
The Rich History and Evolution of Animal-Assisted Therapy
*Corresponding Author(s):
Allison FungMilton Academy, Milton, MA, United States
Tel:+1 781-888-8006,
Email:allisonfung55@gmail.com
Abstract
Background: Animal-Assisted Therapy (AAT) has a long and rich history of complementing traditional medicine in the treatment of many types of conditions. This type of therapy however may be poorly understood resulting in underutilization and bias. We explore the early foundations of AAT and why it should remain an important tool to be applied in patient treatment strategies.
Summary: Multiple case reports and studies have shown the benefits of AAT in the treatments of specific medical conditions, psychological disorders, physical ailments and psychosocial and developmental disabilities.
Key Messages: In conjunction with traditional therapies, AAT has been shown to augment treatment strategies and improve clinical outcomes. The paradigm shift of utilizing AAT to treat patients with conditions ranging from hypertension to Autism Spectrum Disorder (ASD), mobility disabilities to emotional well-being, Post-Traumatic Stress Disorder (PTSD) to anxiety and depression, may not only help improve what we already have in traditional medicine, but also may offer an alternative approach to patients refractory to traditional medical treatment regimens.
Keywords
Alternative therapies; Animal-assisted; Animal therapy; Treatment strategies
Introduction
Despite being utilized in many medical conditions for over several decades, Animal Assisted Therapy (AAT) is still considered a nouveau treatment strategy. History has long established the therapeutic role of companion animals as a resource for those in need. Until 1964, the terms ‘therapy animals’ or ‘animal-assisted therapy’ did not exist, and these terms were initially coined by the psychologist Dr. Boris Levinson [1]. His findings were instrumental in laying the groundwork for developing pet therapy as a form of treatment. In retrospect, many have utilized the therapeutic benefits of animals since the ninth century. There is evidence of ancient Greeks using horses to improve the overall well-being of an individual. Physicians in the 1600s applied animal therapy on patients to improve their mental and physical ailments. Even before animal companionship was not explicitly considered therapy, individuals have historically found ways to benefit from them.
In the United States, the use of animals as a form of therapy dates back to the late nineteenth century, and many influential figures have contributed to its growth and development. Historians have credited Levinson foremost for popularizing animal therapy in the US. He was the first to study the use of pets in formal therapy and published several papers on this topic. His research revealed that pets could significantly impact individuals with mental health issues and played a critical role in establishing the use of animals as a therapeutic tool. This work contributed to the concept of pet therapy as a form of medical treatment. Another key figure in this history was the psychologist Dr. Samuel Corson, an early pioneer in the field of animal therapy who worked with animals to help individuals with their mental health conditions. He believed that animals could provide a unique form of therapy that was effective and more humane than traditional methods. In the early twentieth century, he conducted groundbreaking research on this benefit and found that animals could assist individuals with a variety of mental health conditions, ranging from anxiety and depression to post-traumatic stress disorder (PTSD). Despite animal-assisted therapy’s ancillary place in medicine during the nineteenth century, patients utilizing this form of therapy found success in managing their conditions. This treatment strategy evolved over time, and provided benefits and contributions in both the fields of psychology and medicine up until the present.
Background
The history of animal-human interaction dates back thousands of years. From people using animals for practical purposes such as hunting, herding and transportation, to domesticating animals such as dogs, cats and horses for human therapeutic benefits, evidence of the animal-human relationship goes as far back as prehistoric times [2]. While this bond began as a working relationship, people eventually realized the calming effects pets had, especially to those with mental health conditions, and began incorporating animals into their daily lives. In 2017, archaeologists in Saudi Arabia found evidence of cave paintings depicting the relationship between wolves and early humans by illustrating these animals wearing leashes and collars [3]. These archeological images revealed that humans handled and trained canines even before establishing farming communities. It also suggests that humans likely first domesticated canines around 10,000 years ago (Figure 1). Dogs had many roles to play including hunting and carrying loads, but their ability to form emotional connections with humans set them apart from many other animals. Researchers believed that the moment a dog responded to a simple pat on the head with a wagging tail, it marked the beginning of a genuine human-dog relationship. In fact, many anthropologists assert the fact that dogs “co-evolved with humans,” supported by the fact of their gradual acclimation to humans. The animals themselves may have kickstarted the human-animal bond [4]. Moreover, an ethnographic study found that humans’ innate attraction to the wolves’ infantile features reinforced the human-dog connection.
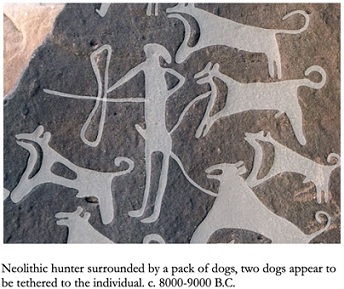 Figures: Neolithic hunter tethered to a pack of dogs. C. 8000-9000BC.
Figures: Neolithic hunter tethered to a pack of dogs. C. 8000-9000BC.
After World War I, formal training of dogs as assistance animals began to emerge in the United States and Germany, with a focus on aiding individuals with visual impairments. Following World War II, the prevalence of formal training increased for other supportive roles, such as mobility and hearing assistance. Since then, the role of service dogs has evolved, expanding to assist with a wide range of disabilities and medical conditions including epilepsy, diabetes and PTSD [5]. In parallel, there was also a rise in the integration of dogs into various working roles, including detection, hunting, herding, and protection in society. While both humans and canines co-existed and co-evolved together, this relationship has only grown stronger over time. An example can be seen, likely from the domestication process, with their heightened empathy and human-like communication ability. It has enabled them to understand human emotions and behaviors better [6].
Along with dogs, researchers found references to the physical and emotional benefits of horseback riding in writings dating back millennia. As early as 460 BC, the renowned Greek physician Hippocrates recognized the therapeutic benefits of horseback riding, referring to its "healing rhythms" [7]. He observed how the horse's natural movement impacts posture, balance, coordination, strength, and sensorimotor systems. Horses are non-judgmental, and as such, are not critical of riders. Many veterans today voiced the benefits they reaped from riding, saying that equine-assisted therapy offers them a space for recovery. Whether they were recovering from PTSD, physical injury, or mental difficulties, patients communicated that “an hour on the saddle [was] worth ten on the couch.” Surprisingly, medical and equine professionals did not take serious notice of the therapeutic benefits of horses until the 1952 Helsinki Olympic Games, where Liz Hartel, a Danish woman suffering from polio-induced paralysis, won the silver medal for dressage. Following this newfound appreciation, many countries including the United States, adopted therapeutic riding for rehabilitation purposes. These programs focused not only on the physical therapeutic goals of the patients, but also assisted with the mental development and psychosocial aspects of treatment goals. The relationship between animals and humans have undergone many transformations throughout history, but the companionship, love, and support they offer have remained constant. These connections serve as a testament to the deep bonds between our species and theirs, and provide us not only a foundational support but also room for continued animal therapy development.
Experimentation
Experimentation surrounding the field of AAT has a rich history, dating back several decades. Dr. Boris Levinson was among the first to incorporate dogs into his therapy sessions. In 1961, Levinson wrote an article titled "The Dog as a Co-Therapist," but was met with ridicule by many of his colleagues when he presented his findings. Some mocked Levinson by inquiring if the dog shared his fees and calling him the “dog’s co-therapist” [8]. The article detailed Dr. Levinson's observations about the therapeutic benefits of dogs and their use in therapy sessions. At the time, the concept of using animals as therapy was relatively new and somewhat controversial. Despite the ridicule he received, Levinson continued to advocate for the use of dogs in psychotherapy and conducted numerous groundbreaking studies to support his claims. One such paper begins with his experience on how dogs can assist patients, particularly children, who had difficulty engaging with therapists and communicating their feelings. Levinson detailed that eight years prior to writing his paper, a child exhibiting increasing withdrawal from society accidentally encountered Levinson’s dog, Jingles. While Levinson initially worried about this interaction, he came to the realization that Jingles and the child got along very well. They played together every time the child came to his office. Gradually, Levinson was allowed to participate in the play. As a result, Levinson and the child were able to create a good working relationship, and the child was eventually rehabilitated. The dog’s calming and nonjudgmental presence helped the child feel comfortable and secure, which in turn allowed them to express themselves more freely. This observation laid the foundation for the development of AAT as a legitimate therapeutic modality.
Another early experimenter in the field was Samuel Corson, a psychologist who worked with Dr. Levinson in the 1960s. Corson explored the concept of using pet animals as nonverbal communication mediators in psychotherapy sessions in institutional settings. He believed that the presence of a pet animal in therapy sessions could help break down barriers between patients and therapists and provide a way for patients to express their feelings and emotions in a nonverbal manner, coining dogs as the “social lubricant” [9]. He recognized that animals, particularly dogs, could pick up on nonverbal cues and respond in a comforting and supportive way. He noted that patients in institutional settings, such as mental hospitals, often felt isolated and disconnected from the outside world and that the presence of a pet animal could provide a sense of comfort and familiarity. Furthermore, Dr. Corson believed that psychologists and therapists could harness the pet animal's natural ability to provide comfort and support to help patients progress more quickly through their treatment. These two pioneers provided the foundation for the development of AAT as a legitimate and effective form of treatment. Their work helped to dispel the idea that therapy involving animals was unscientific, encouraging other psychologists and therapists to incorporate animals into their practices.
Forms of Therapy
There are many different forms of AAT. This alternative method has been utilized for over a millennia in the treatments of psychological and psychosocial conditions, medical and physical impairments, and for use as emotional support vehicles. Practitioners have utilized various animals for this function, from small animals such as cats and guinea pigs, to larger ones such as dolphins and barn animals [10]. By far the two most common variants of AAT include canine-assisted and equine-assisted therapy [11].
Canine-assisted therapy is a burgeoning treatment option under the umbrella of AAT with a particular focus on dogs [12]. While canine-assisted therapy was not officially endorsed during ancient times, history does depict individuals employing dogs in their everyday lives. Egyptian temples dedicated to Anubis, the dog-headed god of the dead, were scattered around Cynopolis. In those temples, people placed dogs there and trained them to lick wounds, as many believed that a dog’s saliva could heal sores and lesions [13]. In fact, many cultures today still hold on to the belief that being licked by a dog has healing properties. There is even a contemporary French saying, “langue de chien, langue de médecin,” which translates to “a dog’s tongue is a doctor’s tongue.” In the United States, approximately sixty-nine million households have a pet dog [14]. While some families utilize dogs as assistance animals, many more households consider their dog as actual family members rather than just a pet. Because of this bond, individuals are often more willing to open up to a dog without the fear of judgment or criticism as well as reducing their anxiety [15]. A study conducted by the American Heart Association in 2005 on AAT and its effects on patients’ blood pressure and anxiety levels revealed that both healthy and hypertensive patients experienced reduced blood pressure with this type of treatment, while hospitalized patients additionally experienced a decrease in anxiety levels. The researchers concluded that even short-term exposure to dogs could provide beneficial physiological and psychosocial effects [16]. We see the manifestation of this today in our modern hospital inpatient units with the usage of comfort dogs to lessen the anxiety and pain associated with medical conditions, treatment regimens, and isolation from being in the hospital.
The same can be said for people who use horses for their mental and physical well-being. Horse therapy, or equine-assisted therapies, are an umbrella term used to describe all of the equine treatments designed for people with diverse needs. This type of treatment involves direct physical interaction between a patient/client and a horse [17]. Equine therapy offers a versatile approach to address an individuals' physical and mental condition. An example of this can be seen with children and teenagers with cerebral palsy. This treatment has shown to improve their balance, coordination, motor control, posture, and behavioral tics. Furthermore, working with horses can boost cognitive skills, reduce stress, alleviate symptoms of PTSD, and address depression in some instances [18]. Clients at Lovelane, a special needs riding center located in Lincoln, Massachusetts, are exposed to supervised riding as treatment strategies for conditions ranging from autism to speech apraxia to spinal cord injury. Many whom experienced the sensations of riding a horse often expressed their enjoyment and increased happiness after their therapeutic sessions. An autistic student, around age 6, once quoted “riding a horse makes me happy… I love it.” Another student said they felt more at ease when riding horses and added, "just looking at [the horse] makes me smile” [19].
While there may be difficulties and cost constraints that come with this kind of treatment, the benefits that come from incorporating AAT into individuals’ lives far outweigh the challenges. Benefits such as an improvement in mental health, physical health, and skill improvement support a strong position for this therapy's usefulness.
Therapeutic Effects
- Psychological conditions
Levinson initially proposed an intriguing question when writing about his research: do pet owners experience a higher level of compassion and empathy than non-pet owners? This question was the basis for many researchers’ investigations [20]. They found that owning a pet increased an individual’s level of empathy towards others [21]. Furthermore, researchers discovered a heightened sense of self-esteem and a lower level of depression from people who bonded with animals [22]. As animals naturally provided a refuge for others to find comfort in, associated biochemical changes were also uncovered. Interactions with animals stimulated the release of hormones such as oxytocin, serotonin, and prolactin. These hormones resulted in stimulating increased relaxation and stress-tolerating responses, which in turn decreased symptoms of depression and anxiety [23]. In addition, owning an animal may contribute to more self-compassion and self-worth. He explains that when people care for animals, they will often increase their own value and worth because of the increased responsibility and bond they created with the animal. Thus, he proposed that companionship with animals could augment an individual’s life value even under “difficult circumstances”
Consistent AAT can lead to a variety of improved skills. Interactions with animals may improve language and conversational abilities as well as increase critical thinking. In one experiment involving a dog’s interaction with various subjects, researchers discovered increased social, communication, and cognitive rehabilitation skills resulting from the brief relationship formed between the dog and the subjects. In equine-assisted therapy, instructors noticed improvement in responsiveness and animation in individuals suffering from low responsiveness while riding. As a result of these therapeutic riding lessons, many students became more attentive and more willing to participate and follow instructions. An example of this was seen with riders becoming more vocal and taking more initiative, picking up the reins to steer the horse themselves rather than waiting for the instructor to hand over the reins.
Many clinical psychological disorders also reap the benefits of AAT. In autism spectrum disorder (ASD), some studies have shown that students interacting and playing with guinea pigs resulted in improved social skills and fewer problem behaviors [24]. With horse therapy in children with ASD, treatment regimens resulted in improved low moods by augmenting their self-confidence [25]. Moreover, not only did patients benefit from this therapy, the perceived benefits were also seen in parents of the patients as well as their therapists. Using semi-structured interviews and thematic analysis, physical, sensory and emotional benefits were noted by practitioners and parents alike [26].
- Physiologic conditions
While many people know of the mental health benefits of AAT, individuals occasionally forget the physical benefits animals provide. Researchers have noted how interactions with animals speed up injury recovery time, reduce the effects of certain medical conditions [27], alter and improve neurohormonal levels and cardiopulmonary pressures [28], and result in increased physical endurance in deconditioned individuals. This added layer of therapy potentiates what we already have in classic treatment strategy to optimize medical care. A common but serious condition associated with significant morbidity and mortality which may be treated by AAT is Cardiovascular Disease (CVD). Cardiovascular disease remains the leading cause of death within the United States and a major cause of death around the world. Despite multiple algorithms for treatment, including pharmacologic and device-based interventions, the number of cases here and around the world remain staggering. As such, factors such as hypertension, hypercholesterolemia, and obesity remain significantly high and poorly controlled, resulting in increased risk for coronary disease and its sequelae. AAT has shown to improve these factors and adds an additional layer of treatment strategy for optimization of CVD prevention. Many studies have shown this correlation of therapy and hypertension control. An Australian study by Anderson et al studied 5741 participants who attended a free wellness screening and found pet owners had a significantly lower systolic blood pressure (p=0.03) than non-pet owners even after factoring body mass index (BMI) and socioeconomic factors [29]. Moreover, an online survey of dog owners and nonowners revealed more self-reported hypertension in the nonowners’ group (OR 1.71, 95% confidence interval [CI] 1.03-2.83) [30]. Interestingly, the only randomized data set regarding pet ownership and blood pressure comes from an unpublished but presented randomized trial of 30 participants, where patients with borderline hypertension were randomized to adopt a dog from a shelter or not adopt a dog. The data revealed significantly lower blood pressure using ambulatory blood pressure monitoring in 2 and 5 months (P<0.001) in the dog adoption group versus the non-adoption group. Surprisingly, at later evaluation when all study participants had adopted dogs, these lower blood pressure findings were also seen in the initial non-adopters [31]. These findings show that animal-assisted antihypertensive benefits can be used as an added layer in the treatment of hypertension, a condition associated with CVD and major morbidity and mortality implications.
- Physical conditions
Equine-assisted therapy offers many benefits as well, including increased muscle tone, range of motion, endurance, and balance. Riding horses is an aerobic activity, and as a result, promotes increased cardio-respiratory function. Interestingly, individuals with certain conditions that may confine them to wheelchairs also reap physical benefits from horseback riding [32]. Because the horse’s motions actively move the rider’s body, oscillating movement patterns are transmitted to the patient. These motions result in stretching of soft tissue, muscle and tendons associated with wheelchair-associated contractures. Moreover, studies involving patients with multiple sclerosis revealed how the horse’s movement pattern had similarities with human gait. This similarity was exploited through riding, with continuous stimulation via voluntary and involuntary muscle contraction, resulting in increasing muscle tone and function for the rider.
Canines have also been shown to help with endurance and augment physical exertion in individuals. Investigations have suggested that daily dog walking encourages physical activity in elderly individuals by promoting increased physical activity, such as walking through different dog parks [33]. An experiment involving 5902 individuals in the US reported a positive relationship between dog walking and the amount of total walking time, showing that dog owners were more likely to walk at least 150 minutes a week compared to people who did not own dogs. This positive correlation supports the benefits of dog ownership and physical activity.
Limitations and Direction for Future Research
There are however limitations to AAT from both a research and implementation standpoint. The studies promoting this type of treatment included only limited control group trials and usually had smaller sample sizes than traditional studies. Also, it remains unclear whether long-term effectiveness persists after treatment. The cost burden associated with these type of therapies also may exclude a large portion of the population. To alleviate this, future research should focus on the standardization of animal interventions and to develop better research designs, including more control group trials and larger sample sizes, to create more impactful and objective data and findings. In addition, access to AAT should be studied between different population groups, such as high and low socioeconomical status and racial/ethnic backgrounds. This may lead to future interventions promoting health care equity utilizing this alternative therapy.
Discussion
Although Levinson did not officially coin the term “animal-assisted therapy” until the 1960s, people have recognized the therapy’s benefits throughout human history. From using animals for daily menial work to connecting with them for emotional stability, individuals have long understood the advantages of incorporating animals into various aspects of their lives, including therapy. Levinson's recognition of the therapeutic potential of animals was built on an age-old understanding of their usefulness in improving emotional well-being and assisting with work. Since then, mental health treatment has relied on AAT as an essential tool for treatment regimens. Many therapy animals exist, including dogs, horses, and even non-traditional ones such as octopi and rodents. These animals can provide emotional support, stress relief, and physical and mental health benefits to patients in a variety of settings, including hospitals, nursing homes, and schools. The enduring bond between humans and animals drives the success of AAT. Researchers have effectively documented the therapeutic benefits of animal companionship, with studies showing that therapy animals can lower blood pressure, reduce anxiety and depression, and even boost life skills. Furthermore, this therapy can aid individuals with cognitive and social deficits, providing opportunities for interaction and engagement.
The history of AAT in the United States is a testament to the transformative power of the bond between humans and animals and its importance in modern-day medicine. The increasing use of this therapy has spurred significant growth in the field, with researchers continuing to investigate new applications for therapy animals and new ways to integrate them into traditional treatment methods. AAT has proven its benefits and made significant contributions to the fields of psychology and medicine throughout the nineteenth and twentieth centuries, and it will undoubtedly continue to do so in the future.
References
- Levinson BM (1962) The dog as a 'co-therapist. University of Pennsylvania 46: 59-65.
- Seifert J (2022) A History of Our Relationship with Animals and Animal Assisted Therapy (AAT). Hawaii Island Recovery USA.
- Grimm D (2017) These may be the world's first images of dogs—and they're wearing leashes. Science.
- Pallardy R (2021) Dogs Have Co-Evolved with Humans Like No Other Species. Discover USA.
- Gee NR, Rodriguez KE, Fine AH, Trammell JP (2021) Dogs Supporting Human Health and Well-Being: A Biopsychosocial Approach. National Library of Medicine 8: 630465.
- Katayama M, Kubo T, Yamakawa T, Fujiwara K, Nomoto K, et al. (2019) Emotional Contagion From Humans to Dogs Is Facilitated by Duration of Ownership. Frontiers in Psychology 10: 1678.
- Equine Assisted Therapy (2023) Healing America's Heroes.
- Levinson BM (1982) The Future of Research into Relationships Between People and Their Animal Companions. International Journal for the Study of Animal Problems 3: 283-294.
- Wijker C, Steen SV, Spek A, Leontjevas R, Enders-Slegers MJ (2020) Social Development of Adults with Autism Spectrum Disorder During Dog-Assisted Therapy: A Detailed Observational Analysis. National Library of Medicine 17: 5922.
- Chitic V, Rusu AL, Szamoskozi S (2012) The Effects of Animal Assisted Therapy on Communication and Social Skills: A Meta-Analysis. VanFleet & FaaThompson, USA.
- American Counseling Association (2023) 8 Things You Didn't Know About Animal-Assisted Therapy (AAT). American Counseling Association, USA.
- Carapezza K (2021) Learning about the experiences of canine-assisted therapy handlers. Counseling Today, USA.
- Fine AH (2015) Handbook on Animal-Assisted Therapy: Foundations and Guidelines for Animal-Assisted Interventions. Elsevier, USA.
- Gray E (2023) US Pet Ownership Statistics 2023: How Many Americans have Pets? PetKeen, USA.
- Dodgson L (2018) People really do love dogs more than other humans, according to a new study. Business Insider, USA.
- Boe VRM (2008) Effects of Animal-Assisted Therapy on a Student with an Emotional/Behavioral Disorder. Southwest Minnesota State University, USA.
- Strongwater Farm Therapeutic Equestrian Center (2023) Benefits of Equine Therapy. Strongwater Farm Therapeutic Equestrian Center, USA.
- Good Therapy (2017) Equine-Assisted Therapy. Good Therapy, USA.
- Lincoln (2023) Interview by the author. Lincoln, USA.
- Esparza JS (1990) Personality Characteristics Associated With Pet Ownership: Validating The Theoretical Propositions Of Boris Levinson. Graduate Council of the University of North Texas in Partial Fulfillment of the Requirements, USA.
- Bhutto ZH, Hassan H (2012) Empathy as a Result of Pet Ownership. Bahria Journal of Professional Psychology 11: 32-45.
- Bhutto ZH, Hassan H (2023) Empathy as a Result.
- Husson University (2024) The Healing Power Of Animals: Benefits Of Animal-assisted Therapy. Husson University Online, USA.
- O'Haire ME, McKenzie SJ, McCune S, Slaughter V (2013) Effects of animal-assisted activities with guinea pigs in the primary school classroom. Anthrozoos 26: 10.2752.
- Kern JK, Fletcher CL, Garver CR, Mehta JA, Grannemann BD, et al. (2011) Prospective trial of equine-assisted activities in autism spectrum disorder. Alternative Therapies in Health and Medicine 17: 14-20.
- Ang CS, MacDougall FA (2022) An Evaluation of Animal-Assisted Therapy for Autism Spectrum Disorders: Therapist and Parent Perspectives. Psychol Stud 67: 72-81.
- Husson University Online (2023) The Healing. Husson University Online, USA.
- Cole KM, Gawlinski A, Steers N, Kotlerman J (2007) Animal-assisted therapy in patients hospitalized with heart failure. Am J Crit Care 16: 575-585.
- Anderson WP, Reid CM, Jennings GL (1992) Pet ownership and risk of cardiovascular disease. Med J Aust 157: 298-301.
- Lentino C, Visek AJ, McDonnell K, DiPietro L (2012) Dog walking is associated with a favorable risk profile independent of moderate to high volume of physical activity. J Phys Act Health 9: 414-420.
- Allen K (2001) Dog ownership and control of borderline hypertension: a controlled randomized trial. Presented at: 22nd Annual Scientific Sessions of the Society of Behavioral Medicine. Seattle, WA, USA.
- Lavín-Pérez AM, Collado-Mateo D, Caña-Pino A, Villafaina S, Parraca JA, et al. (2022) Benefits of Equine-Assisted Therapies in People with Multiple Sclerosis: A Systematic Review. National Library of Medicine 2022: 2022:9656503.
- Cherniack P (2014) The Benefit of Pets and Animal-Assisted Therapy to the Health of Older Individuals. Curr Gerontol Geriatr Res 2014: 623203.
Citation: Fung A, Mok P, Fung WK (2024) The Rich History and Evolution of Animal-Assisted Therapy. J Altern Complement Integr Med 10: 443.
Copyright: © 2024 Allison Fung, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

