
Tinnitus Increase during the COVID-19 Pandemic in Brazil
*Corresponding Author(s):
Adriana Perez Ferreira NetoDepartment Of Otorhinolaryngology-Head And Neck Surgery, Escola Paulista De Medicina, Universidade Federal De São Paulo, 821 Botucatu St, Sao Paulo, SP, Brazil
Tel:(+55 11) 5576-4848,
Email:dri_neto@msn.com
Abstract
Objective: To assess whether tinnitus annoyance increased with the pandemic and to correlate this increase with socioeconomic, psychological and health care delivery impacts.
Methods: Cross-sectional study carried out at a tertiary referral center between August and October 2020 by applying a standard questionnaire to outpatients previously followed up for tinnitus, assessed in their first visit after lockdown.
Results: Our study group comprised 71 patients. The impacts resulting from the pandemic included: compliance with social distancing (90.1%), decrease in household income (33.8%), weight changes (52.1%), increased consumption of caffeine and/or sugar (21.1%), and tinnitus treatment interruption (19.7%). Tinnitus annoyance increased after the pandemic onset for 29 (40.9%) patients. For these 29 patients, the visual analog scale (VAS) for tinnitus annoyance increased significantly from 5.6 to 8.3 (P<.001). The tinnitus annoyance increased in 80.0% of patients with anxiety, compared to 30.4% among patients with no anxiety (P = .001). No correlation was found between the increase in tinnitus annoyance and the other parameters assessed.
Conclusion: Tinnitus annoyance increased for 40.9% of the patients included in our study. We found a significant correlation between anxiety and increase in tinnitus annoyance after the pandemic onset.
Keywords
COVID-19; Pandemic; SARS-CoV-2; Social Isolation; Tinnitus
Introduction
In December 2019, a new type of corona virus was identified in a group of adults with pneumonia of unknown etiology in Wuhan, China. The new virus was named severe acute respiratory syndrome corona virus 2 (SARS-CoV-2), and the disease caused by it was termed corona virus disease 2019 (COVID-19) [1]. The World Health Organization, concerned with the severity and quick spread of the virus, characterized COVID-19 as a pandemic in March 2020 [2].
The transmission of COVID-19 occurs mainly from person to person. In order to reduce the spread of the disease, in March 2020, several states in Brazil adopted lockdown, with the closure of non-essential services, such as restaurants, movie theaters, stores, schools, outpatient clinics etc [3]. These measures had socioeconomic, psychological and health care delivery impacts [4-7].
Tinnitus may be defined as the conscious awareness of a sound in the absence of a corresponding external auditory stimulus [8]. The prevalence of tinnitus is estimated at 11.9% to 30.3% globally [9]. Oiticica and Bittar found a prevalence of 22% in the city of Sao Paulo, and the majority (64%) reported feeling annoyed because of the tinnitus [10]. Previous studies have shown a close association between tinnitus symptoms and anxiety, depression and insomnia, with significant interference in the quality of life of affected individuals [11,12].
We hypothesized that the impacts resulting from the pandemic could cause an increase in the tinnitus annoyance. Thus, this study aimed to assess whether tinnitus annoyance increased with the pandemic and to correlate this increase with socioeconomic, psychological and health care delivery impacts.
Methods
Patient selection and study design
This is a cross-sectional study approved by the Ethics Committee of our institution (protocol 41820820.7.0000.5505), including patients previously followed up at the tinnitus outpatient clinic of a tertiary referral center. The outpatient services were suspended from March to July 2020, due to the lockdown. When outpatient visits were allowed again, patients were invited to participate in the study by answering a standard questionnaire on their first visit, which occurred between August and October of the same year. The inclusion criteria were as follows: patients with a previous diagnosis of tinnitus, regardless of etiology, and agreement to participate in the study by signing the informed consent form (ICF).The exclusion criteria were patients under 18 years of age.
Standard questionnaire applied
The following information was collected through the questionnaire: gender, age, living status, duration of tinnitus, previous treatment for tinnitus and whether this treatment had been interrupted with the pandemic, diagnosis of previous hearing loss, tinnitus characteristics, visual analog scale (VAS) of the annoyance caused by the tinnitus, comorbidities [anxiety, depression, insomnia, temporomandibular joint dysfunction (TMD)], diagnosis of COVID-19 and if hospitalization and/or use of potentially ototoxic medication had been needed, compliance with social distancing, decrease in household income, weight change, and increase in the consumption of caffeine and/or sugar.
The questionnaire included an open-ended question regarding the factors to which patients attributed the worsening of their tinnitus. These answers were then classified into 4 groups: emotional factors (such as fear, anxiety, depression, insomnia, death of relatives), socioeconomic factors (including social distancing, job loss, decrease in household income), COVID-19 diagnosis, and other health-related factors (comprising changes in eating habits and weight).Patients could attribute the worsening to more than one factor.
Hearing loss was diagnosed based on pure tone audiometry, performed prior to the pandemic, as part of the etiological investigation of tinnitus. The pure tone average (PTA) was calculated with 500-, 1000- and 2000-Hz air conduction thresholds, and PTAs ≥ 26dB HL were considered hearing loss, according to Lloyd and Kaplan's classification [13].
Regarding the tinnitus characteristics, patients were asked to define whether their tinnitus was continuous or intermittent, and to compare it to known sounds. Based on this comparison, the tinnitus was classified according to the pitch in pure tone or noise, with high or low frequency sensation, following the psychoacoustic classification of tinnitus proposed by Suzuki et al [14]. Thus, all reports of tinnitus with the characteristics of "whistle/cicada/insect" were classified as high frequency pure tone; "ship horn" as low frequency pure tone; "bee/wheezing/pressure cooker/rain" as high frequency noise; and "car engine/sea wave/airplane/waterfall" as low frequency noise [14]. Pulsatile tinnitus was considered a distinct category and was not classified as pure tone or noise. Tinnitus was deemed polytonal when the patient reported 2 or more types of tinnitus.
Tinnitus assessment
A 10 cm long horizontal line was used as the VAS (figure 1). Patients were instructed to put a cross on the straight line at the point that most precisely corresponded to their degree of annoyance due to tinnitus before the beginning of the pandemic, and another cross for the degree of annoyance after the pandemic started. The position of the cross was assigned a score between 0 and 10. The closer to 10, the greater the annoyance [15-17]. The tinnitus annoyance was therefore quantified with the VAS score and an increase in annoyance was defined as a difference between the VAS score before the pandemic and the VAS score after its onset ≥ 1.
Exceptionally, if patients assigned the maximum score (n = 10) for the annoyance both before and after the pandemic, given the impossibility of a quantitative comparison between the two similar maximal scores, a categorical evaluation was performed, i.e., these patients were asked whether they considered that their annoyance increased or not.
 Figure 1: Visual analog scale (VAS) used.
Figure 1: Visual analog scale (VAS) used.
Statistical analysis
As the normality hypothesis was excluded for all data after the Kolmogorov-Smirnov test, we used nonparametric tests: chi-square test for categorical data and Mann-Whitney test and Wilcoxon test for quantitative data comparison. Statistical analyses were performed with SPSS for Mac version 26.0 (IBM). Statistical significance was determined at the confidence level of P < .05.
Results
Clinical profile of patients and tinnitus characteristics
The study group comprised 71 patients, who answered the standard questionnaire between August and October 2020. The clinical profile of patients and their tinnitus characteristics are presented in table 1.
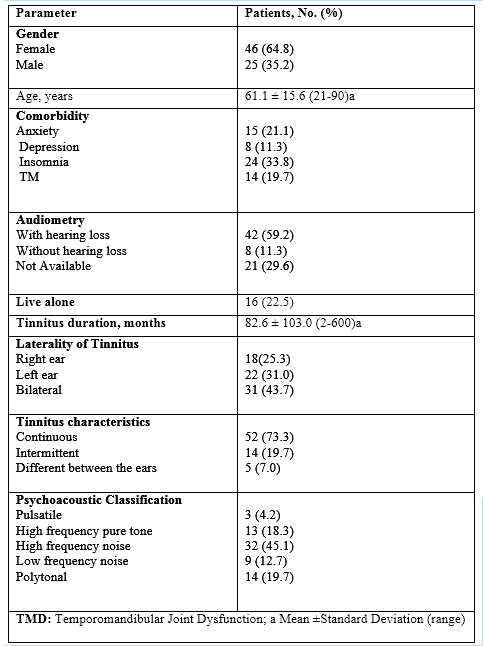 Table 1: Clinical profile of patients and characterization of tinnitus.
Table 1: Clinical profile of patients and characterization of tinnitus.
Impacts resulting from the pandemic and tinnitus assessment
In our study, 68 patients (95.8%) did not have COVID-19. The 3 (4.2%) patients who had COVID-19 did not require hospitalization, nor did they use chloroquine or hydroxychloroquine, potentially ototoxic medications [18]. All patients diagnosed with COVID-19 reported an increase in tinnitus annoyance. The remaining data regarding the impacts resulting from the pandemic are shown in table 2.
|
Parameter |
Patients, No. (%) |
|
Tinnitus treatment Interrupted treatment Maintained treatment No previous treatment |
14 (19.7) 35 (49.3) 22 (31.0) |
|
Decrease in household income |
24 (33.8) |
|
Compliance with social distancing |
64 (90.1) |
|
Weight Increased Decreased Maintained |
27 (38.0) 10 (14.1) 34 (47.9) |
|
Increased consumption of caffeine and/or sugar |
15 (21.1) |
Table 2: Impacts resulting from the pandemic.
Tinnitus annoyance remained stable after the pandemic onset for 38 (53.5%) patients, increased for 29 (40.9%) patients, and decreased for 4 (5.6%). Among the patients with increased tinnitus annoyance, 26 presented an increase in the VAS score≥ 1, while 3 had a VAS score of 10 before and after the beginning of the pandemic but reported that their annoyance increased.
For the 71 patients, the mean score assigned to the VAS after the pandemic onset was 7.4, significantly higher than the pre-pandemic score (6.5; P = .002).Likewise, for the 29 patients with an increase in tinnitus annoyance, the mean VAS score after the pandemic was 8.3, significantly higher than the mean VAS score before the pandemic (5.6; P < .001).
Concerning the factors to which patients attributed the increase of their tinnitus annoyance, from the 29 patients 9 (31.0%) reported emotional factors; 4 (13.8%) socioeconomic factors; 5 (17.2%) other health-related factors; 3 (10.3%) attributed to COVID-19 diagnosis; and 13 (44.8%) could not specify a reason. Five (17.2%) patients attributed the increase of their tinnitus annoyance to more than one factor.
The tinnitus annoyance increased in 80.0% of patients with anxiety, whereas only 30.4% of patients with no anxiety reported an increase in the annoyance (P = .001; figure 2). No significant correlation was found between the increase in tinnitus annoyance and the following parameters: gender, age, tinnitus duration, treatment interruption, depression, insomnia, TMD, social distancing, increased consumption of caffeine and/or sugar, increase, decrease or maintenance of weight, decrease in household income, and living alone.
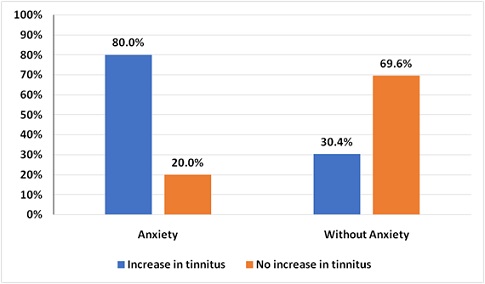 Figure 2: Relationship between anxiety and increase in tinnitus annoyance.
Figure 2: Relationship between anxiety and increase in tinnitus annoyance.
The statistical analysis of the correlation between the increase in tinnitus annoyance and the tinnitus characteristics (continuous, intermittent or different between the ears), as well as the tinnitus psychoacoustic classification, was not possible due to the low incidence of some categories.
Discussion
This study aimed to evaluate whether tinnitus annoyance increased with the pandemic and to correlate this increase with socioeconomic, psychological and health care delivery impacts resulting from the pandemic. In the literature, few studies have addressed the topic given the timeliness of the COVID-19 pandemic.
There was an increase in tinnitus annoyance after the pandemic onset for 40.9% of the patients, maintenance for 53.5%, and decrease for 5.6%. The mean score assigned to the VAS increased significantly from 6.5 to 7.4 (P = .002) for the 71 patients and from 5.6 to 8.3(P< .001) for the 29 patients. In a multicenter study by Beukes et al., 32% of patients rated their tinnitus as more bothersome after the pandemic, 67% as stable, and 1% reported an improvement [19]. An Italian study reported an increase in the Tinnitus Handicap Inventory (THI) by one-level in 75% of 16 patients assessed during the lockdown in Italy [20]. Likewise, Schlee et al. observed, on average, an increase in the THI score of 4.37 points during lockdown in Germany [21].
Considering the individual nature of tinnitus, several subjective questionnaires have been developed to assess its severity. The VAS and the THI are frequently used to identify tinnitus handicap severity [22,23]. Figueiredo et al. and Nascimento et al. found a significant correlation between THI and VAS [24,25]. Therefore, although the THI is a more comprehensive assessment, we preferred to use the VAS because it is simpler and easily assimilated by patients, being equally reliable.
The increase in tinnitus annoyance was significantly more frequent among patients with anxiety (80.0%), compared to patients with no anxiety (30.4%; P = .001). Several studies have reported an association between emotional states and tinnitus perception [26]. The prevalence of psychiatric disorders, particularly anxiety and depression, has been shown to be high among tinnitus patients, and the presence of these disorders correlate with tinnitus annoyance and severity [27]. Some theories have been described to explain these findings. Gamma-aminobutyric acid (GABA) is the main inhibitory neurotransmitter in the brain, and participates in the activity of central auditory pathways, as well as in pathways involved with anxiety [28,29]. Furthermore, neuro-imaging studies have shown that symptoms of depression and/or anxiety correlate with perceived tinnitus intensity and with volumetric changes in the brain [30].
Xia et al reported a significant increase in anxiety associated with the COVID-19 pandemic, both in terms of increased incidence and intensity.31Consistent with our results, the aforementioned study found an increase in tinnitus annoyance after the pandemic among patients with anxiety. Patients with anxiety had significantly higher THI scores than patients without [31]. We hypothesize that the lack of statistically significant correlation between tinnitus annoyance and depression is due to the small number of patients with depression in our sample.
The COVID-19 pandemic has led to several psychological, socioeconomic and health care delivery changes: compliance with social distancing (90.1%), decrease in household income (33.8%), and weight changes (52.1%), and increased consumption of caffeine and/or sugar (21.1%), and tinnitus treatment interruption (19.7%). Of the participants in the study by Beukes et al., 44% followed social distancing, 24% reported less healthy diet and 49% related financial concerns [19]. Weight changes and increased consumption of sugar could cause an increase in tinnitus. The Na+-K+-ATPase pump is a transmembrane protein found in the inner ear hair cells and generates an inward-directed Na+ gradient and an outward-directed K+ gradient. This pump activity may be compromised by glucose and insulin fluctuations, resulting in a greater amount of sodium inside the endolymph. The endolymph modification may cause tinnitus, vertigo, dizziness, aural fullness and fluctuating hearing loss [32]. In relation to caffeine, we evaluated its consumption because, although no clear relationship has been demonstrated, some studies have considered it an exacerbating factor for tinnitus [19,33,34].
In our study, with the exemption of anxiety, we did not find a significant correlation between the increase in tinnitus annoyance and the different parameters assessed. Likewise, a previous study from the literature has shown that patients who perceived frustration, grief, stress, and nervousness during the pandemic reported an increase of tinnitus-related distress; however, items with a more specific focus on the concerns arising from the pandemic, such as financial or health-related, or on the objective situation (e.g., social isolation, impact on professional activities) did not significantly correlate to tinnitus changes [21].
We theorize that this lack of significant correlation found may be explained by the small number of patients included in some variables, by the heterogeneous impact of the pandemic for each patient, and by the subjective interpretations regarding the changes caused by the pandemic. Patients may have lost their jobs, for example, but their concerns may be focused on getting a new job or on how to increase their income, with possible reduction in the attention given to the tinnitus.
The loudness of any sound depends on the contrast between this sound and the background sound. Thus, the reduction of environmental sound will lead to an increase in the perceived tinnitus loudness. In silence, tinnitus is the only sound present and the auditory system will detect it [35]. Therefore, unlike the result found in our study, we could assume that social distancing would lead to a reduction in environmental sound, with a consequent increase in the annoyance caused by the tinnitus. However, social distancing may have different meanings for each individual; it may have reduced sound exposure for those who spent most of the time on their own, whereas increased it for patients whose family members started working from home. Similarly, people who lived alone, if exposed to numerous virtual meetings held during the pandemic, for example, may have increased their exposure to sounds when at home.
Emotional, socioeconomic, and other health-related factors, as well as the diagnosis of COVID-19, were reported by patients as possible reasons for their increase in tinnitus annoyance. A systematic review found a high psychological impact of the COVID-19 pandemic among the general public, healthcare professionals, and patients with pre-existing comorbidities or COVID-19 [36]. However, although we have excluded the possibility of tinnitus increase due to ototoxic drugs or hospitalization, patients diagnosed with COVID-19 represent a potential conflict in the analysis of tinnitus increase due to possible sensorineural dysfunction caused directly by the new corona virus. In these cases, an isolated analysis of the psychological, socioeconomic and health care delivery impacts caused by the pandemic is not possible [37].
Considering the importance of the COVID-19 pandemic, it is of utmost importance to identify an increase in tinnitus annoyance and evaluate the possible factors related to that increase, in order to properly monitor and treat patients, including the possibility of preventing the tinnitus worsening. Patients with anxiety should be carefully followed up, since a significant association between anxiety and tinnitus increase has been demonstrated. As social distancing is essential to reduce the spread of the virus, remote treatment modalities should be considered. Studies have shown that cognitive behavior therapy provided via the Internet can help patients decrease the annoyance associated with tinnitus and is equally effective when compared to face-to-face therapy [38,39].
The primary limitation of this study is its cross-sectional design, which limits a better analysis of casual relationships. However, part of this limitation may have been reduced by asking the patients about their tinnitus annoyance before the pandemic. Additionally, we did not evaluate the onset of tinnitus during the pandemic, as only patients with chronic tinnitus were included in the study. Moreover, validated self-reported questionnaires addressing anxiety and depression were not used. Finally, this study comprised a small number of patients as it was conducted during a short period of time, since outpatient visits were suspended again due to worsening of the pandemic.
This study is the first to assess the changes in the perception of tinnitus annoyance arising from the COVID-19 pandemic in Brazil. Our findings have direct clinical implications, as the identification of anxiety as a factor associated with tinnitus increase may allow a more targeted treatment of patients.
Conclusions
Tinnitus annoyance increased after the pandemic onset for 40.9% of the patients evaluated. The COVID-19 pandemic has led to psychological, socioeconomic and health care delivery impacts, such as compliance with social distancing, decrease in household income, weight changes, increased consumption of caffeine and/or sugar, and tinnitus treatment interruption. We found a significant correlation between anxiety and increase in tinnitus annoyance.
Conflicts of Interest and Source of Funding
The authors disclose no conflicts of interest and this research did not receive any specific grant from funding agencies in the public, commercial, ornot-for-profit sectors.
References
- Hu B, Guo H, Zhou P, Shi ZL (2021) Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol 19: 141-154.
- https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10
- https://www.al.sp.gov.br/repositorio/legislacao/decreto/2020/decreto-64879-20.03.2020.html
- Campos JADB, Martins BG, Campos LA, Marôco J, Saadiq RA, et al. (2020) Early psychological impact of the COVID-19 pandemic in Brazil: a national survey. J Clin Med 9: 2976.
- Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, et al. (2020) The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg 78: 185-193.
- Danhieux K, Buffel V, Pairon A, Benkheil A, Remmen R, et al. (2020) The impact of COVID-19 on chronic care according to providers: a qualitative study among primary care practices in Belgium. BMC Fam Pract 21: 255.
- Wright A, Salazar A, Mirica M, Volk LA, Schiff GD (2020) The invisible epidemic: neglected chronic disease management during COVID-19. J Gen Intern Med 35: 2816-2817.
- Esmaili AA, Renton J (2018) A review of tinnitus. Aust J Gen Pract 47: 205-208.
- McCormack A, Edmondson-Jones M, Somerset S, Hall D (2016) A systematic review of the reporting of tinnitus prevalence and severity. Hear Res 337: 70-79.
- Oiticica J, Bittar RSM (2015) Tinnitus prevalence in the city of Sao Paulo. Braz J Otorhinolaryngol 81: 167-176.
- Bhatt JM, Bhattacharyya N, Lin HW (2017) Relationships between tinnitus and the prevalence of anxiety and depression. Laryngoscope 127: 466-469.
- Ziai K, Moshtaghi O, Mahboubi H, Djalilian HR (2017) Tinnitus patients suffering from anxiety and depression: a review. Int Tinnitus J 21: 68-73.
- Lloyd LL, Kaplan H (1978) Audiometric Interpretation: A Manual of Basic Audiometry. 2nd, University Park Press, Baltimore.
- Suzuki FAB, Suzuki FA, Onishi ET, Penido NO (2018) Psychoacoustic classification of persistent tinnitus. Braz J Otorhinolaryngol 84: 583-590.
- Krabbe PFM (2017) Chapter 5 - Constructs and Scales. In: Krabbe PFM, The Measurement of Health and Health Status. 1st, Groningen, NL: Academic Press pp. 67-89.
- Klimek L, Bergmann KC, Biedermann T, Bousquet J, HellingsP, et al. (2017) Visual analogue scales (VAS): Measuring instruments for the documentation of symptoms and therapy monitoring in cases of allergic rhinitis in everyday health care. Allergo J Int 26: 16-24.
- Nemade SV, Shinde KJ (2019) Clinical efficacy of tinnitus retraining therapy based on tinnitus questionnaire score and visual analog scale score in patients with subjective tinnitus. Turk Arch Otorhinolaryngol 57: 34-38.
- Prayuenyong P, Kasbekar AV, Baguley DM (2020) Clinical implications of chloroquine and hydroxychloroquine ototoxicity for COVID-19 treatment: a mini-review. Front Public Health 8: 252.
- Beukes EW, Baguley DM, Jacquemin L, Lourenco MPCG, Allen PM, Onozuka J, et al. (2020) Changes in tinnitus experiences during the COVID-19 pandemic. Front Public Health 8: 592878.
- Anzivino R, Sciancalepore PI, Petrone P, D’Elia A, Petrone D, et al. (2021) Tinnitus revival during COVID-19 lockdown: how to deal with it? Eur Arch Otorhinolaryngol 278: 295-296.
- Schlee W, Hølleland S, Bulla J, Simoes J, Neff P, et al. (2020) The effect of environmental stressors on tinnitus: a prospective longitudinal study on the impact of the COVID-19 pandemic. J Clin Med 9: 2756.
- Görtelmeyer R, Schmidt J, Suckfüll M, Jastreboff P, Gebauer A, et al. (2011) Assessment of tinnitus-related impairments and disabilities using the German THI-12: sensitivity and stability of the scale over time. Int J Audiol 50: 523-529.
- Lee JH, Ra JJ, Kim YH (2014) Adequacy of the simplified version of the Tinnitus Handicap Inventory (THI-S) to measure tinnitus handicap and relevant distress. Korean J Audiol 18: 19-27.
- Figueiredo RR, Azevedo AA, Oliveira PM (2009) Correlation analysis of the visual-analogue scale and the tinnitus handicap inventory in tinnitus patients. Braz J Otorhinolaryngol 75: 76-79.
- Nascimento IP, Almeida AA, Diniz Junior J, Martins ML, Freitas TMMWC, et al. (2019) Tinnitus evaluation: relationship between pitch matching and loudness, visual analog scale and tinnitus handicap inventory. Braz J Otorhinolaryngol 85: 611-616.
- Guitton MJ, Pujol R, Puel JL (2005) m-Chlorophenylpiperazine exacerbates perception of salicylate-induced tinnitus in rats. Eur J Neurosci 22: 2675-2678.
- Pinto PC, Marcelos CM, Mezzasalma MA, Osterne FJ, de Melo Tavares de Lima MA, et al. (2014) Tinnitus and its association with psychiatric disorders: systematic review. J Laryngol Otol 128: 660-664.
- Wang H, Brozoski TJ, Caspary DM (2011) Inhibitory neurotransmission in animal models of tinnitus: maladaptive plasticity. Hear Res 279: 111-117.
- Richardson BD, Brozoski TJ, Ling LL, Caspary DM (2012) Targeting inhibitory neurotransmission in tinnitus. Brain Res 1485: 77-87.
- Leaver AM, Seydell-Greenwald A, Turesky TK, Morgan S, Kim HJ, et al. (2012) Cortico-limbic morphology separates tinnitus from tinnitus distress. Front Syst Neurosci 6: 21.
- Xia L, He G, Feng Y, Yu X, Zhao X, et al. (2021) COVID-19 associated anxiety enhances tinnitus.PLoS One 16: e0246328.
- Sanchez TG, Medeiros IRT de, Fassolas G, Coelho FF, Constantino GTL, et al. (2001) Frequency of glucose, lipids and thyroid hormones disorders in tinnitus patients. Archives of Otorhinolaryngology 5: 16-20.
- Hofmeister M (2019) Do dietary factors significantly influence tinnitus? Aust J Gen Pract 48: 153-157.
- Onishi ET, Coelho CCB, Oiticica J, Figueiredo RR, Guimarães RCC, et al. (2018) Tinnitus and sound intolerance: evidence and experience of a Brazilian group. Braz J Otorhinolaryngol 84: 135-149.
- Jastreboff PJ, Hazell JWP (2008) Tinnitus Retraining Therapy: Implementing the Neurophysiological Model. 1st edn, Cambridge University Press, Cambridge, UK.
- Luo M, Guo L, Yu M, Jiang W, Wang H (2020) The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - a systematic review and meta-analysis. Psychiatry Res 291: 113190.
- Liang Y, Xu J, Chu M, Mai J, Lai N, et al. (2020) Neurosensory dysfunction: a diagnostic marker of early COVID-19. Int J Infect Dis 98: 347-352.
- Andersson G, Strömgren T, Ström L, Lyttkens L (2002) Randomized controlled trial of internet-based cognitive behavior therapy for distress associated with tinnitus. Psychosom Med 64: 810-816.
- Beukes EW, Andersson G, Allen PM, Manchaiah V, Baguley DM (2018) Effectiveness of guided internet-based cognitive behavioral therapy vs face-to-face clinical care for treatment of tinnitus: a randomized clinical trial. JAMA Otolaryngol Head Neck Surg 144: 1126-1133.
Citation: Neto APF, Costa MB, de Barros Suzuki FA, Onishi ET (2021) Tinnitus Increase during the COVID-19 Pandemic in Brazil. J Otolaryng Head Neck Surg 7: 63
Copyright: © 2021 Adriana Perez Ferreira Neto, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

