
The Twisted Ovary in Infancy and Childhood - A Therapeutic Dilemma
*Corresponding Author(s):
Aniruddha D BhagwatFormer Consultant Pediatric Surgeon, Fortis Hiranandani Hospital, New Bombay, India
Email:aniruddha.bhagwat@dpu.edu.in
Introduction
Ovarian torsion is a rare gynecological emergency. The ovary twists on its ligamentous support, obstructing blood supply to the organ [1]. Simple ovarian cysts are common. True ovarian neoplasms are rare. A variety of treatment options are available like pre-natal or post-natal cyst aspiration, observation and surgery [2].
Materials And Methods
Data collected on children diagnosed with torsion of ovarian cysts over a span of 4 years was compiled from multiple hospitals and reviewed. Case files were studied for presentation, investigations and management and outcome. The diagnosis was made by imaging antenatal and post-natal ultrasound, MRI and color doppler. The patients underwent either Laparoscopic or open surgery and depending on the operative findings, either ovarian cystectomy, or oophorectomy, or fenestration and oophoropexy were performed. Patients were followed up at 3 mo, 6 mo and 1 year. Three cases of ovarian malignancy, and one case of corpus luteal cyst (all without torsion) were excluded from this study. (Figure 1 &2).
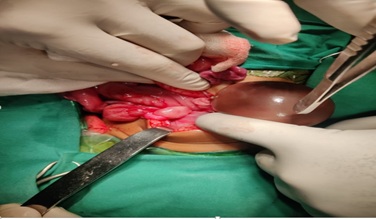 Figure 1. Left ovarian cyst torsion in a 3-month-old
Figure 1. Left ovarian cyst torsion in a 3-month-old
 Figure 2. Excised specimen of twisted left ovarian cyst in the same patient.
Figure 2. Excised specimen of twisted left ovarian cyst in the same patient.
Results
The first case was a five-day-old baby girl, born to a diabetic mother, diagnosed in a third trimester antenatal ultrasound scan as having a right ovarian cyst. There was no maternal polyhydramnios. The baby was asymptomatic at birth. Clinical examination revealed a non-tender mobile, palpable mass. A post-natal ultrasound confirmed the presence of a large right ovarian cyst extending up to the inferior surface of liver. The cyst was containing fluid and debris. A large brown colored ovarian cyst was confirmed during Laparoscopy. It had undergone a 270 degree rotation on its pedicle. The cyst was aspirated and delivered out of abdominal port site, untwisted and ovarian cystectomy was performed. Viable ovarian parenchyma was sutured and returned to the abdomen. Follow up ultrasound at 3 months, and 1 year showed a viable ovary on both the sides.
The second case was a twelve year old pubertal girl with pain in left side of abdomen and vomiting. Ultrasound showed a large left sided ovarian cyst with equivocal blood flow on color doppler. The girl underwent Laparoscopy and a congested, dusky, twisted left ovary was found. The ovary was successfully de-twisted and return of color and reduction of congestion was well appreciated. The ovary was fixed after fenestrating the cyst and de-twisting. Post op ultrasound done at 3 months revealed a viable ovary with functional cysts.
The third case was a 3 month old female who was diagnosed to have a? Ovarian? Mesenteric? Enteric duplication cyst on antenatal third trimester ultrasound. The baby was asymptomatic at birth. An MRI scan was performed which revealed a normal ovary on right side and a 5 cm sized cyst in right para-colic gutter? Mesenteric? Enteric duplication cyst. The infant was followed up. The cyst showed no signs of regression and in fact increased marginally in size at 3 months follow up. Serum AFP and beta HCG were normal for age. The child underwent a mini open laparotomy and a large left ovarian cyst was found, sitting in the right flank, twisted multiple times on its Salpinx and ligaments. The cyst was de-rotated. The cyst aspirate was hemorrhagic in color. As there was neither any discernible ovarian parenchyma identifiable, nor any pulsatile blood flow through the pedicle, and no bleeding from the cut edges, a salpingo- oophorectomy was performed on the left side. The right ovary and uterus were normal.
Discussion
The vast majority of ovarian cysts are follicular in origin. 60% of newborn ovaries demonstrate mature ovarian follicles. The normal newborn ovary has several anechoic cysts, 4-5 mm in diameter. Newborn cysts less than 2 cm in diameter are unlikely to cause problems.
FSH, LH, oestrogen and placental beta HCG all stimulate the ovarian follicle [3-5]. Infants born to diabetic mothers, Rh-iso-immunisation and pre-clampsia have higher circulating placental HCG, and are associated with a higher incidence of large ovarian cysts.
At birth beta HCG and oestrogen levels drop precipitously in the newborn. LH and FSH secretion by the hypothalamus and pituitary decreases by 4-6 months of age. Stimulation of ovarian follicle halts and simple ovarian cysts are known to involute spontaneously in 1-6 months [3,6]. Cysts more than 4-5 cm are at high risk of undergoing complications, notably torsion [3,7]. Complex, heterogeneous cysts occur more likely as a result of torsion. Cystadenomas, Teratomas, Germ cell tumors, granulosa cell tumors, ovarian carcinomas, endodermal sinus tumors are rare [3,8-10].
Simple cysts are completely anechoic with an imperceptible thin cyst wall. Complex cysts contain fluid and debris. They may be solid or multi-septate or heterogeneous. Hemorrhage, calcification, auto-amputation and free floating intra-abdominal cysts can occur. Complex cysts with fluid debris level is a hallmark of torsion.
44 to 70% antenatally diagnosed simple cysts convert to complex ones by the time of first post- natal ultrasound scan [10]. There is no co-relation between cyst size and risk of ovarian loss.
Radiological imaging including antenatal scans, ultrasound, color doppler and MRI scans are useful tools in diagnosis.
Management
The treatment remains controversial. Small, less than 4 cm simple ovarian cysts can be followed up for resolution. Large, more than 5 cm, complex ovarian cysts usually undergo torsion. In cases of torsion, initial de-torsion de-rotation is attempted. Every attempt is made to salvage and preserve the ovary. Despite ischemia, it is worthwhile to spare the ovary whenever possible. Some ovarian tissue may undergo atrophy but viable tissue will survive. The cyst can often be peeled off the surface of ovary using a moist pledget. Bleeding ovarian surface is cauterized and the edges of ovarian tissue may be approximated (not always necessary) obviously necrotic and gangrenous tissue has to be sacrificed. Complex cysts have undergone spontaneous resolution, but no viable ovarian tissue could be found on follow-up ultrasound scans in these cases. The twisted ovarian cyst is often removed for lack of identifiable ovarian tissue [4, 8, 10].
Some surgeons prefer to remove complex cysts to exclude malignancy [2,3,5,10]. Tumor markers AFP, beta HCG, are sent in all cases. Pre-operative blood samples can be stored in the refrigerator for tumor marker studies to make treatment more cost effective for the patient. MRI and CT scans need sedation and anesthesia in babies and small infants. Exposure to general anesthesia in under 2 year olds may be associated with an elevated risk of adverse neurodevelopment outcome (Table.1).
|
PROCEDURE |
MERITS |
RISK |
|
Aspiration |
Less invasive Ovary preserved |
Torsion can follow simple aspiration Malignancy may be missed Mis-diagnosis e.g. enteric cyst Re-filling and re-do maybe required. |
|
Observation & follow-up |
Spontaneous Involution may occur |
Torsion may occur Loss of ovary Intestinal obstruction |
|
Ovary sparing surgery- Cystectomy, De-roofing, fenestration, oophoropexy. |
A definitive diagnosis is obtained |
Anesthesia and neurodevelopment delay risk. Risk of loss of ovary if ischemic ovary left behind Intestinal adhesions/ obstruction. |
|
Surgery- oophorectomy |
Tissue diagnosis is obtained |
Anesthesia and neurodevelopment delay risk Loss of organ Intestinal adhesions/ obstruction |
Table 1. Shows available therapeutic options, their merits and associated risks.
Conclusion
Newborn cysts less than 2 cm in diameter are unlikely to cause problems. Small cysts less than 4 cm in size may undergo spontaneous involution. 44 to 70% antenatally diagnosed simple cysts convert to complex ones by the time of first post-natal ultrasound scan. There is no co-relation between cyst size and risk of ovarian loss. Risk of malignancy remains, albeit rare. Different modalities of treatment are available and decision needs to be tailored as per individual patients circumstances with every effort made to spare the ovary. More studies are needed to examine future fertility potential in children who have been treated for ovarian cyst torsion.
Declaration Of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the legal guardian has given his/her consent for images and other clinical information to be reported in the journal. The guardian understands that names and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil
Conflict of interest
Nil
References
- Aljohani M, Aljahany M, Elbasheer SY, Abowadaan M, Kentab O, et (2021) Pre menarchal Adolescent Female Ovarian torsion: A case of delayed diagnosis. American journal of case reports 22: e932245.
- Emmanuel S, Bargy F, Lewin F, Baron JM, Adamsbaum C, et al. (1991) Management of ovarian cyst detected by prenatal ultrasounds. European Journal of Paediatric surgery 4: 137-140.
- Mary BL, Luks FL, Feliatrautt D, Garel L, Desjardins JG, et al. (1991) Surgical indications in antenatally diagnosed ovarian cysts. Journal of Pediatric Surgery 26: 276-282.
- AnnBE, Laufer MR (2004) Foetal ovarian cysts: Incidence, Diagnosis and Journal of Reproductive Medicine 49: 329-337.
- StephenDE (2000) Ovarian masses in the Seminars in Paediatric Surgery 9: 121-127.
- Ali AM, Aikin L, Özbek S, Tireli G, Kavuncuoglu S, et al. (2010) Foetal, neonatal ovarian cysts- Their monitoring and management. Retrospective evaluation of 20 cases and review of literature. Journal Clin Res Ped Endo 2: 28-33.
- Israel M, Levy A, Katz M, Maresh AL, Glezerman M, et al. (1991) Foetal ovarian cysts: Prenatal ultrasonographic detection and post-natal evaluation and treatment. American Journal of Obstetric Gynaecology 164: 874-878.
- Ada K, Nagar H, Graif M, Ben-Sira L, Miller E, et al. (2006) Percutaneous drainage as treating of choice for neonatal ovarian cysts. Paediatric Radiology 36: 954-958.
- Jonathan CP, Billmire DF, Rescorla FJ, Finnell SME, et al. (2014) Management of neonatal ovarian cysts and its effect on ovarian preservation. Journal of Paediatric surgery 49: 990-994.
- Newbornsurgery 4th Edited by Prem Puri. CRC Press.
Citation: Bhagwat AD, Bendre PS, Shimpi A, Jadhav P (2022) The Twisted Ovary in Infancy and Childhood - A Therapeutic Dilemma. J Neonatol Clin Pediatr 9: 097.
Copyright: © 2022 Aniruddha D Bhagwat, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

