterol, LDL-cholesterol, triglycerides) was assayed using commercial laboratory kits on automated analyzer Konelab 301 SC. From lipid serum panel we computed atherogenic index (AI) as log (triglycerides/HDL-cholesterol) and its values are associated with:
- Low risk -0.3 ÷ 0.1
- Medium risk 0.1 ÷ 0.24
- High risk above 0.24
Cardiovascular risk was estimated with HeartScore, an interactive version of SCORE - Systematic Coronary Risk Evaluation - a cardiovascular disease risk assessment system initiated by the European Society of Cardiology [18].
The HeartScore risk was divided into three subclasses according to the various algorithms:
- Low risk (HeartScore<2%),
- Intermediate risk (HeartScore2% but<5%) and
- High risk (HeartScore>5%)
Statistical analysis
Data were collected and statistically analyzed through SPSS version 18.0. Graphs and tables are generated with Microsoft Word and Excel program. For quantitative values, results were expressed as means ± S.D. The general characteristics of patients were compared using Student’s “t” test for continuous variables. Pearson test was used to compare categorical variables. The relationship between lipid serum levels, HeartScore and AI was assessed using a linear regression model. The prevalence of MD according to AI respectively HeartScore risk categories was calculated by logistic regression model. The Odds Ratios (OR) and their 95% Confidence Intervals (CI) were estimated by multivariable logistic regression analyses. In all calculations, p<0.05 was considered as statistically significant level.
Results
The distribution by gender of the patients studied is: 84.36% (209) women and 13.63% (33) men. Of these 242 patients, 134 had mood disorders (14.17% men) and 108 control group (12.96% men). The mean age of the studied patients was 65.46 years (Table 1).
|
|
Mood disorders patients (n=134) |
Control (n=108) |
|
Age (years) |
65.67±6.56 |
65.25±7.17 |
|
Body mass index (kg/m2) |
27.98±5.21 |
28.08±4.37 |
|
Glycemia (mg/dl) |
103.55±30.73* |
97.57±17.31 |
|
Cholesterol (mg/dl) |
207.66±46.01 |
210.51±42.16 |
|
Triglycerides (mg/dl) |
131±67.53 |
120.64±69.34 |
|
HDL-Cholesterol (mg/dl) |
53.38±17.98* |
58.50±21.02 |
|
LDL-Cholesterol (mg/dl) |
129±43.88 |
131±41.14 |
Table 1: Baseline characteristics of the studied patients.
Results are presented as means±SD; p* < 0.05 vs. C
There were no differences in body mass index and glycemic levels are in normal range. On the contrary, there were changes in lipid parameters as low levels of: cholesterol (statistical insignificant), LDL-cholesterol (statistical insignificant) and HDL-cholesterol (p < 0.05) in MD patients vs. control (Table 1). From the point of view of atherogenic indices, many researchers believe that they could play an important role in the evaluation of the depression risk [19-21]. Our study showed that AI and HeartScore values (Table 2) are significantly increased in MD patients vs. control (p < 0.01 respectively p < 0.05). Moreover, for MD patients, the average value of HeartScore is over 2, which means an intermediate cardiovascular risk for them.
|
|
Mood disorders patients (n=134) |
Control (n=108) |
|
Atherogenic index |
0.35±0.31** |
0.27±0.31 |
|
HeartScore |
2.94±2.37* |
2.41±1.90 |
Table 2: Atherogenic status and cardiovascular risk at Mood disorders patients vs. Control.
Results are presented as means±SD; p* < 0.05 vs. C, p** < 0.01 vs. C
From the point of view of dyslipidemia, high risk AI and HeartScore is increased in MD patients (60.68% vs. 39.31% respectively 56.66% vs. 43.33%) compared to control group (Table 3). Therefore, the prevalence of dyslipidemia at MD patients increased from 42.37% in the low risk AI group to 60.68% in the high risk AI group. For HeartScore, the prevalence of dyslipidemia increased too, from 43.20% to 56.66%. Linear regression analyses revealed a significant positive correlation between AI and triglycerides (p < 0.000001); between HeartScore and triglycerides (p < 0.000001) and between AI and HeartScore (p < 0.000001) at control group. For MD patients, AI and HeartScore (Figures 1 and 2) were significantly negative correlated with HDL-cholesterol (p < 0.00001).
|
Parameters |
Mood disorders patients (%) |
Control patients (%) |
Total |
|
Cholesterol (mg/dl) 200-239 (borderline) >240 (high) |
61 (58.09) 43 (54.43) 30 (51.72) |
44 (41.90) 36 (45.56) 28 (48.27) |
(105) (79) (58) |
|
HDL-Cholesterol (mg/dl) ≤40 (low) >40 (high) |
31 (62) 103 (53.64) |
19 (38) 89 (46.35) |
(50) (192) |
|
LDL-Cholesterol (mg/dl) 130-159 (borderline) 160-189 (high) |
66 (56.89) 39 (54.92) 29 (52.72) |
50 (43.10) 32 (45.07) 26 (47.27) |
(116) (71) (55) |
|
Tryglicerides (mg/dl) 150-199 (borderline) 200-499 (high) |
94 (53.10) 23 (58.97) 17 (65.38) |
83 (46.89) 16 (41.02) 9 (34.61) |
(177) (39) (26) |
|
Atherogenic index -0.3-0.1 (low risk) 0.11-0.24 (medium risk) >0.24 (high risk) |
25 (42.37) 21 (55.26) 88 (60.68) |
34 (57.62) 17 (44.73) 57 (39.31) |
(59) (38) (145) |
|
HeartScore <2% (low risk) 2% but<5% (intermediate risk) >5% (high risk) |
35 (43.20) 82 (62.59) 17 (56.66) |
46 (56.79) 49 (37.40) 13 (43.33) |
(81) (131) (30) |
Table 3: Prevalence of dyslipidemia among Mood disorders patients vs. Control.
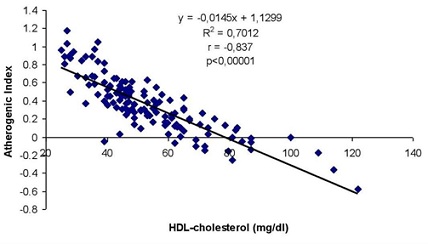 Figure 1: Correlation between Atherogenic Index and HDL-cholesterol at MD patients.
Figure 1: Correlation between Atherogenic Index and HDL-cholesterol at MD patients.
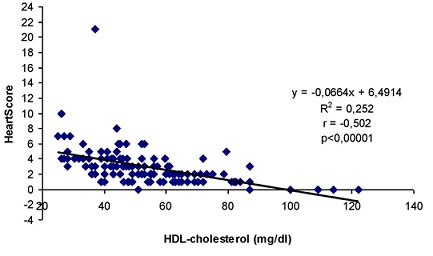 Figure 2: Correlation between HeartScore and HDL-cholesterol at MD patients.
Figure 2: Correlation between HeartScore and HDL-cholesterol at MD patients.
Also, we found a positive significant correlation between AI and HeartScore (Figure 3) at MD patients (p < 0.00001).
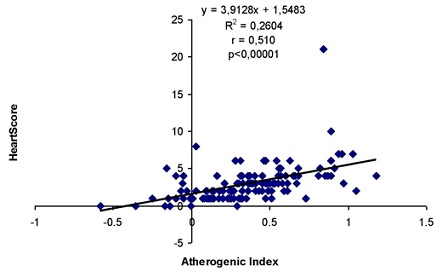 Figure 3: Correlation between Atherogenic Index and HeartScore at MD patients.
Figure 3: Correlation between Atherogenic Index and HeartScore at MD patients.
Multivariate logistic regression analysis showed that, compared to low risk, patients with high AI had 2.00-fold risk for MD. The 95% confidence interval of the odds ratios [OR 2.00, 95% CI: 1.10-3.63; p=0.022] indicates that odds of MD are significantly higher for the patients with high AI compared to low AI group. Also, patients with high HeartScore were 2.09 times likely to have MD (OR 2.09, 95% CI: 1.21-3.58; p=0.006). AI test has 81.34% sensibility and specificity 31.48%, respectively HeartScore test a sensibility of 73.88% and specificity 42.59%. Longitudinal studies are needed to confirm whether these indices with discriminatory power maintain their prognostic capacity in long term.
Discussion
In our study, we found that patients with MD have:
- Significant low HDL-cholesterol
- Increased atherogenic index
- HeartScore was raised and revealed an intermediate cardiovascular risk
- Patients with high atherogenic index had 2.00-fold risk for MD and patients with high HeartScore were 2.09 times likely to have MD too
It is known that high cholesterol is associated with cardiovascular diseases, in contrast to low cholesterol that could be involved in some medical conditions, such as cancer, depression and anxiety. Jia et al., [22] suggest that serum lipid profile may be directly linked to self-rated depression and cognitive performance. Some researchers theorize that low levels of cholesterol alter brain chemistry, enhancing the risk of depression due to the neuronal dysfunction [10,23]. Similar to our findings, several studies reported that low serum levels of HDL-cholesterol are associated with cognitive impairment and depressive symptomatology in elderly patients [11,13,14]. Also, Hui et al., [24] found that serum HDL-cholesterol levels were positively correlated with cognitive function in patients with bipolar disorders, which suggests that abnormal serum HDL-cholesterol levels may influence cognitive function in patients with bipolar disorders. The finding of a positive association between low levels of cholesterol and depression symptomatology is in agreement with a number of studies [19,25,26].
Some hypotheses have been advanced to explain the relationship between cholesterol and depressed mood. One hypothesis [27] is that the decreased concentration of esterified cholesterol might be connected with the defect of chromosome 16. Other several studies presumed that decrease of cholesterol in the serum may lead to a decrease in the content of membrane cholesterol in the brain, decrease in microviscosity and availability of protein serotonin membrane receptors. This results in smaller serotonin uptake from the blood and smaller serotonin concentration in brain cells [5,28-30].
Also, some researchers suggest another hypothesis that oxLDL activate the immune response of T cells and as a result the production of IL-2 increases. This reaction leads to a decrease in melatonin secretion in the pineal gland, which in turn leads to depression symptoms and suicidal thoughts [31]. So, it is very important to establish lipid and lipid fraction levels at which the risk of developing MD becomes significant. Several biological changes influence the incidence of cardiovascular diseases in depression and studies showed a higher frequency of cardiovascular risk factors among patients with depressive disorders, which can also explain the higher incidence of cardiovascular events [32,33]. Kalelioglu et al., [29] indicate that AI may be more useful to identify individuals with bipolar disorders at high risk for cardiovascular diseases than absolute lipid parameters.
Since there is a correlation between age, MD and high risk for cardiovascular events, any abnormal changes in lipid status of older patients with MD should be notice, to reduce their cardiovascular risk. Low serum lipid concentration, according to the results of this study, seems to be an important factor for the occurrence and persistence of MD. Increased cardiovascular risk among individuals with depression is multifactorial and requires several strategies towards cardiovascular risk reduction. Therefore, further investigations will help clarify the pathophysiology of MD in late life and promote more effective therapeutic strategies.
Some limitations should also be considered. Firstly, psychiatric diseases, both rare and common should be studied for longer duration to know more about its association with lipid profile. Second, potential cofounders, such as lifestyle - smoking, low or no physical activity, dietary habits, also obesity and social factors - low occupational status, low income, were not considered, therefore, residual confounding may exist in the multivariable logistic regression analyses. Third, we are not taking into account the degree of MD, only the presence/absence of its.
Conclusion
There is definitively a strong association between lipid profile, HeartScore and MD. Even if we cannot provide a clear conclusion, the results of our investigation suggested that serum lipids and atherogenic index could be future biomarkers for MD development, enhancing their value for prevention, diagnostic and therapeutic purposes. Furthermore, future studies should take into account the link between atherogenic index, MD and low-lipid medication. We suggest that properly regulating the lipid levels, through diet and/or secondary risk factors, and/or adjusting lipid-lowering medication may be one of MD’s treatment pathways in older patients. On the other hand, treating MD patients who have high atherogenic index and HeartScore it might help reduce cardiovascular risk and raise the quality of life.
Author Contributions
All authors have contributed equally to the article. All authors read and approved the final manuscript for submission.
Acknowledgment
This work was supported by the Research Project no. 691/12.08.2015 IAFR and no. 10413/1.09.2015 NIGG named “Quantitative and qualitative study on successful aging. A Psycho-Socio-Medical Approach on Third Age” (2016-2018), elaborated on the basis of Convention no. 551/17.07.2015 and no. 7079/18.06.2015 between Institute of Anthropology “Francisc I. Rainer” of the Romanian Academy and “Ana Aslan” National Institute of Gerontology and Geriatrics, Bucharest. Project managers: Rada C. (IAFR) and Draghici R. (NIGG).
Funding
This study did not receive any direct funding.
Disclosure of Interest
The Authors declares that there is no conflict of interest.
Availability of Data and Materials
The dataset used and analysed during the current study is available from the corresponding author on reasonable request.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Commission of IAFR (no. 153/01.03.2016).
Informed Consent Statement
Informed consent was obtained in written form from all participants involved in the study.
References
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders (5thedn) DSM-5TM. American Psychiatric Association, Arlington, USA.
- Blazer DG (2003) Depression in late life: Review and commentary. J Gerontol A Biol Sci Med Sci 58: 249-265.
- Draghici R (2015) The Clinical Geropsychology - the Role of the Psychologist in Geriatrics. In: Ciobanu A, Popa C (eds.). Psychiatry and Psychopathology - Practical Application. LAP LAMBERT Academic Publishing, Saarbrucken-Deutschland, Germany.
- Perez-Rodriguez MM, Baca-Garcia E, Diaz-Sastre C, Garcia-Resa E, Ceverino A, et al. (2008) Low serum cholesterol may be associated with suicide attempt history. J Clin Psychiatry 69: 1920-1927.
- Shrivastava S, Pucadyil TJ, Paila YD, Ganguly S, Chattopadhyay A (2010) Chronic cholesterol depletion using statin impairs the function and dynamics of human serotonin(1A) receptors. Biochemistry 49: 5426-5435.
- Ergün UG, Uguz S, Bozdemir N, Güzel R, Burgut R, et al. (2004) The relationship between cholesterol levels and depression in the elderly. Int J Geriatr Psychiatry 19: 291-296.
- John S, Dharwadkar K, Motagi MV (2014) Study on association between lipid profile values and psychiatric disorders. J Clin Diagn Res 8: WC04-WC06.
- Ancelin ML, Carrière I, Boulenger JP, Malafosse A, Stewart R, et al. (2010) Gender and genotype modulation of the association between lipid levels and depressive symptomatology in community-dwelling elderly (the ESPRIT study). Biol Psychiatry 68: 125-132.
- Lehto SM, Hintikka J, Niskanen L, Tolmunen T, Koivumaa-Honkanen H, et al. (2008) Low HDL cholesterol associates with major depression in a sample with a 7-year history of depressive symptoms. Prog Neuropsychopharmacol Biol Psychiatry 32: 1557-1561.
- Lehto SM, Niskanen L, Tolmunen T, Hintikka J, Viinamäki H, et al. (2010) Low serum HDL-cholesterol levels are associated with long symptom duration in patients with major depressive disorder. Psychiatry Clin Neurosci 64: 279-283.
- Dimopoulos N, Piperi C, Salonicioti A, Psarra V, Mitsonis C, et al. (2007) Characterization of the lipid profile in dementia and depression in the elderly. J Geriatr Psychiatry Neurol 20: 138-144.
- Broncel M, Serejko-Banas K (2016) Is there a link between cholesterol level and the risk of developing depression? Open Medicine J 3 : 352-361.
- Morgan RE, Palinkas LA, Barrett-Connor EL, Wingard DL (1993) Plasma cholesterol and depressive symptoms in older men. Lancet 341: 75-79.
- Aijänseppä S, Kivinen P, Helkala EL, Kivelä SL, Tuomilehto J, et al. (2002) Serum cholesterol and depressive symptoms in elderly Finnish men. Int J Geriatr Psychiatry 17: 629-634.
- World Health Organization (1992) The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. World Health Organization, Geneva, Switzerland.
- Folstein MF, Folstein SE (2005) MMSE-2: Mini-Mental State Examination (2ndedn). Manual de utilizare a testului. GOS Romania.
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, et al. (1983) Development and validation of a geriatric depression screening scale: A preliminary report. J Psychiatr Res 17: 37-49.
- De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, et al. (2003) European guidelines on cardiovascular disease prevention in clinical practice: Third Joint Task Force of European and other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of eight societies and by invited experts). Eur J Cardiovasc Prev Rehabil 10: 1-10.
- Beydoun MA, Beydoun HA, Dore GA, Fanelli-Kuczmarski MT, Evans MK, et al. (2015) Total serum cholesterol, atherogenic indices and their longitudinal association with depressive symptoms among US adults. Transl Psychiatry 5: 518.
- Nunes SO, Piccoli de Melo LG, Pizzo de Castro MR, Barbosa DS, Vargas HO, et al. (2015) Atherogenic index of plasma and atherogenic coefficient are increased in major depression and bipolar disorder, especially when comorbid with tobacco use disorder. J Affective Disorders 172: 55-62.
- Lucka A, Arabska J, Fife E, Kroc L, Soltysik BK, et al. (2017) Atherogenic Indices Are Increased in Elderly Patients with Unipolar Depression-Case-Control Analysis. Metab Syndr Relat Disord 15: 291-295.
- Jia QF, Yang HX, Zhuang NN, Yin XY, Zhu ZH, et al. (2020) The role of lipoprotein profile in depression and cognitive performance: A network analysis. Sci Rep 10: 20704.
- Rabe-Jablonska J, Poprawska I (2000) Levels of serum total cholesterol and LDL-cholesterol in patients with major depression in acute period and remission. Med Sci Monit 6: 539-547.
- Hui L, Yin XL, Chen J, Yin XY, Zhu HL, et al. (2019) Association between decreased HDL levels and cognitive deficits in patients with bipolar disorder: A pilot study. Int J Bipolar Disord 7: 25.
- Ghaemi SN, Shields GS, Hegarty JD, Goodwin FK (2000) Cholesterol levels in mood disorders: High or low? Bipolar Disord 2: 60-64.
- van Reedt Dortland AK, Giltay EJ, van Veen T, van Pelt J, Zitman FG, et al. (2010) Associations between serum lipids and major depressive disorder: Results from the Netherlands Study of Depression and Anxiety (NESDA). J Clin Psychiatry 71: 729-736.
- Maes M, Delanghe J, Meltzer HY, Scharpé S, D'Hondt P, et al. (1994) Lower degree of esterification of serum cholesterol in depression: Relevance for depression and suicide research. Acta Psychiatr Scand 90: 252-258.
- Dursun SM, Reveley MA (1996) Low serum cholesterol and serotonin receptor subtypes. Brit J Psychiatry 163: 417-418.
- Kalelioglu T, Ünalan P, Kök B, Sözen S, Yüksel Ö, et al. (2018) Atherogenic index of plasma as a cardiovascular risk marker in manic, depressive, and euthymic stages of bipolar disorder. Turk Kardiyol Dern Ars 46: 32-38.
- Katrencíková B, Vaváková M, Waczulíková I, Oravec S, Garaiova I, et al. (2020) Lipid Profile, Lipoprotein Subfractions, and Fluidity of Membranes in Children and Adolescents with Depressive Disorder: Effect of Omega-3 Fatty Acids in a Double-blind Randomized Controlled Study. Biomolecule 10:
- Penttinen J (1995) Hypothesis: Low serum cholesterol, suicide, and interleukin-2. Am J Epidemiol 141: 716-718.
- Grippo AJ, Johnson AK (2009) Stress, depression and cardiovascular dysregulation: a review of neurobiological mechanisms and the integration of research from preclinical disease models. Stress 12: 1-21.
- Nemeroff CB, Goldschmidt-Clermont PJ (2012) Heartache and heartbreak--the link between depression and cardiovascular disease. Nat Rev Cardiol 9: 526-539.
Citation: Draghici R, Opris S, Rusu A (2022) The Link between Lipid Profile, Cardiovascular Risk and Mood Disorders Appearance in Older Patients. J Gerontol Geriatr Med 8: 138.
Copyright: © 2022 Rozeta Draghici, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

