
The Vein of Galen Aneurysmal Malformation Associated with Sinus Venosus Defect and Anomalous Pulmonary Veins
*Corresponding Author(s):
Merjema KaravdicDepartment Of Cardiac Surgery, Heart Center Sarajevo, Sarajevo, Bosnia And Herzegovina
Email:karavdic.merjema@gmail.com
Abstract
The Vein of Galen Aneurysmal Malformation (VGAM) is a rare cerebral arteriovenous shunt, which may be associated with a congenital cardiac defect. Embolisation of the VGAM is safer in infancy, even it may be undertaken in the neonatal period if necessary. This case report describes a patient with a Sinus Venosus Defect (SVD) and a VGAM and considers both the optimal timing of treatment of the two malformations.
Keywords
Cardiopulmonary bypass; Embolisation; Sinus venosus defect; Vein of Galen aneurysmal malformation
INTRODUCTION
The Vein of Galen Aneurysmal Malformation (VGAM) is a rare intracranial vascular malformation where vein of Galen is dilated in a form of sacculus that collects blood shunted from the enlarged cerebral arteries. This can lead to serious consequences as Congestive Heart Failure (CHF), respiratory failure, and pulmonary hypertension. Its association with congenital heart disease has been described. Coexistence of the heart defects with VGAM has previously been reported. Associated heart defects are usually some of the following: atrial septal defect (most often the sinus venosus type with the partially anomalous pulmonary venous drainage), coarctation of the aorta, ventricular septal defect, transposition of the great arteries, tetralogy of Fallot and atrioventricular septal defect [1].
Ultrasound is an outstanding noninvasive method for the diagnosis of VGAM in neonates as well as in utero. Information about the feeding and draining vessels as well as the patency of the VoGM can be assesed through the Color Doppler ultrasound findings. CT reveals VGAM presented as a round mass that will opacificate homogenously when contrast is administered. Finally, angiography is the gold standard for evaluating and classifying of VGAMs [2]. Symptoms can vary and they can depend on the age as well as on the anatomical angioarchitecture of malformation. There are few tools for assessing the therapeutic management of a child with VGAM. The Bicetre-score is a scoring system for the evaluation of the cardiac, cerebral, respiratory, hepatic and neurological symptoms for children with VGAM. When the score is >12 (cardiovascular and neurological symptoms are stable) the treatment is usually delayed up to the age of 5 to 6 month. Score from 8 to 12 points requires an emergency endovascular procedure [3].
Amacher and Shillito categorized signs and symptoms of presentation with age in four groups. Group I is comprised of neonates that present with high-output cardiac failure as well as the cranial bruit. Neonates with just mild heart failure and craniomegaly are describes as Group II. Group III consists of infants with craniomegaly and a cranial bruit. Group IV includes patients that present after age 3.5 years with headaches, syncope with exercise and a verified calcified mass in the pineal region [4]. The leading cause of death in newborns with VGAMs is severe high-output cardiac failure. Inside the arteriovenous shunt the resistance is low so the most of the newborn’s cardiac output is directed towards the cerebral circulation. Placenta also has low vascular resistance so it competes with the VAGM in utero. The previous statement is the reason why the manifestation of the heart failure happens usually after birth [5].
It was documented that in untreated VGAM patients the mortality among newborns with cardiac insufficiency goes to even 100%, while in infants it’s 72% [6]. Before the breakthrough of the endovascular treatment, vein of Galen malformations had fatal outcome in 90% of patients that were under 1 month of age and half of those between 1 month and 1 year [7]. With the transcatheter embolisation techniques, survival among neonates and young infants is 70-80% and cure rate is about 50%. Complications of the endovascular technique were also described and were mostly connected with the perforation of the aneurysm [8,9].
CASE PRESENTATION
A 4 year old boy was admitted to our hospital for the planned operative treatment of interatrial septal defect with partial anomalous pulmonary venous return. Our patient was prenatally suspected with the diagnosis of vein of Galen aneurysmal malformation. Physical examination at birth also revealed a cardiac murmur. Echocardiogram showed a large sinus venosus Atrial Septal Defect (ASD), with Partial Anomalous Pulmonary Venous Return (PAPVR). Postnatally, magnetic resonance imaging confirmed the diagnosis of aneurysmal malformation. Seizures were noted once and were treated with phenobarbitone. On day 42 after birth, patient underwent endovascular intervention for Galen aneurysm as well as the reintervention at 2 years of age.
The first procedure was the partial embolization of the galenic fistula. Diagnostic DSA under general anesthesia was performed first: The aneurysm was found to fill through numerous anterior and posterior choroidal arteries. After selective catheterization of the choroidal and pericallosal arteries, the fistule-arteries with the galenic vein were embolized. During the second procedure, a significant reduction in flow through the fistula was found. Smaller choroidal arteries that feed the fistula are also found and were excluded from circulation by catheterization. CT after the procedure shows subarachnoid hemorrhage that is absent on CT after 15 minutes.
At 4 years of age, child underwent MRA and MR DSA of the brain. Neurosurgical team concluded that the Galenic vein aneurysm was excluded from the circulation, and that the neurosurgical treatment was completed. On admission, child was without neurological abnormalities. Regarding the cardiac status, our patient tolerated physical load, without fatigue or other ailments, except for a weaker appetite and weight gain. No cardiac therapy was included preoperatively. Echocardiogram on admission showed dilatation of the right heart cavities, anomalous inflow of the upper right pulmonary vein in superior caval vein as well as the ASD sinus venosus type with diameter about 14 mm. Intraoperatively we found the slightly enlarged right cavities along with the satisfactory heart contractility. Upon opening of the right atrium, two pulmonary veins with abnormal inflow were detected - one opened into the VCS and the other into the right atrium immediately adjacent to the ASD type sinus venosus superior. We redirected the two pulmonary veins by tunneling them into the left atrium with autologous pericardial patch and closed atrial septal defect. Postoperative course went without any complications. Child was discharged home on the fifth postoperative day (Figures 1-5).
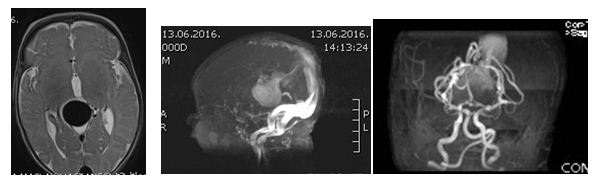 Figure 1: Magnetic resonance images before treatment.
Figure 1: Magnetic resonance images before treatment.
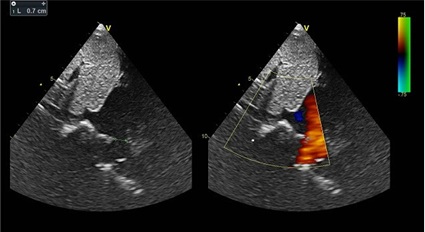 Figure 2: Transthoracic echocardiographic view of sinus venosus type of atrial septal defect.
Figure 2: Transthoracic echocardiographic view of sinus venosus type of atrial septal defect.
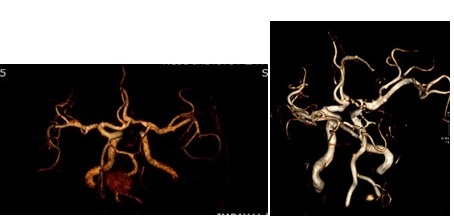 Figure 3: Magnetic Resonance Angiography (MRA) maximal intensity projection images after treatment.
Figure 3: Magnetic Resonance Angiography (MRA) maximal intensity projection images after treatment.
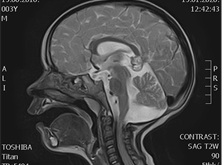 Figure 4: Magnetic resonance / sagittal / view after treatment.
Figure 4: Magnetic resonance / sagittal / view after treatment.
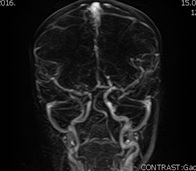 Figure 5: Magnetic Resonance Digital Subtraction Angiography (MR DSA) after treatment.
Figure 5: Magnetic Resonance Digital Subtraction Angiography (MR DSA) after treatment.
DISCUSSION
In this case we report a 4 year old boy with congenital heart anomaly - interatrial septal defect with partial anomalous pulmonary venous return that was surgically treated in our hospital. Earlier, our patient underwent two endovascular interventions due to the prenatally diagnosed vein of Galen aneurysmal malformation. VAGM is also known as the “Gordon knot” of brain s vascular system. Endovascular therapy with embolization is the most popular treatment option and it usually requires several procedures [10,11].
Association of VAGM and congenital heart defects is rare but previously described in literature. It is presupposed that greater return from the arteriovenous malformation to superior vena is associated with the absorption of the right horn of sinus venosus into the right atrium. This event occurs around 8th week and the vein of Galen develops between 6-11 weeks when it can already be diagnosed by ultrasound. However, it is often detected in the post natal period [12-14].
To inhance the chance of the survival and to improve quality of life after the treatment of VGAM it is also important to search for other viable lesions. Signs of atrial septal are usually non specific and can in this case be hidden by the high flow state with congestive failure and other murmurs. Luckily, echocardiography nowadays is enough sensitive and specific to recognize sinus venosus defect. In the modern era with endovascular treatment option, associated cardiac defects should be considered even further to improve life quality after VGAM occlusion.
Our case was diagnosed with sinus venosus ASD with PAPVR just after birth through the echocardiogram. Also, the physical examination at birth revealed a significant cardiac murmur. His heart defect wasn’t life-threatening for him at the time, so the heart surgery was postponed until further notice. At birth, urgency was directed towards the planning of treatment for vein of Galen aneurysm. In untreated VGAM, because of the low vascular resistance in the head, major part of left ventricular output goes toward the head. This can bring to reduced systemic blood flow, lactic acidosis, multiple organ ischemia. In diastole, the systemic perfusion is further diminished by ‘‘steal’’ to the VGAM which can cause reversed diastolic flow in the descending aorta [15].
In untreated patients, mortality is 95% in the 1st month and 33% between 1-12 months of age. Presentations in young age can comprise intracranial bleeding, myocardial ischemia, pulmonary hypertension and neurologic deficits [16]. Our patient was promptly endovascularly treated and his congenital vascular malformation left him no visible consequences. Prior to cardiac surgery, he was examined through MRA and MR DSA of the brain after which neurosurgical team concluded that the neurosurgical treatment was completed. Only after achieving stability of the nervous status, the child was planned for heart surgery.
Considering his cardiac status, we can say that cardiovascular symptoms were absent for the whole time although echocardiogram upon admission showed dilatation of right cardiac chambers. No signs of heart failure or significant volume overload were present. After the surgical correction of the congenital heart anomaly, our patient was without any neurological deficits in the following days. By the 4th year of life, both of his cardiac and cerebrovascular congenital anomalies were successfully treated and no lifelong consequences were to be seen.
CONCLUSION
We presented a case its successfully treated both brain vascular aneurysmal formation as well as the congenital heart defect. We recommend the establishment of the close follow up by the help of multidisciplinary approach, so that it can be treated by endovascular method before onset of symptoms without complications.
REFERENCES
- McElhinney DB, Halbach VV, Silverman NH, Dowd CF, Hanley FL (1998) Congenital cardiac anomalies with vein of Galen malformations in infants. Arch Dis Child 78: 548-551.
- Burch EA, Orbach DB (2015) Pediatric central nervous system vascular malformations. Pediatr Radiol 45: 463-472.
- Lasjaunias PL, Chng SM, Sachet M, Alvarez H, Rodesch G, et al. (2006) The management of vein of Galen aneurysmal malformations. Neurosurgery 59: 184-194.
- Amacher AL, Shillito J Jr. (1973) The syndromes and surgical treatment of aneurysms of the great vein of Galen. J Neurosurg 39: 89-98.
- Chevret L, Durand P, Alvarez H, Lambert V, Caeymax L, et al. (2002) Severe cardiac failure in newborns with VGAM. Prognosis significance of hemodynamic parameters in neonates presenting with severe heart failure owing to vein of Galen arteriovenous malformation. Intensive Care Med 28: 1126-1130.
- Khullar D, Andeejani AM, Bulsara KR (2010) Evolution of treatment options for vein of Galen malformations. J Neurosurg Pediatr 6: 444-451.
- Johnston IH, Whittle IR, Besser M, Morgan MK (1987) Vein of Galen malformation: Diagnosis and management. Neurosurgery 20: 747-758.
- Dowd CF, Halbach VV, Higashida RT, Fraser KW, Smith TP, et al. (1989) Endovascular Management of Vein of Galen Malformations. New Trends in Management of Cerebro-Vascular Malformation: 553-558.
- Wisoff JH, Berenstein A (1989) Interventional neuroradiology. In: Hoffman HJ, Edwards MSB (eds.). Cerebral Vascular Disease in Children and Adolescents. Williams and Wilkins, Baltimore, USA.
- Recinos PF, Rahmathulla G, Pearl M, Recinos VR, Jallo GI, et al. (2012) Vein of Galen malformations: Epidemiology, clinical presentations, management. Neurosurg Clin N Am 23: 165-177.
- Sasidharan CK, Anoop P, Vijayakumar M, Jayakrishnan MP, Reetha G, et al. (2004) Spectrum of clinical presentations of vein of galen aneurysm. Indian J Pediatr 71: 459-463.
- Purdy IB, Halnon N, Singh N, Milisavljevic V (2010) Vein of Galen arteriovenous malformation with PAPVR and use of serial B-type natriuretic peptide levels in the management: A case report and review of the literature. Cases J 3: 43.
- Patel N, Mills JF, Cheung MM, Loughnan PM (2007) Systemic haemodynamics in infants with vein of Galen malformation: Assessment and basis for therapy. J Perinatol 27: 460-463.
- Ahmad NS, Walker IA, Brew S (2008) Repair of sinus venosus defect in a patient with untreated vein of Galen aneurysmal malformation. Paediatr Anaesth 18: 548-553.
- Madhuban A, van den Heuvel F, van Stuijvenberg M (2016) Vein of Galen Aneurysmal Malformation in Neonates Presenting With Congestive Heart Failure. Child Neurol Open 3: 2329048X15624704.
- Smith T, Abbadi D, Thurlow P, Poornima I (2015) An Uncommon Presentation of a Rare Disorder - Ruptured Vein of Galen Malformation with Atrial Septal Defect. J Cardiol Curr Res 2: 00056.
Citation: Karavdic M, Halimic M, Kadic A, Pandur S, Hadzimuratovic N (2020) The Vein of Galen Aneurysmal Malformation Associated with Sinus Venosus Defect and Anomalous Pulmonary Veins. J Non Invasive Vasc Invest 5: 026.
Copyright: © 2020 Merjema Karavdic, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

