
Thermography and Orthodontics
*Corresponding Author(s):
Dr. Lucia RaimondiDentist, Via F.lli Bandiera N.1, 85017, Tolve (PZ), VAT Number: 01923070765, Tax Code: RMNLCU88H60G942H, UNIQUE CODE: 5RUO82D, Italy
Email:luciaraimondilu@gmail.com
Thermography And Orthodontics
Thermography (or thermal infrared imaging - IR imaging) is the graphic representation of the body temperature map obtained by the non contact and non invasive recording of the spontaneous infrared thermal emission of the body at the superficial level of the human body [1]. As heat is the main result from biochemical process and skin is means to its dissipation par excellence, through infrared radiations emission, thermography does nothing but captures thermal infrared emission by means of a thermal camera and shows it graphically.
Using the latest generation infrared cameras it is possible to record in real time all the changes in the thermal distribution of the skin, which are induced by physiological or environmental processes, such as the action of vasoactive substances or thermal stresses.
Functional analysis of this thermal response can be an effective instrument to gauge and to find out a number of pathologies [2-5]. The availability of images capable of reporting the precise map of the body (medical thermography) allows expanding the diagnostic capabilities in a whole series of pathologies of significant social impact. Thermography is applied in: cardiology, rheumatology, orthopedics, neurology, anesthesiology, dermatology, gastroenterology, urology, particularly in the early diagnosis of asymptomatic varicose lesions, dentistry [6-14].
In particular, in the dental field, researchers and clinicians have shown particular interest in thermography, evaluating the thermal pictures of the orofacial district in patients suffering from neuropathic facial pain, temporomandibular joint dysfunctions [15-16], craniofacial pain, atypical odontalgia, chronic neck pain [17-19].
Haddad, Brioschi and Arita, Merla at al. with their studies demonstrated as thermography provides a non invasive and functional test to identify myofascial trigger points. D’Attilio, Merla et al., tested the head-neck skin temperature in patients suffering from myofascial pain syndrome and asymptomatic people, in response to maximal voluntary clenching [20-22]. They showed that patients feeling a pain in the head-neck region, presented with a more asymmetric skin temperature’s distribution than controls. Some researches considered temperature and sensitivity variations in painful regions, in comparison with not aching, and got discordant results. Mohan Radhakrishna et al. [23] assert that regarding to myofascial pain syndrome, there isn’t an important relation between:
- Pression threshold, exerted on some upper and medium trapezius muscles’ regions and covering skin;
- Temperature variation of painful and not aching areas
Painful stimulation of the trigger points in sternocleidomastoid muscle may induce a thermal variation in the target area which may depend on the intensity of the felt referred pain [24] (figure 1).
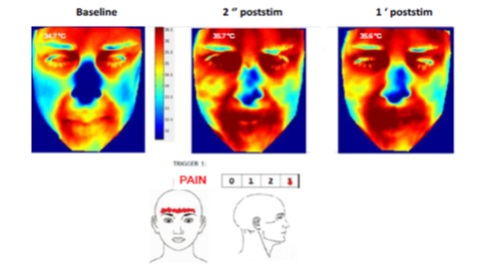
Figure 1: Painful stimulation of the trigger points in sternocleidomastoid muscle may induce a thermal variation in the target area.
Thermography also studies the effectiveness of some orthodontic treatments; Orthodontics is a branch of dentistry that deals with facial growth, development of dentition, occlusion, diagnosis and treatment of dental malocclusion.
The malocclusion is clinically characterized by single or combined dental anomalies, such as monolateral or bilateral anterior or posterior cross bite, increate or decreased over jet, covered or open bite, spacing, presence of teeth rotated, included or supernumerary or missing, etc. An orthodontic treatment treats a malocclusion to improve dental, facial aesthetics and oral function [22-23]. The rapid palate expander (ERP) iso ne of the most used orthodontic devices.
The expansion of the maxilla can and is held thanks to the rapid expander of the palate (ERP). Although this procedure is traditionally used to correct transverse discrepancies such as mono or bilateral cross bites, it is also useful for increasing the perimeter of the maxillary arch, the width of the smile, leveling the Wilson curve and increasing the patency of the patient's airways growing.
It can also be used as an anchor device. It is an orthopedic orthodontic appliance that has its roots around the middle of the nineteenth century, when Emerson H. Angell treated it for the first time. In an article published in Dental Cosmos [24] he describes its use on a fourteen-year-old to whom he claimed to have caused the opening of the median suture of the palate proving it with the appearance of an interincisal diastema. On that occasion it was formed by a central bar that acted at the level of the premolars thanks to a screw that was activated twice a day. For about 100 years it saw mixed fortunes until, starting from the 1960s, its use became routine in orthodontic practice thanks to two authors such as G. Korkhaus (1953) and A.J. Haas (1961, 1965).
As the name implies, it is a device that acts on the palate by expanding it rapidly and in its most common form it consists of a central screw with 4 arms attached to 2 or 4 bands or to an acrylic resin splint (a bite block) [25]. It acts in a short time not only by distracting the median suture of the maxilla, but also by activating the circummaxillary sutures (scalar, frontonasal and pterygopalatine zygomatico) [26-27]. With its action it directly and indirectly involves the structures connected to the maxillary bone such as the nasal cavities, the pharynx, the pterygoid process of the sphenoid and the mandible. The characteristic of ERP is the application of a high force (up to 10 kg) on the posterior dentoalveolar processes of the maxilla to which it is anchored [28-29]. Initially the dentoalveolar processes undergo a tilting movement (tipping movement of the molars), after which the force transmitted to the maxillary sutures causes a separation of the two halves of the palate along the median palatine suture (Figure 2): the final result is a variation in the width of the jawbone. The opening of the suture is clinically manifested by the appearance of an interincisal diastema, which closes spontaneously in the 2/3 months for skeletal recurrence and traction of the transseptal fibers. 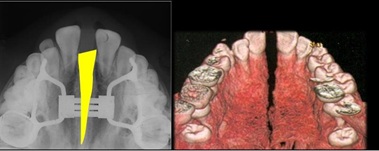
Figure 2: The two halves of the palate along the median palatine suture.
It would be interesting to evaluate the thermographic variations of the palate; before ED, after each activation of the REP, before ED, after removing REP. Thermography is certainly an excellent non- invasive tool that shows the presence or absence of variations related to biochemical processes, which can be applied to orthodontics to study the effects of orthodontic treatments.
Summary
Thermography is a non-invasive technique that allows to highlight and measure the temperature of the surface of the human body, expoiting the caloric energy emitted by the organism through the skin in the form of infrared electromagnetic radiation. Thermography is applied in various fields: industry, agriculture, medicine. Interesting and source of study is the application of thermography in medicine, especially in dentistry.
References
- Hoheisal U, Mense S, Simons D, Yu XM (1993) Appearance of new receptive fields in rat dorsal horn neurons following noxious stimulation of skeletal muscle: a model for referral of muscle pain? Neurosci Lett 153: 9-12.
- Sessle BJ, Hu JW, Amano N, Zhong G (1986) Convergence of cutaneous, tooth pulp, visceral, neck and muscle afferents onto nociceptive and non-noceceptive neurones in trigeminal subnucleuscaudalis (medullary dorsal horn) and its implications for referred pain. Pain 27: 219-235.
- Imperiali F, Tecniche termografiche. (1991) Stato dell’arte e sviluppo tecnologici. Atti del Workshop su “Stato dell’arte del rilevamento con camere termiche nella banda 8-14 micron”, Fondazione Giorgio Ronchi, Firenze.
- Merla A (2008) Developments and advances in biomedical functional infrared imaging. In: Handbook of Research on Advanced Techniques in Diagnostic Imaging and Biomedical Applications. IGI Global publication.
- Merla A, Romani GL (2007) Biomedical Applications of Functional Infrared Imaging. CRC Press.
- Biasi G, Fioravanti A, Franci A, Marcolongo R (1994) The role of computerized telethermography in the diagnostic fibromioalgia syndrome. Minerva Med 85: 451-454.
- Pappalardo A, di Girolamo F, Brignone G, Pindaro L, Caradonna E, et al. (1992) Telethermography in the diagnosis of lumbo-sciatica syndromes . Clin Ter 141: 193-197.
Citation: Raimondi L (2021) Thermography and Orthodontics. J Otolaryng Head Neck Surg 7: 60
Copyright: © 2021 Dr. Lucia Raimondi, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

