
The Perceptions of Persons with Multiple Sclerosis (MS) on the Impact of Diet and Supplements on MS Symptoms
*Corresponding Author(s):
Heather Dillon AndersonDepartment Of Physical Therapy, Division Of Nursing And Health Sciences, Neumann University, United States
Tel:+1 2155936774,
Email:andersoh@neumann.edu, hdillon.anderson@gmail.com
Abstract
Background: Currently there is no cure for persons living with Multiple Sclerosis (MS). Disease progression, and secondary symptoms, has traditionally been managed pharmacologically. Recent studies have examined the use of dietary modification and/or supplementation to manage MS, but most do not offer the perspective of persons living with MS on the impact of these interventions. The purpose of this study is (1) to determine whether persons with MS are managing their symptoms using dietary changes and/or supplementation and (2) to investigate their perceptions about the influences of these interventions on MS-related symptoms.
Methods: This survey study included many questions with open-ended “other” responses and an individual interview process. Participants included persons with MS living in the Northeast corridor of the United States, contacted though MS support groups. Data collection occurred during the summer and fall of 2017 and 2018.
Results: Dietary modification was reported by 57% of the 114 participants; supplementation by 90%. There was a significant relationship for participants using a Paleo, Mediterranean, and Gluten-free diets; as well as Vit B6, antioxidants, Vit B12, Vit C, Turmeric, Omega 3 and Probiotics, and the perception that diet/supplementation influenced MS symptoms. Most (89%) participants are willing to modify their diet and/or take a supplement if effective in managing MS. Cost was the most frequently cited barrier.
Conclusion: Most participants reported making dietary changes and/or taking supplements to manage MS symptoms and are willing to make changes if these interventions are proven effective. Additional research is warranted.
Keywords
Dietary management of MS; Multiple Sclerosis (MS); Supplementation for MS; Survey of persons with MS
Introduction
Multiple Sclerosis (MS) is an inflammatory disease affecting the central nervous system (CNS) that involves demyelination of nerves, causing disruption of communication from the brain to other regions of the body [1]. Symptoms of the disease, which include fatigue, vision impairments, paresis, pain, sexual dysfunction, bowel and bladder dysfunction, gait impairment, and decreased endurance, vary between persons with the disease and often fluctuate [2]. Currently, there is no consensus identifying the cause of MS, but experts believe it is a combination of hereditary and environmental risk factors [2,3]. According to the National MS Society, nearly one million people in the United States of America have been diagnosed with MS [4].
Currently, MS does not have a cure, interventions focus on decreasing the progression and secondary symptoms of the disease. Medical management typically includes medication, which is prescribed according to the type of MS. Persons with relapsing remitting MS are typically prescribed disease modifying agents in the form of injections, oral medication, and infusions [5]. According to Hartung et al., (2017) the cost of these medication often exceeds $70,000 per year, which often decreases compliance [6]. Furthermore, persons with other types of the disease are unable to use disease modifying agents and must use other medications, known to have increased side-effects and/or rely on secondary medications to manage the myriad of symptoms that typically accompany MS.
Because of the cost and known side-effects of MS medications, persons with MS frequently seek alternatives to manage their disease. This often includes dietary changes and/or supplementation [7]. Diet modification, including diets such as low-fat plant-based diets [8], Paleo based diets [9] and high fat diets [10], have exhibited positive impacts on MS symptoms. Some diets have been suggested to alter levels of inflammation in the body [11,12], where other diets have been suggested to repair the damaged myelin sheath that causes symptoms of the disease [10,13]. There is also some literature to supportthe use of antioxidants [14], Vitamin D [15,16] and Vitamin A supplementation for persons with MS [14].
The purpose of this study was to examine the frequency and perceptions of persons with MS using diet and/or supplementation to manage MS symptoms. This study investigated the specific diet and supplementary changes being used, their perceived impact, and the associated barriers. Based on the research reviewed on MS and diet, as well as clinical experience treating persons with MS, the research team hypothesized that the majority of persons with MS would be aware that diet may influence symptoms related to MS and the progression of the disease, but that most participants will report that they have not made significant dietary changes. Data about diet and supplement usage in persons with MS, and the impact on MS-related symptoms, may guide future use as well as additional larger studies to improve the quality of life for persons living with MS.
Materials and Methods
This study utilized a survey questionnaire (refer to Appendix A, MS Survey) with individual interviews. Prior to initiation of data collection, the study received approval (2017-13-020) from the IRB committee at Neumann University. Data collection occurred in two stages, the first included 61 subjects, ages 25-79, and took place during the summer and fall of 2017. The second occurred one year later and consisted of 53 subjects ages 25-77. The study population was a sample of convenience consisting of persons with MS living in the northeastern part of the United States. Inclusion criteria included a diagnosis of MS, and the ability to answer questions about diet and health habits. Participants were recruited through MS support groups, social media posts, and word of mouth. Once consent was granted, participants completed a questionnaire inquiring about diet, lifestyle, and health habits. Finally, individual interviews were conducted to confirm all information and discuss qualitative responses to open-ended questions.
Results
Statistical analyses were performed using SPSS software version 22 (IBM Corporation, Armonk, NY, USA). Descriptive statistics were used to analyze participant characteristics and responses to medication, lifestyle, and dietary habits. Chi square tests were used to compare dichotomous data, such as whether participants believed there is a connection between diet and MS and specific types of dietary modifications used by the participant. Independent samples t tests were used to determine relationships between continuous data, like the number of years with MS, and dichotomous findings, such as whether the participant had tried specified diets to manage their MS. In addition, all open-ended responses provided in the “other” fields was reviewed and categorized.
A total of 114 persons with MS completed all parts of the questionnaire and participated in the interview process. The age of the subjects ranged from 25-79; the mean age was 54.56, median 56, and standard deviation (SD) 11. The most common education was a bachelor’s degree (39%), followed by a high school diploma (31%), graduate degree (20%), and associates degree (11%). The majority of participants were white (75%) females (80%). The range of time that participants reported living with MS was .5 years to 38 years with a mean of 15.7 and SD 9.8. When asked which type of MS they had, most participants reported having relapsing-remitting (74%), followed by secondary-progressive (12.5%), primary progressive (10%), and clinically isolated/benign (2%) (Table 1).
|
Number of participants |
n = 114 |
|
Age range |
25-79 years of age |
|
Mean age |
57 years of age |
|
Gender identity |
80% female; 20% male |
|
Most common type of MS |
Relapsing-remitting (72%) |
|
Mean years since MS diagnosis (range) |
17 years (0.5 – 38 years) |
|
Education level |
69% college& more; 31% high school or less |
|
Used medication to manage MS |
83% |
|
Used dietary changes to manage MS |
57% |
|
Used supplementation to manage MS |
49% |
|
Used exercise to manage MS |
82% |
|
Used physical therapy to manage MS |
74% |
Table 1: Participant Characteristics.
The majority of participants reported taking MS medications (83%). In addition, physical therapy (74%), exercise (82%), dietary modification (57%) and lifestyle (23%) were reported as strategies to manage MS symptoms. During the second phase of data collection, participants (n=52) were asked about using complementary and alternative medicine (CAM) as a strategy to manage MS; 23% indicated that they did. Most participants (74%) reported that the use of management strategies other than medication were helpful.
Most participants (75%) reported that they believed diet has a connection with MS. When participants were asked which types of diets they had tried, the most common (27%) selection was not any of those listed on the questionnaire, but a variety of diets categorized as “other.” Many of the “other” choices consisted of various types of elimination diets. The gluten-free diet was the most commonly reported on the questionnaire (17.5%), followed by low sodium (16%) and low fat (10%). Less than 10% of participants reported using caloric restriction, ketogenic, and/or swank diet. The most commonly reported “other” diet was the Wahl’s diet (7) followed, by descriptions of generally improving the quality of diet by increasing vegetable consumption, decreasing sugar and processed foods. Several participants also described following a regime of intermittent fasting (Figure 1).
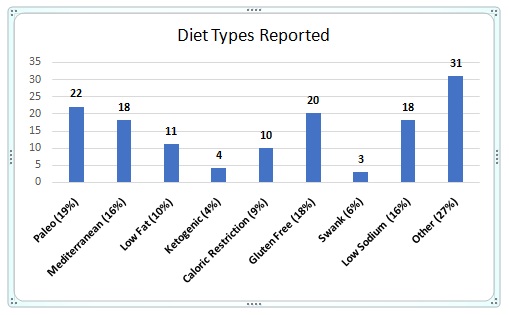 Figure 1: Diet Types Reported.
Figure 1: Diet Types Reported.
Almost all participants (90%) reported that they tried using vitamins and minerals to manage MS. Vitamin D was the most frequently reported (81%), followed by B12 (34.5%), Calcium (26.5%), Vitamin A (24%) and B6 (22%). Less than 15% of the participants reported using Vitamin E, antioxidants, and Zinc. Many of the participants (31%) also reported using an “other” type of vitamin or mineral to manage MS. The most common was Biotin (8) which is combination of vitamin B and antioxidants. Many participants also reported taking Magnesium (7), followed by use of a general multivitamin (Figure 2).
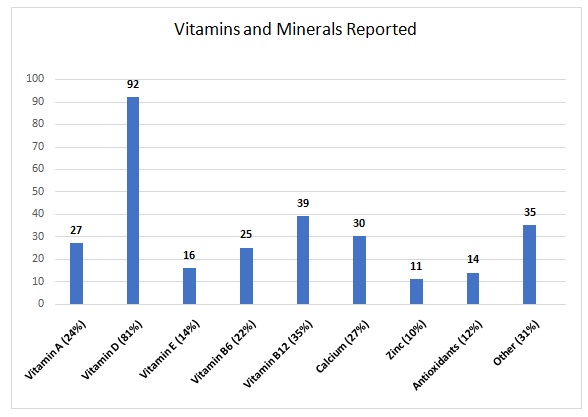 Figure 2: Vitamins and Minerals Reported.
Figure 2: Vitamins and Minerals Reported.
Slightly less than half (49%) of the participants reported using supplements to manage MS. Probiotic was the most reported supplement (30%), however this supplement was only present on the questionnaire during the second phase of data collection after several participants entered this in the “other” category during the first phase. Turmeric (22%), Omega 3 (20%), and Cranberry (11%) were also frequently reported. Less than 5% of the participants use Ginkgo Biloba, Echinacea, and/ or Valerian root. Coenzyme Q10, ginger and fish oil were reported by multiple participants in the “other” category. Furthermore, many participants reported using unusual supplements such as transfer factor, bee pollen, grade seed extract, milk thistle and Alpha-Lipoic acid. The use of marijuana and CBD oil were also reported in the “other” category (Figure 3).
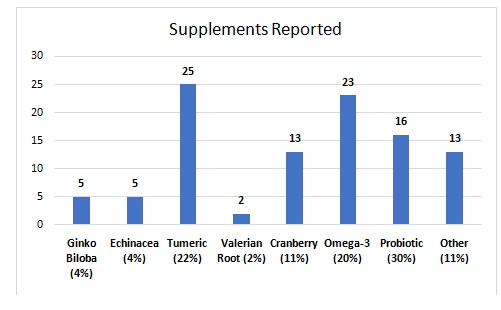 Figure 3: Supplements Reported.
Figure 3: Supplements Reported.
Slightly less than half of participants reported perceiving that diet and/or supplementation helped MS symptoms (49%). The majority (89%) reported being willing to modify their diet if there was evidence that it would help. Most (74%) were willing to participate in a larger study to investigate the connection between MS and diet. The majority (70%) of participants anticipated barriers to making dietary changes or adding supplements. The most common was cost (38%) followed by habit (28%), time (19%), knowledge (18%) and cooking (17%).Responses within the “other” category for this question often involved the psycho-social aspect of food preparation and food consumption such as cooking for family members who may not be open to dietary modification, and/or reliance on others to prepare food due to physical impairment.
There was a significant relationship between participants who tried diet to manage MS and those who believed there was a connection between MS and diet (x = 19.721, df = 1, p = 0.000). There was also a relationship between those who tried diet to manage MS and whether or not they perceived diet and/or supplementation to help MS symptoms χ2(1) = 15.192,p = 0.000).There was not a relationship between the participants age, the number of years a person had MS, or their educational level and whether or not they believed there was a connection between MS symptoms and diet and/or supplementation.
When examining those who tried specific dietary modification and whether or not they perceived diet and supplementation to influence MS symptoms, there was a significant relationship found for those who tried the Paleo diet modification (χ2(1) = 7.812,p = 0.005), Mediterranean diet modification ( χ2(1) = 3.798,p = 0.051), gluten free diet modification (χ2(1) = 6.719,p = 0.010) and for those who selected the “other” category (χ2(1) = 7.486,p = 0.006). There was not a relationship found for those who tired low fat, ketogenic, caloric restriction, low sodium and the Swank diets.
There was a significant relationship for those who used Vitamin B6 (χ2(1) = 5.283,p = 0.022), antioxidants (χ2(1) = 5.671, p=0.017), Vitamin B12 (χ2(1) = 8.837,p = 0.012), Vitamin C (χ2(1) = 9.22,p = 0.002), Turmeric (χ2(1) =5.976, p = 0.015), Omega 3 ( χ2(1) =13.407, p = 0.000), and Probiotic supplementation ( χ2(1) =4.555, p = 0.033) and whether they perceived supplementation to improve MS symptoms. There was not a relationship found for those who used Vitamins A, E, and D, Calcium, Zinc, GinkgoBilbo, St. John’s Wort, Echinacea, Valerian root, and Cranberry supplementation.
There was a significant relation found, between those who believed diet has a connection with MS and those willing to change their diet if it would help (χ2(1) =20.193, p = 0.000), as well as participants who believed there is a connection between diet and MS and those willing to participate in a study about diet and supplementation for persons with MS if there was evidence it was helpful (χ2(1) =14.031,p = .000) and between subjects who believed there is a connection between diet and MS and those willing to change diet if evidence supported it (χ2(1) =20.193,p = .000).
Discussion
Like current reports by the MS Society describing women accounting for 74 percent of persons diagnosed with MS [4] females accounted for 80 percent of participants in this study. In addition, the MS Society reports that MS is most common amongst Caucasians of northern European ancestry [4] and 75 percent of the subjects in this study identify themselves as White. Similarly, most participants had relapsing-remitting MS, the most common type reflected by data collected by the MS Society.
Consistent with our hypothesis, most participants believed that diet and supplementation may be beneficial to managing MS-symptoms. Participants reported taking a wide range of diets, vitamins, and supplements. Many of which were not listed on the survey but described within the “other” category. Furthermore, many participants described following diet and supplementation regimes that were not prescribed by a medical doctor or supported by current research.
Thirty-four percent of participants reported using the Paleo diet to manage MS symptoms. The Paleo diet eliminates all processed foods from a person’s diet, as well as grains, dairy, and legumes. Processed foods have been criticized for many years due to adverse health effects to those who eat in excess [9]. A pilot study by Wahls (2019) found a low lectin Paleolithic diet eliminating foods believed to cause inflammation was associated with favorable clinical response to MS as measured by biomarkers [17]. Another study by Sand (2018)that included a modified Paleolithic diet, as well as dietary supplements, a physical exercise program, electrical stimulation, and meditation, significantly improved fatigue in persons with secondary progressive MS [11].
Twenty-eight percent of the 56 participants in this study who modified their diet reported lowering their sodium intake. A low salt diet is believed to decrease global inflammation in the body, yielding better nerve conduction, therefore reducing the impact of MS symptoms [18]. A study by Farez et al., (2015) linked higher sodium intake to increased clinical symptoms and new enhancing lesions visible with imaging [19]. Furthermore, a study by Sand (2018) with 70 subjects, found persons with MS with medium or high sodium intake levels had clinical relapse rates 2.75- and 3.95-fold higher, respectively [11].
The Mediterranean diet is a diet consisting of low saturated fats, high in unsaturated fats, and high volume of fruits and vegetables [16]. There have been many adaptions to the Mediterranean diet, including the Wahls diet. Twenty-eight percent of subjects in this study reported trying the Mediterranean diet to decrease MS symptoms and the majority of those reporting an “other” diet type followed the Wahls diet. A study comparing the Wahls Elimination Diet and the Swank Diet, suggest that nutrients that are highly recommended within the Mediterranean based diet, may be beneficial to persons with MS [17]. However, there is no conclusive evidence that these dietary changes impact on the number of exacerbations or function.
Caloric Restriction (CR) diets are often credited with decreasing global inflammation which has been associated with MS. CRdiets have been used for quite some time and remain controversial. Some consider it to be synonymous with the newer diet trend of intermittent fasting, however caloric restriction is focused on reducing calorie intake and intermittent fasting is focused on reducing the number of meals consumed throughout the day [10,20]. Fifteen percent of our participants state that they have attempted caloric restriction diets after being diagnosed with MS. In addition, several reported using intermitting fasting to manage MS symptoms. According to Timmermans (2014) caloric restriction and dietary molecules such as polyphenols, carotenoids, vitamin D and niacin are able to counteract inflammation in MS and improve disease symptoms while other dietary compounds like sweets, alcohol, coffee and tea are more commonly associated with MS incidence [10]. A randomized-controlled pilot trial by Fitzgerald et al., (2018) with different types of CR diets, found that both intermittent and daily calorie restriction diets reduced weight in persons with MS and did not cause harm [20].
Ninety percent of participants reported using vitamins and/or supplements to manage their MS. Vitamin D was the most frequently reported (81%). The relationship between vitamin D and MS is complex and not completely understood. Correlations between latitude and MS prevalence first linked vitamin D levels to MS. There is a higher prevalence of MS in regions with less sunlight and the most common source of vitamin D is from ultraviolet radiation [21]. More recently, studies link vitamin D to suppressing an inappropriate immune response [22,23] and suggest it may help decrease levels of inflammatory cytokines hypothesized to control gene expression [22,24]. A study by Shirazi et al., (2015) suggested that vitamin D contributes to immunomodulatory protection of the brain [25]. Suboptimal levels may contribute to axonal inflammation and subsequent degeneration [26]. Some small trial studies have reported that vitamin D improves the ability of persons with early MS to generate improved regulatory T-cell suppressive function [27,28]. However, the doses used in these studies to obtain this immunoregulatory effect were much greater than the daily recommended dose [27, 28]. Furthermore, the number of subjects in these studies was small. On the other hand, larger clinical studies proving the efficacy of vitamin D for persons with MS are lacking. A Cochrane systematic review study of 12 Randomized Control trials (RCTs) by Jagannath et al., (2018) reported that vitamin D supplementation did not decrease the rate of relapses, the presence of lesions found using magnetic resonance imaging (MRI) or the incidence of serious adverse events [15]. Similar to these findings, participants in our study who used vitamin D did not perceive that it had an influence on MS symptoms.
Probiotics was the supplement most often used by study participants (49%). In addition, there was a relationship between persons taking probiotics to manage MS, and the perception that diet and supplements influence MS symptoms. Probiotics alter the composition of the microbiome, the complex environment within the gastrointestinal tract that contains microbes such as bacteria, viruses, protozoa, fungi and their associated genetic material [29]. There is growing evidence the microbiome in persons with MS is altered compared to healthy controls [29-31]. Experimental studies in induced autoimmune Encephalomyelitis (EAE), a condition that mimics MS in adults, in mice have shown that certain dysbiotic changes in the gut microbiota composition may exacerbate EAE, and positive offer protection [32,33]. A study by Tankou et al., (2018) involving high doses of probiotic supplementation for nine persons with MS, successfully increased the abundance of several microbes known to be depleted in persons with MS, and decreased the presence of several considered harmful [34].
In addition to the nine vitamins/minerals and eight supplements listed on the survey questionnaire, participants reported using 21 additional types of dietary supplements in the collective “other” categories. Most reported taking them because of advice from persons outside of their primary medical team. To investigate each is beyond the scope of this paper. However, the willingness of persons with MS to seek alternative forms of treatment to manage their disease speaks to the importance of further research to investigate their efficacy.
Contrary to our hypothesis, the majority of participants in this study did report using dietary modification (57%). This percentis higher than the 17% of respondents who reported they were currently attempting a diet to manage their MS in a survey study with 199 participants by Brenton and Goldman (2016) [7]. Like the majority of respondents in this study (74%), Brenton & Goldman reported that 91.5% of participants were interested in diet modification as way to manage MS. Similar to our conclusion, Brenton & Goldman (2016) recommend future studies, involving at least three months of dietary changes for persons with MS [7].
When planning future studies involving dietary behavior changes, it is important to understand what barriers the target population may have. In this study, the majority (70%) of respondents reported barriers to making diet and/or supplement changes, with cost reported most. A qualitative study by Barnard et al., (2020) that also investigated the barriers to dietary changes, interviewed 20 persons with MS who self-enrolled in a healthy lifestyle intervention which included dietary modification and found that social support, the ability to cook and enjoyment in food preparation facilitated dietary changes [35]. Participants reported lack of will-power, reliance on other to cook, and lack of dietary guidance from healthcare professionals as barriers to dietary modification [35].
In summary, many participants in this study perceived that dietary changes and/or or the use of certain supplements may be useful in managing MS symptoms and most have attempted to do so.Almost all expressed a willingness to adopt a specific diet or take supplements if proven to effectively manage their MS. Additional research investigating persons with MS who are actively participating in specific dietary and supplement protocols, compared to controls, with specific measurements to objectively assess outcomes is indicated. Furthermore, investigation of supplements that participants commonly reported that were not initially studied or included on the questionnaire, like Biotin, Magnesium and several others, and their effects MS should be investigated.
Acknowledgement
The authors would like to acknowledge and thank two separate groups of Neumann University Doctor of Physical Therapy Students for their essential contributions to this research study: Monique Beeko, Carrie Campbell, Melissa Choe, Ajay Mampilly, Marc Marcelin, Amanda Mikolajczyk, Shannon O’Brien, Afolabi Ogunnusi and Sara Volk-Perez.
Author’s Contribution
All the authors have accepted responsibility for the entire content of this submitted manuscript and approved submission.
Research funding: None.
Employment or leadership: None.
Honorarium: None.
Competing Interests
The authors report no declarations of interest. None of the authors have any conflicts of interests or any disclosures to report.
Financial Disclosure & Declaration of Interest
This study did not receive any financial support from entities outside of Neumann University. The authors report no declarations of interest. None of the authors have any conflicts of interests or any disclosures to report.
Appendix
References
- Belbasis L, Bellou V, Evangelou E, Ioannidis JP, Tzoulaki I (2015) Environmental risk factors and multiple sclerosis: an umbrella review of systematic reviews and meta-analyses. The Lancet Neurology 14: 263-273.
- Lazaro RT, Guerra SGR, Quiben M (2020) Umphred’s Neurological Rehabilitation. Elsevier Health Sciences, Amsterdam, Netherlands.
- Hernán MA, Olek MJ, Ascherio A (1999) Geographic variation of MS incidence in two prospective studies of US women. Neurology 53: 1711-1718.
- National MS Society (2020) Symptoms and Diagnosis. National MS Society, USA.
- Minen MT, Karceski S (2011) Multiple sclerosis and disease-modifying therapies: About multiple sclerosis. Neurology 77: 26-27.
- Hartung DM (2017) Economics and cost-effectiveness of multiple sclerosis therapies in the USA. Neurotherapeutics 14: 1018-1026.
- Brenton JN, Goldman MD (2016) A study of dietary modification: Perceptions and attitudes of patients with multiple sclerosis. Multiple Sclerosis and Related Disorders 8: 54-57.
- Yadav V, Marracci G, Kim E, Spain R, Cameron M, et al. (2016) Low-fat, plant-based diet in multiple sclerosis: a randomized controlled trial. Multiple Sclerosis and Related Disorders 9: 80-90.
- Chenard CA, Rubenstein LM, Snetselaar LG, Wahls TL (2019) Nutrient composition comparison between a modified paleolithic diet for multiple sclerosis and the recommended healthy US-style eating pattern. Nutrients 11: 537.
- Timmermans S, Bogie JF, Vanmierlo T, Lütjohann D, Stinissen P, et al. (2014) High fat diet exacerbates neuroinflammation in an animal model of multiple sclerosis by activation of the renin angiotensin system. Journal of Neuroimmune Pharmacology 9: 209-217.
- Sand IK (2018) The role of diet in multiple sclerosis: Mechanistic connections and current evidence. Current Nutrition Reports 7: 150-160.
- Storoni M, Plant GT (2015) The therapeutic potential of the ketogenic diet in treating progressive multiple sclerosis. Multiple Sclerosis International 2015: 681289.
- Choi IY, Piccio L, Childress P, Bollman B, Ghosh A, et al. (2016) A diet mimicking fasting promotes regeneration and reduces autoimmunity and multiple sclerosis symptoms. Cell Reports 15: 2136-2146.
- Holton KF, Kirkland AE (2020) Moving past antioxidant supplementation for the dietary treatment of multiple sclerosis. Multiple Sclerosis Journal 26: 1012-1023.
- Jagannath VA, Filippini G, Pietrantonj CD, Asokan GV, Robak EW, et al. (2018) Vitamin D for the management of multiple sclerosis. Cochrane Database of Systematic Reviews 9: CD008422.
- Riccio P, Rossano R (2015) Nutrition facts in multiple sclerosis. ASN Neuro 7: 1-20.
- Wahls TL, Chenard CA, Snetselaar LG (2019) Review of two popular eating plans within the multiple sclerosis community: low saturated fat and modified paleolithic. Nutrients 11: 352.
- Zostawa J, Adamczyk J, Sowa P, Sowa MA (2017) The influence of sodium on pathophysiology of multiple sclerosis. Neurological Sciences 38: 389-398.
- Farez MF, Fiol MP, Gaitán MI, Quintana FJ, Correale J (2015) Sodium intake is associated with increased disease activity in multiple sclerosis. Journal of Neurology, Neurosurgery & Psychiatry 86: 26-31.
- Fitzgerald KC, Vizthum D, Barron BH, Schweitzer A, Cassard SD, et al. (2018) Effect of intermittent vs. daily calorie restriction on changes in weight and patient-reported outcomes in people with multiple sclerosis. Multiple Sclerosis and Related Disorders 23: 33-39.
- Simon KC, Munger KL, Ascherio A (2012) Vitamin D and multiple sclerosis: epidemiology, immunology, and genetics. Current Opinion in Neurology 25: 246.
- Danner OK, Matthews LR, Francis S, Rao VN, Harvey CP, et al. (2016) Vitamin D3 suppresses class II invariant chain peptide expression on activated B-lymphocytes: a plausible mechanism for down regulation of acute inflammatory conditions. Journal of Nutrition and Metabolism 2016: 4280876.
- Niino M, Fukazawa T, Kikuchi S, Sasaki H (2008) Therapeutic potential of vitamin D for multiple sclerosis. Current Medicinal Chemistry 15: 499-505.
- Muris AH, Smolders J, Rolf L, Thewissen M, Hupperts R, et al. (2016) Immune regulatory effects of high dose vitamin D3 supplementation in a randomized controlled trial in relapsing remitting multiple sclerosis patients receiving IFNβ; the SOLARIUM study. Journal of Neuroimmunology 300: 47-56.
- Shirazi HA, Rasouli J, Ciric B, Rostami A, Zhang GX (2015) 1, 25-Dihydroxyvitamin D3 enhances neural stem cell proliferation and oligodendrocyte differentiation. Experimental and Molecular Pathology 98: 240-245.
- Sandberg L, Biström M, Salzer J, Vågberg M, Svenningsson A, et al. (2016) Vitamin D and axonal injury in multiple sclerosis. Multiple Sclerosis Journal 22: 1027-1031.
- Psujek HB, Tabarkiewicz J, Pocinska K, Stelmasiak Z, Rolinski J (2010) Immunomodulatory effects of vitamin D on monocyte-derived dendritic cells in multiple sclerosis. Multiple Sclerosis Journal 16: 1513-1516.
- Mahon BD, Gordon SA, Cruz J, Cosman F, Cantorna MT (2003) Cytokine profile in patients with multiple sclerosis following vitamin D supplementation. Journal of Neuroimmunology 134: 128-132.
- Jangi S, Gandhi R, Cox LM, Li N, Glehn FV, et al. (2016) Alterations of the human gut microbiome in multiple sclerosis. Nature Communications 7: 1-11.
- Miyake S, Kim S, Suda W, Oshima K, Nakamura M, et al. (2015) Dysbiosis in the gut microbiota of patients with multiple sclerosis, with a striking depletion of species belonging to clostridia XIVa and IV clusters. PloS one 10: 1-16.
- Chen J, Chia N, Kalari KR, Yao JZ, Novotna M, et al. (2016) Multiple sclerosis patients have a distinct gut microbiota compared to healthy controls. Scientific Reports 6: 1-0.
- Repáraz JO, Mielcarz DW, Ditrio LE, Burroughs AR, Haque SB, et al. (2010) Central nervous system demyelinating disease protection by the human commensal Bacteroides fragilis depends on polysaccharide A expression. The Journal of Immunology 185: 4101-4108.
- Lee YK, Menezes JS, Umesaki Y, Mazmanian SK (2011) Proinflammatory T-cell responses to gut microbiota promote experimental autoimmune encephalomyelitis. Proceedings of the National Academy of Sciences 108: 4615-4622.
- Tankou SK, Regev K, Healy BC, Tjon E, Laghi L, et al. (2018) A probiotic modulates the microbiome and immunity in multiple sclerosis. Annals of Neurology 83: 1147-1161.
- Barnard E, Brown CR, Weiland TJ, Jelinek GA, Marck CH (2020) Understanding barriers, enablers, and long-term adherence to a health behavior intervention in people with multiple sclerosis. Disability and Rehabilitation 42: 822-832.
Citation: Anderson HD, Leister NR, Biely SA (2022) The Perceptions of Persons with Multiple Sclerosis (MS) on the Impact of Diet and Supplements on MS Symptoms. J Altern Complement Integr Med 8: 221.
Copyright: © 2022 Heather Dillon Anderson, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

