
The Successful Management of a Breast-Feeding Type 1 Diabetic Infant
*Corresponding Author(s):
Joanna Yuet-ling TungDepartment Of Paediatrics And Adolescent Medicine, Queen Mary Hospital, The University Of Hong Kong, Hong Kong
Tel:+852 22554485,
Email:tungylj@hku.hk
Abstract
Management of infants with type 1 diabetes is challenging to both the families and the medical team. In general, they have unpredictable oral intake and activity level, limited ability to express their needs, and low insulin requirement demanding more precise adjustment. We report a breast-feeding infant with multiple food allergies and type 1 diabetes managed smoothly with insulin pump and continuous glucose monitoring system.
Keywords
INTRODUCTION
We report an infant with type 1 diabetes managed smoothly with insulin pump and continuous glucose monitoring system.
CASE REPORT
During the transition to subcutaneous insulin, great challenges were encountered. First, she had history of multiple food allergies and was still predominately breast-feeding ad lib before the diagnosis of type 1 diabetes. During her recovery, she refused all kinds of food except direct breast-feeding. In addition, her oral intake was very unpredictable. This makes estimation of carbohydrate intake extremely difficult.
She was put on continuous glucose monitoring (Smartguard™ Suspend by Sensor), afterwards and the trend of glucose readings with respect to breast-feeding duration and timing of breast-feeding was closely observed. The subcutaneous insulin was titrated accordingly, and a fair glucose profile was achieved.
Subsequently, in addition to continuous glucose monitoring, she was also transited to Subcutaneous Insulin Infusion (CSII) pump therapy (Medtronic MiniMed® 640G System). The daily insulin requirement dropped from 8 to 9 units (0.89 to 1 unit/kg/day) to 5 to 6 units (0.63 to 0.67 units/kg/day). The basal insulin ranged from 0.025 to 0.75 units per hour, contributing to around 30 % total daily insulin dose. However, some challenges were noted in the initial phase.
INSULIN SENSITIVITY FACTOR
VERY LOW BASAL RATE
VARIABLE CARBOHYDRATE CONTENT AND GLYCAEMIC INDEX IN BREAST MILK
SKIN IRRITATION AND REPEATED DISLODGEMENT
After around 2-week of adaptation, we finally managed to overcome some of these challenges. A satisfactory glucose profile was achieved (Figure 1). She is currently 2 years of age with normal development and her A1C remained at 6.5 % to 6.8 %. There was no further hospital admission related to her diabetes.
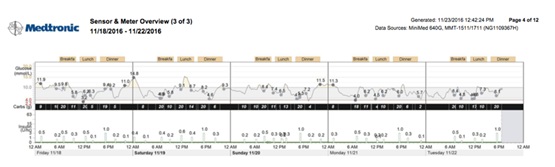 Figure 1: Good glycaemic control with the use of CGMS and insulin pump.
Figure 1: Good glycaemic control with the use of CGMS and insulin pump.DISCUSSIONS
In general, using CSII pump therapy required more vigilance especially on the technical aspects and frequent glucose monitoring than basal/bolus insulin injection regimen. However, as reported in qualitative studies, the CSII pump therapy allows more ‘freedom, flexibility, and spontaneity in daily lives’ [2], ‘no longer having to administer painful injections’, ‘fewer restrictions on the frequency, timing and carbohydrate contents of snacks and meals; and improvements in family life and their child’s glycaemic control’ [3]. In our case, the use of CSII pump therapy, together with CGMS in this case helped both the parents and the medical team to manage this infant’s unpredictable and restricted diet issues smoothly. A smaller pump bolus could be given first before meal, and further doses could be given if she ate more. In this way, even if she refused food, it was no longer an issue as the bolus given prior to meal was only a small bolus. This flexibility relieved many anxieties and potential conflicts on eating between the caretakers and the child. In addition, a more precise insulin dose could be given as bolus (increment as low as 0.025 units) conveniently without insulin dilution. With the suspend before low function, basically our patient had minimal hypoglycaemic episodes, even with such a good HbA1c level. This would not be easily achievable with basal/bolus regime of insulin injection.
In the past decade, the use of CSII pump therapy in children has increased remarkably worldwide, though there is still significant variability among countries in the use of pump technology, contributed by both reimbursement issues and expertise in pump management. There are growing evidences on the safety and better metabolic control with CSII pump therapy when compared to MDI [4-7]. Results from a multi-centered childhood diabetes registry involving more than 16 000 type 1 diabetic children showed that, both HbA1c and daily insulin dose (U/kg/d) are lower among children treated with CSII, when compared to basal/bolus regimen, after adjustment for age, gender, and diabetes duration [5]. Similarly, results from three large, transatlantic paediatric registries involving 54,410 children and adolescents also revealed lower mean HbA1c among the pump users than those receiving insulin injection therapy [6]. It has also been reported in a large prospective cohort that, the use of CSII in adolescents is associated with lower rates of microvascular complication, independent of glycemic control or social economic status [8]. To date, there is only one retrospective study on medium term outcome of CSII pump therapy among type 1 diabetic children. It included subjects who used CSII for at least 5 years and reported significantly glycaemic improvement in terms of better A1C 1 year after CSII therapy initiation; with the use of advanced pump features associated with greater improvement in HbA1c. No significant differences were observed for body mass index, insulin requirement or other adverse events and hence it was concluded that its use is safe and effective in the pediatric population [9]. However, long-term data is not available at the moment and its benefits among infants or toddlers are not well described.
Since the insulin dose of infants could be very low, this makes the in-built occlusion detection system unreliable. For example, with the Medtronic MiniMed® 640G System, the occlusion alarm would only be triggered by an average of 2.23 units of missed insulin (standard bolus) or 1.97 units of missed insulin (quick bolus). In an infant whose total daily dose is only 5 units, this alarm system would not detect insulin delivery occlusion. Therefore, it is extremely important to have close blood glucose monitoring, desirably CGMS to prevent DKA related to tubing blockage.
The prediction of insulin requirement with respect of breast-feeding was especially challenging in this case. However, with CGMS and very close communication between the mother and the medical team, it is not impossible. We could, of course, suggest changing to elemental formula for her cows and soya milk protein allergy rather than continuing with breast-feeding to minimize all these challenges. Nevertheless, we understand the benefits of breast-feeding and also respected mother’s strong wish to continue with breast-feeding. We also believe that we should try our best to facilitate our diabetic children to grow up like other ordinary children as far as possible.
Recently, the closed loop system has been shown to improve glycemic control and reduce nocturnal hypoglycemia in both young people and adults with T1DM [10]. However, the system, similar to our current system, was designed mainly for older children but not infants or toddlers, and hence the aforementioned challenges would still exist at the moment. On the other hand, with the real time CGMS, some parents might be tempted to control their children’s blood glucose level very tightly, which could potentially induce unnecessary stress and anxiety. Appropriately coaching and counseling by the medical team is needed to achieve a reasonably good metabolic control without inducing too much unnecessary pressure and frustrations to the families.
In summary, we report an infant with type 1 diabetes managed successfully with CGMS and insulin pump. The integrated system allows a more precise glycaemic control and is safe, more physiological and easier for the insulin administration. The success in management does not just lie on the technology, but also close communications and sharing of experience between the parents and the diabetic team. A multidisciplinary team with special expertise in managing young children with diabetes is essential
REFERENCES
- Schwartz DD, Wasserman R, Powell PW, Axelrad ME (2014) Neurocognitive outcomes in pediatric diabetes: A developmental perspective. Curr Diab Rep 14: 533.
- Sullivan-Bolyai S, Knafl K, Tamborlane W, Grey M (2004) Parents’ reflections on managing their children’s diabetes with insulin pumps. J Nurs Scholarsh 36: 316-323.
- Rankin D, Harden J, Noyes K, Waugh N, Barnard K, et al. (2015) Parents’ experiences of managing their child’s diabetes using an insulin pump: A qualitative study. Diabet Med 32: 627-634.
- Olsen B, Johannesen J, Fredheim S, Svensson J (2015) Danish society for childhood and adolescent diabetes. Insulin pump treatment; increasing prevalence, and predictors for better metabolic outcome in danish children and adolescents with type 1 diabetes. Pediatr Diabetes 16: 256-262.
- Szypowska A, Schwandt A, Svensson J, Shalitin S, Cardona-Hernandez R, et al. (2016) Insulin pump therapy in children with type 1 diabetes: Analysis of data from the SWEET registry. Pediatr Diabetes 23: 38-45.
- Sherr JL, Hermann JM, Campbell F, Foster NC, Hofer SE, et al. (2016) Use of insulin pump therapy in children and adolescents with type 1 diabetes and its impact on metabolic control: Comparison of results from three large, transatlantic paediatric registries. Diabetologia 59: 87-91.
- Levy-Shraga Y, Lerner-Geva L, Modan-Moses D, Graph-Barel C, Mazor-Aronovitch K, et al. (2013) Benefits of continuous subcutaneous insulin infusion (CSII) therapy in preschool children. Exp Clin Endocrinol Diabetes 121: 225-229.
- Zabeen B, Craig ME, Virk SA, Pryke A, Chan AK, et al. (2016) Insulin Pump Therapy Is Associated with Lower Rates of Retinopathy and Peripheral Nerve Abnormality. PloS One 11: 0153033.
- Mameli C, Scaramuzza AE, Ho J, Cardona-Hernandez R, Suarez-Ortega L, et al. (2014) A 7-year follow-up retrospective, international, multicenter study of insulin pump therapy in children and adolescents with type 1 diabetes. Acta Diabetol 51: 205-210.
- Kumareswaran K, Elleri D, Allen JM, Harris J, Xing D, et al. (2011) Meta-analysis of overnight closed-loop randomized studies in children and adults with type 1 diabetes: The Cambridge cohort. Diabetes Sci Technol 5: 1352-1362.
Citation: Tung JY, Sat W, Kwan W (2019) The Successful Management of a Breast-Feeding Type 1 Diabetic Infant. J Neonatol Clin Pediatr 6: 032.
Copyright: © 2019 Joanna Yuet-ling Tung, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

