
Toothbrushes and Tooth Brushing Methods: A Periodontal Review
*Corresponding Author(s):
Sudhanshu AgrawalDepartment Of Periodontology, Chandra Dental College & Hospital, Barabanki, India
Tel:+91 9415400591,
Email:drsudhanshu_bds@hotmail.com
Abstract
Tooth brushing is a basic technique to prevent major oral diseases (e.g., dental caries and periodontal disease). Several methods of tooth brushing technique devised by some dental scholars have been introduced. However, some guidelines to select the proper method are needed for an individual patient considering age and oral status. Methods such as rolling, Fones’, Bass, Stillman, Charters, Watanabe’s tooth-pick, and other modifications have been introduced. The rolling technique was recommended for general use, the Fones’ technique for preschool children, the Bass technique for the patient with gingivitis with gingival sulcus problem, the Stillman technique for widespread gingivitis, and the Charters technique for bridge wearer. Moreover, fixed-type orthodontic appliance wearer is recommended to use the mix-type methods as Bass, rolling, and Charters. Moreover, the Watanabe’s technique would be available for patients with a dental implant or periodontal problem. The denture wearer should clean the denture with a partial denture brush for a partial denture and a full denture brush for a full denture with the rolling method or its modification. The selection of the proper tooth brushing method suggested in this article would be one of the guidelines for clinical use of tooth brushing instruction for preventive measures.
Keywords
Dental caries; Oral status; Periodontal diseases; Simple plaque score; Tooth brushing
Introduction
After teeth have been completely cleaned by the dental professional or by the individual, soft microbial dental plaque continually reforms on the tooth surfaces. With time, plaque is the primary agent in the development of caries, periodontal disease, and calculus the three conditions for which individuals most often seek professional services. If plaque, particularly at interproximal and gingival areas, is completely removed with home-care procedures, these dental-disease conditions can be prevented. Unfortunately, the majority of the population is unable, uninstructed, or unwilling or does not realize the need to spend the time to remove plaque from all tooth surfaces, and/or the product(s) used are not adequate to remove plaque at critical sites. Plaque deposits can be removed either mechanically or chemically.
The Manual Toothbrush and Its History
Hirschfeld, in his 1939 landmark textbook on the toothbrush and oral care, included an in-depth review of the history of tooth brushing [1]. The exact origin of mechanical devices for cleaning teeth is unknown. Ancient peoples chewed twigs from plants with high aromatic properties. Chewing these twigs freshened the breath and spread out fibers at the tips of the twig for cleaning the tooth and gum surfaces. The Arabs before Islam used a piece of the root of the arak tree because its fibers stood out like bristles; this device was called a siwak. After several uses, the bristle fibers became soft, and a new “brush” was created by stripping off the end and making new bristle fibers. In the seventh-century, Mohammed made rules for oral hygiene, and so it became a religious obligation. To this day the siwak, composed from aromatic types of wood, is still used. Chew sticks not only help to physically clean teeth but also, because they contain antibacterial oils and tannins, may help prevent or remove plaque [2]. The Chinese are credited for inventing the toothbrush comprising a handle with bristles during the Tang dynasty (618-907 A.D.). They used hog bristles similar to those in some contemporary models. In 1780, in England, William Addis manufactured what was termed the first modern toothbrush [3,4]. This instrument had a bone handle and holes for placement of natural hog bristles, which were held in place by wire. In the early 1900s, celluloid began to replace the bone handle, a changeover that was hastened by World War I when bone and hog bristles were in short supply. As a result of the blockade of high-quality natural hog bristles from China and Russia during World War II, nylon bristles were used instead. Initially, nylon bristles were copies of natural bristles in length and thickness. They were stiffer than natural bristles of similar diameter. They did not have the hollow stem of natural bristles and, accordingly, did not absorb water. Compared to natural bristles, nylon filaments have the additional advantages that they can be prepared in various uniform diameters and shapes, and can be end-rounded to be more gentle on gingival tissues during the brushing procedure. In 1924, an American dentist reported on 37 different manual toothbrushes with regard to handle shape, head design, bristle type, length, and width. Individual dentists disagreed then, and still do today, on what type of toothbrush was best. The primary toothbrush shapes marketed in the 1940s through 1980s in the United States had flat, multitufted toothbrush-head shapes. Since the 1990s new manual toothbrushes have been introduced with new shapes, sizes, colors, and claimed advantages. By varying the length and the angle of the filaments in the brush head, brushing with these newly designed products has been documented to improve plaque removal since the bristle filaments can be directed into the sulcus or interproximal areas [3-12]. New unconventional toothbrushes with two or more heads or segments of filaments in angular relation- ship have shown improved plaque removal. One new brush with three heads can be used to simultaneously clean the buccal, occlusal, and lingual surfaces [13-15]. The proliferation of brushes can be attributed, in part, to advances in manufacturing, for example, the attachment of bristles into the handle using molding techniques rather than stapling to allow a wider flexibility in toothbrush designs and bristle angulations. In addition, toothbrush bristles are now available in a variety of colors, textures and shapes. There also has been an increase in both the quality and number of laboratory and clinical research studies on toothbrushes. The International Association of Dental Research and American Association of Dental Research are major meetings for both academic and industry scientists to present their latest research. In the 1991 and 1992 key-word indexes of the abstracts accepted for presentation at these meetings, toothbrushes were not included as a topic. In 1993 the number of abstracts were ranked as dentifrices, mouth rinses and toothbrushes. Since then, through 2001, the number of dentifrice abstracts has shown marked increases or decreases, with a peak of over 90 abstracts in 1998. Mouth rinse abstracts have shown essentially a leveling-off or a slight decrease in number since 1991. Toothbrush abstracts have continued to demonstrate a consistent increase, and at the 2001 AADR meeting, exceeded dentifrices and mouth rinses. With the scientific reports about toothbrush contamination after oral or medical bacterial/ viral infections, dental professionals recommend replacing toothbrushes at 3- to 4-month intervals, so repeat purchasing of toothbrush products is done more frequently. The increase in toothbrush sales may be an additional driving force for the marketing of new designs and variety of toothbrushes. Toothbrush pricing has reached new highs with the introduction of “high-tech” manual toothbrush designs and stronger claims, yet the cost per individual product is generally less than the cost for a “family-size” tube of toothpaste or mouthrinse. Toothbrush shipping costs are less, breakage is minimal and the shelf-life (stability) is longer than for other product categories thus, the potential profitability of toothbrushes to the manufacturers may be greater than for dentifrice or mouth rinse products.
Manual Toothbrush Designs
Manual toothbrushes vary in size, shape, texture, and design more than any other category of dental products [5]. A manual toothbrush consists of a head with bristles and a handle. When the bristles are bunched together, they are known as tufts. The head is arbitrarily divided into the toe, which is at the extreme end of the head, and the heel, which is closest to the handle. A constriction, termed the shank, usually occurs between the handle and the head. Many toothbrushes are manufactured in different sizes large, medium, and small (or compact) to adapt better to the oral anatomy of different individuals [5,7]. Toothbrushes also differ in their defined hardness or texture, usually being classified as hard, medium, soft or extra soft. Much of the early data comparing the efficacy of various toothbrush designs is contradictory because of (1) the lack of quantitative methods used to measure cleaning (plaque removal), (2) the many sizes and shapes of toothbrushes used, and (3) the lack of standardized tooth brushing procedures used in the studies. More recently, toothbrush heads have been altered to vary bristle lengths and placement in attempts to better reach inter proximal areas. Handles have also been ergonomically designed to accommodate multiple dexterity levels. As described in the introduction, the change from the old flat toothbrush to multilevel designs was possible because of new bristle technology and manufacturing procedures. When viewed from the side, toothbrushes have four basic lateral profiles: concave, convex, flat, and multileveled (rippled or scalloped). The concave shape can be useful for improved cleaning of facial surfaces, whereas convex shapes appear more useful for improved cleaning of lingual surfaces [5]. In laboratory and clinical studies, toothbrushes with multilevel profiles were consistently more effective than flat toothbrushes, especially when inter proximal efficacy was monitored [6,8,11,16,17]. Recently, new toothbrush bristle shapes and textures have been fabricated. Toothbrush products utilizing these bristles in multiple diameters, textures, and bristle trims have been developed, and laboratory studies have documented improved efficacy of toothbrushes with tapered, feathered and diamond-shaped bristles, compared to toothbrushes with standard round bristles [18-20]. Originally, individual toothbrush bristles were cut bluntly and often had sharp end configurations. In 1948, Bass reported that these bristle tips could damage the soft tissues and that rounded, tapered, or smooth bristle tips were less abrasive [21]. Although Bass's research was not performed according to strict research protocol, his findings have remained undisputed for more than 40 years. Indeed, advertisers still recommend end-rounded tips for safety and to promote toothbrush sales. When toothbrushes are examined under low magnification, most bristles labeled as “rounded” do in fact appear smooth or end-rounded. However, at higher magnification, many of these “rounded” bristles take on different configurations [5]. During use, bristles become smoother and more end-rounded. With continued use, the bristles of the tuft expand and spread out [22]. Bristle wear has been shown to vary directly with the tooth brushing load and amount of dentifrice and inversely with bristle diameter [23]. In a recent study, there were no significant differences in plaque or gingivitis indices in a group in which toothbrushes were replaced on a monthly basis compared to the second group using their same toothbrush over the 3 month period. The toothbrushes used for 3 months exhibited a significant increase in the wear index compared to the baseline values [24]. A 1988 scanning-electron microscope study compared end- rounding of bristles from eight marketed types [25]. Based on statistical analysis of 30 toothbrushes of each type, acceptability varied from 22 to 88%, indicating to these authors that some brushes are not sufficiently rounded and are likely to produce gingival damage. In addition, they have abrasive potential on dentin and cementum. A 1992 study compared a ripple design with a flat-profile brush using a stereoscopic microscope with fiberoptic lighting [26]. Close to 90% of the bristles of the ripple brush were end-rounded, whereas the flat brush had an average of 52% rounded bristles. Apparently, the degree of end-rounding depends on a manufacturer's specifications and not on toothbrush design. In a study conducted in 2001 on 31 different toothbrushes, only 4 products had more than 50% of the filaments rounded; in 19 products, end-rounding was 12 to 40% and only 0 to 7% in 8 brands. The authors concluded that a large percentage of marketed toothbrushes do not meet acceptable end-rounding criteria [27]. If bristles are cut, frayed, or are hollow they can harbor bacteria, viruses, and other potential periopathogens, especially if no dentifrice is used, and they can transfer these into and around the mouth [28].
 Figure 1: Manual Toothbrush Designs.
Figure 1: Manual Toothbrush Designs.
Handle Designs
Many of the new toothbrushes in the United States have a styled-handle design. Modifications, such as triangular extrusions or indentations along the sides for a better grasp, a “thumb position” on the back of the handle for more comfort, and various angle bends to permit better access into and around the mouth, have been introduced. Several brushes have recently been marketed with an “angled” design, stated to be like a dental instrument. These toothbrushes are similar to a dental professional's mirror. Brushes are also available, with a handle on the same plane as the bristle tips, as are dental instruments used for caries evaluations and prophylaxes. With both the offset and angled-offset designs, points of bristle contact are in line with the longitudinal axis of the handle during brushing. Handle design and length may provide comfort and compliance during toothbrush use and these factors have recently been documented to improve the quality of tooth brushing. This is particularly true of toothbrushes for children, whose dexterity may not be highly developed [8,9] (Figure 2).
 Figure 2: Handle Designs.
Figure 2: Handle Designs.
Texture
Nylon bristles have a uniform diameter and a wide range of predictable textures. Texture is defined as bristle resistance to pressure and is also referred to as firmness, stiffness, and hardness. The firmness or texture of a bristle is related to its (1) composition, (2) diameter, (3) length, and (4) number of individual bristles per tuft. In the manufacturing process, the diameter of nylon bristles can be well controlled. Because the majority of toothbrushes contain bristles 10- to 12-millimeters long, the diameter of the bristle becomes the critical determinant of texture. The usual range of diameters for adult toothbrush bristles is from 0.007 to 0.015 inches. Factors such as temperature, uptake of water (hydration), and toothbrush-use frequency affect texture. Texture labeling is not standardized. Individual manufacturers label their brushes according to their testing criteria. Thus one manufacturer’s “soft” grade may be stiffer than another manufacturer's “medium” grade. The International Organization for Standardization (ISO) has formulated testing procedures that permit manufacturers to label their brushes in a consistent manner [29]. The American Dental Association is a member of ISO (Figure 3).
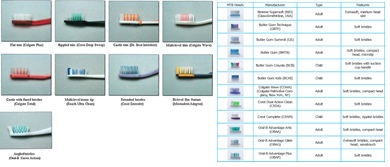 Figure 3: Nylon Versus Natural Bristles.
Figure 3: Nylon Versus Natural Bristles.
The nylon bristle is superior to the natural (hog) bristle in several aspects. Nylon bristles flex as many as 10 times more often than natural bristles before breaking; they do not split or abrade and are easier to clean. The configurations and hardness of nylon bristles can be standardized within specified and reproducible tolerances. Natural bristle diameters, since they are tapered, vary greatly in each filament. This can lead to wide variations in the resulting texture of the marketed toothbrush. As a result of the advantages of nylon, as well as its ease and economy of production, relatively few natural bristle toothbrushes are marketed.
Actions
Bristle actions caused by different brushing motions are illustrated in a 1992 publication7 that measured and quantified three-dimensional individual movements during brushing. Data frames were filmed to create a computer-generated reanimation of brushing motions in order to design new toothbrush bristle conformations. These authors concluded that an individual's brushing techniques do not vary and are inadequate; therefore bristle configurations in newly designed toothbrushes could be developed to be adaptable to any brushing style
Powered Toothbrushes
Powered toothbrushes were first advertised in Harper’s Weekly in February 1886 [30], but only became a factor in the U.S. marketplace beginning in the 1960s with the introduction of Broxadent. With the commercial success of this product, battery-powered products were introduced with the advantage of being portable and available at a lower cost. Unfortunately, problems with these battery-powered products included short “working times” and mechanical breakdowns. The enthusiasm for the powered toothbrush declined and was recommended mainly for the handicapped. In the 1980s, the category of powered toothbrushes was revitalized with the introduction of the InterPlak product. This “second generation” powered toothbrush had a uniquely rotating head and was powered by long-life/ rechargeable batteries. Increased efficacy compared to manual toothbrushes was consistently demonstrated in published studies [4,8,9,31-33]. Since then, sonic-powered toothbrushes of a “third” generation have been developed and shown to remove more plaque in comparison to manual toothbrushes, especially in long-term studies. Two primary types of head designs are now used: the rotating, oscillating type with a small, round molar-crown-size brush head and three oscillating brushes with either vibrating or rotational sonic movements [34-37]. Plaque removal by these brushes appears equally effective; periodontal therapeutic effects were demonstrated in pockets of 5 mm. Most recently, powered toothbrushes have been introduced that are battery-powered or disposable after “running down,” and are priced, in the United States below $20.00. Published studies have been found on two of these brushes [38,39]. In most developed countries, the number of powered toothbrush products sold has increased dramatically in recent years. In Switzerland, the regular use of powered toothbrushes increased from 10 to 30% in the last decade. In epidemiological studies, it has been documented that populations are exhibiting increased gingival abrasion and recession. This has been associated with the increased use of oscillating powered toothbrushes. In comparison to these oscillating toothbrushes, sonic toothbrushes have been shown to do little harm to the gingiva. Also sonic brushes of this type can be used up to 6 or 12 months because the bristles show minimal overt signs of use and do not splay [40-44]. The heads of most powered or mechanical toothbrushes are smaller than manual toothbrushes and are usually removable to allow for replacements. The head follows three basic patterns when the motor is started: (1) reciprocating, a back-and-forth movement; (2) arcuate, an up-and-down movement; and (3) elliptical, a combination of the reciprocating and arcuate motions. Powered toothbrushes are consistently superior to manual toothbrushes in plaque removal and gingivitis efficacy [9,31,45]. Differences are most significant when tested against manual toothbrushes. Motivation to improve oral hygiene appears to be a key factor for patients to purchase powered toothbrushes [31,46]. In a survey by the ADA, of the 139 respondents who owned powered toothbrushes, 21.6% used them regularly, and 25.2% used them occasionally [47]. This survey does not indicate the tooth brushing frequency of the remaining 53%. A published study on the use of powered toothbrushes found that when consumers first purchased the electric brush they increased their frequency of brushing. The effectiveness is especially improved when the users are given instructions and controlled during the first 6-month period. More recently [48], a survey conducted 6 months after subjects completed a clinical efficacy study indicated that most subjects were not using their powered device twice a day. With the development of the second and third generation of powered toothbrushes, it appears that long-term use is increasing; however, recent publications on this have not been definitive. Weinstein, et al. analyzed the failures of motivation [49]. One of the important aspects is to accept each patient as an individual, and the dental hygienist and dentist should be able to listen to the patient. Oral hygiene can be instructed only when we are informed about a patient's attitudes, and he or she has to demonstrate their oral hygiene. The procedure in brushing for any method used should have a definite sequence. Health professionals should take time and not expect the patient to change more than one thing from session to session. It is important to have a preventive program for each patient, and this starts with the charting. After the first steps we should follow the program to obtain the goals with the patient. The patient’s progress should be evaluated from session to session and from year to year. Dental professionals should also accept failures and have an alternative plan to implement in case of failure. Tooth brushing devices have been developed that accurately standardize all of the above factors, in addition to length and number of tooth brushing strokes over simulated anterior or posterior teeth. Published testing methods are now available to evaluate both safety and efficacy of manual and powered toothbrushes. Differences between products can be determined and, in several areas, are predictive of clinical results. For example, three laboratory methods have been predictive of clinical plaque removal when plaque assessments focusing on interproximal areas were used. Significant clinical differences between toothbrush designs have also been documented [8,9,17]. Interproximal access efficacy has been directly related to increasing brushing pressures and inversely correlated with bristle texture (the “softer” the texture, the higher the interproximal efficacy) [50,51]. Clinical advantages of various toothbrush-head configurations for removing dental plaque and debris (cleaning efficacy) have been difficult to substantiate. This is attributed to the wide variations among individuals in tooth brushing times, motions, pressures, and in the shape and number of teeth present. Published studies on the clinical superiority of one newly designed manual or powered toothbrush versus another have been inconsistent. It is clear, however, that these new products are more effective than standard manual brushes [8,9].
The American Dental Association (Ada) Acceptance Program
The American Dental Association (ADA) has established guidelines to enable manufacturers to obtain an acceptable rating and use the ADA Seal of Acceptance. In 1996, the Council on Scientific Affairs of the American Dental Association proposed new guidelines for the Seal of Acceptance [52]. These guidelines require laboratory documentation of acceptable end-roundedness, Good Manufacturing Procedures (GMPs), and equivalency in clinical plaque and gingivitis efficacy compared with a control toothbrush provided by the ADA. Manual toothbrushes with a standard design, acceptable laboratory data, and GMPs do not require clinical testing. For manual toothbrushes with new designs and for mechanical brushes, the guidelines require only equivalency in plaque and gingivitis reduction compared with a toothbrush provided by the ADA. The statement to be used in the labeling of products accepted by the ADA is: “(Product Name) is accepted as an effective cleansing device that has been shown to remove plaque and reduce gingivitis when used as directed in a program of good oral hygiene to supplement regular professional care. As listed on the American Dental Association’s website (www.ADA.org), more than 140 manual toothbrushes have been awarded the ADA Seal of Approval (August 2001). The ADA has developed criteria for acceptance of powered toothbrushes based on both safety and efficacy. These are: (1) laboratory evidence of electric safety, that is, no electric shock hazard; (2) clinical evidence of both hard- and soft-tissue safety under unsupervised conditions; (3) clinical evidence of plaque and gingivitis efficacy compared to a toothbrush already accepted and provided by the ADA; and (4) evidence of proper labeling and advertising claims that may mention plaque reduction but not improvement of any existing oral disease.52 The required statement for labeling and commercial claims on powered toothbrushes accepted by the ADA is the same as for manual toothbrushes. As of August 2001, 10 powered toothbrushes have been awarded the ADA Seal of Acceptance. Five of these products are distributed by Water Pik Technologies (Figure 4).
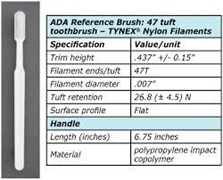 Figure 4: Toothbrushing Methods.
Figure 4: Toothbrushing Methods.
The objectives of tooth brushing are to (1) remove plaque and disturb reformation; (2) clean teeth of food, debris, and stain; (3) stimulate the gingival tissues; and (4) apply dentifrice with specific ingredients to address caries, periodontal disease or sensitivity. During the last 50 years many tooth brushing methods have been introduced, and most are identified by an individual's name, such as Bass, Stillman, Charters, or by a term indicating a primary action to be followed, such as roll or scrub. No one method shows consistently better results in removing plaque than scrubbing. Most studies with manual toothbrushes and the different instructed methods show more gingival abrasion than with powered sonic toothbrushes. Most people brushing with an instructed professional method are not aware that they are brushing in a specific way. Thus it may be more effective to instruct patients to improve their own method. This can be achieved by using a plaque disclosant to stain plaque or identify areas that are missed during tooth brushing. Then the patient can be taught how to clean the sites properly and on the next visit be rechecked. The proposed adaptation has to be recorded in the patient's chart and rechecked at the beginning of the next session, as not all patients can remember all the instructions. Additionally, professionals should never argue with a patient but instead should encourage and help. Various tooth brushing methods will be briefly described here. For more details see the original papers or this chapter in the previous textbook edition. The toothbrushing methods most emphasized are horizontal scrub, Fones, Leonard, Stillman, Charters, Bass, rolling stroke (press roll), and Smith-Bell. All of these techniques are applicable to the cleaning of the facial, lingual, and to some extent to occlusal surfaces; all are relatively ineffective in cleaning interproximal areas; and only the Bass technique is effective in cleaning the sulcus.
Horizontal Scrub Method
It has been the most popular motion for tooth-brushing technique by uneducated people. It is a motion for scrub tooth-surface with horizontal movement as back and forth ward. It can be occurred the accumulation of micro-debris at the inter-dental area and happen the cervical abrasion or hyper sensitive dentin through the using this motion for a long time as 20 or 30 years (Figure 5).
 Figure 5: Horizontal scrub method.
Figure 5: Horizontal scrub method.
Rolling Method
Rolling method of tooth-brushing is world-wide spread method recommending for general peoples who have not specific oral problems. It had been once recommended by World Health Organization as well as the Ministry of Health and Welfare in Korean government for general people. It has been suggested the movement of rolling through wrist the hand which had hold a tooth-brush. Sweep the tooth surface from up to down movement with rolling the hand-wrist in upper teeth, and from down to up in lower teeth. Insert the tooth-brush straight with obliquely at inner side of frontal teeth, both in upper and lower teeth, and sweep the brush from inside to outside and horizontal movement as back and forth for occlusal surface of posterior teeth, both upper and lower. Rolling technique is known as comparatively easy for learning and effective for removal of plaque even at proximal area (Figure 6).
 Figure 6: Rolling method.
Figure 6: Rolling method.
Bass Technique
Bass technique of tooth-brushing has been recommended for periodontal problem dental patient, even though it had been some difficult to perform. It needed for soft and 1 or 2 lane tooth-brush to vibrate shortly and lightly with holding tooth-brush handle with lightly. Short and light vibration would be needed inserting one lane of tooth-brush into the gingival sulcus or periodontal pocket which had been some inflammatory tissues. Vibratory action could induce the plaque removal and gingival massage effect at the gingival sulcus, in order to subsid the gingivitis. Recent years, the modification of Bass method as adding the rolling motion together to Bass method has been recommended for subsid gingivitis as well as plaque removal effectively (Figure 7) [5].
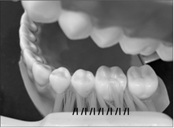 Figure 7: Bass method.
Figure 7: Bass method.
Stillman Method
Stillman method would be applied for gingival inflam-mation area with relatively wide spread. Short zig-zag movement with soft bristled and 3 or 4 lane tooth-brush holding with lightly, from up to down ward sweep with short vibration on the gingiva at the upper jaw and from down to up at the lower jaw. Gingival massage effect would be great to increase the blood circulation on the inflammatory gingival area. Also modification would be performed by adding the rolling motion after zig-zag vibration at gingiva (Figure 8).
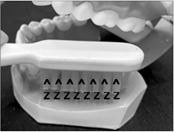 Figure 8: Stillman method.
Figure 8: Stillman method.
Fones’ method
Dr. Fones was a pediatric dentist and try to supply the proper and easy method for tooth-brushing for preschool child as sweeping with small sized kids tooth-brush with motion as drawing continues circle on the teeth with closing the mouth slightly. It could be easier to change the rolling method after school aging than in horizontal scrub method. Horizontal scrub action would be accomplished on brushing on occlusal site and lingual site (Figure 9) [6].
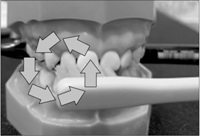 Figure 9: Fones method.
Figure 9: Fones method.
Charters method
This method of tooth-brushing is emphasize to clean the interdental area especially. Insert tooth-brush tip with perpendicular direction to longitudinal tooth axis at the proximal area or revers 45 degrees from the gingiva to tooth direction. And then, short vibration would be needed focusing on the proximal area. But, this method is a little bit hard to perform at lingual side of the tooth surface. This method is effective for bridge wearer and well done at the bottom of the artificial tooth on bridge area. Of course, it could be applied as modified method by adding the rolling motion (Figure 10) [7].
 Figure 10: Charters method.
Figure 10: Charters method.
Watanabe’s, tooth-pick method
Dr. Watanabe has suggested that plaque removal and gingival massage would be very important for periodontal problem patient or dental implant patient, and they should eliminate the plaque through the tooth-brushing movement of pushing action from buccal side to lingual side with short vibration, so we call as tooth-pick method. It might be some hard for patient to perform by oneself at the first without professional person aid, and it needed some trainings from the dental professions (Figure 11).
 Figure 11: Watanabe’s, tooth-pick method.
Figure 11: Watanabe’s, tooth-pick method.
Clinical Application Of Proper Method For Each Patient
General dental patients
For the general dental patients age from over 7, and without any special problems or wearing the special dental appliance, rolling method is recommended to perform and to be habitual use (Table 1).
|
Perio probl: periodontal problem patient, Orthodo: orthodontics, Gingiv: Gingivitis, Perio pocet: periodontal pocket, Horiz.: horizontal scrub, Interd. Br.: interdental brush, Inn. Front Tooth: inner site of frontal tooth, M: modification, Occ: occlusal surface, Br.tip: bristle tip, 45 dege.: 45 degrees, Interd.: interdental, Hardne.: hardness, Hypersen: hypersensitivity, Can: canine, Smal. Siz: small size, Bru: brush, Prox.B: proximal brush, Part.b: partial denture brush, Full Bru: full denture brush, Plaq. Rem: plaque removal, Prev. calc,: prevention of calculus deposit, Abrasi: Abrasion, Soft des.: soft brush, desensitization dentifrice, Desensit: desensitization effect, Habit Ch,: habit for child, Ging. Ma.: gingival massage, Prox cle: proximal cleansing, Periimpl: peri-implantitis. |
Table 1: Recommend tooth-brushing method according to patient age or oral status
Preschool age child
For preschool child, Fones’ technique is recommended for easy learning to use and changing it with rolling technique in the later (Table 1).
Gingivitis-gingival sulcus
Modified Bass technique would be available for gingivitis dental patient for cleansing in the gingival sulcus and gingival massage (Table 1).
Gingivitis-wide area with periodontitis
Modified Stillman’s method would be recommended with short and soft zig-zag vibration by moving the vibration from apical to coronal direction and then, the rolling movement would be added (Table 1).
Bridge wearer
At bridge portion, Charters method would be available to clean the inter-proximal and the bottom of the pontic area, as short vibratory action with inserting the bristle tip into the proximal or bottom of the pontic area by locating the head of tooth-brush with reverse 45 degrees from the long axis of the tooth (Table 1).
Fixed orthodontic appliance patient [8,9]
At first, horizontal scrub would be applied on the labial surface to clean upper and lower of the bracket, and then short vibration action would be applied at upper, lower and subgingival sulcus from 1 tooth by the other tooth, by use of concave form of the bristle head tooth-brush. Rolling motion would be done at lingual surface and back and forth stroke at the occlusal surface. It should be needed to use the interdental brush for cleaning the proximal area and around the bracket. Water pick is also recommended to use to clean the interdental area and around the bracket (Table 1).
Hypersensitive dentin [10]
Rolling technique should be educated for the hypersen-sitive dentine with cervical abrasion, owing to habits for tooth-brushing with horizontal scrub for a long time (Table 1).
Implant patient
Watanabe suggested tooth-pick method for implant patient as well as severe problem at the interdental area. Insert the brush tip into the proximal area of the implant tooth with perpendicular or reverse 45 degrees to the long axis of the tooth and push it with zig-zag vibration action from buccal to lingual direction, like using the tooth-pick. It could be hard to perform for lingual surface and rolling method would be recommended if it could be hard (Table 1).
Denture cleaning
Partial denture should be cleaned by use of partial denture brush and full denture for full denture brush, with holding the denture on the water base or towel. Brushing method would be a modification of rolling technique and specific cleansing at the specific part as like a clasp. Denture should be storage within the water with denture cleaner tablet when sleeping at night time (Table 1).
Natural Methods of Brushing
The most natural brushing methods used by patients are a reciprocating horizontal scrub technique [53], a rotary motion (Fones's technique) [54], or a simple up-and-down motion over the maxillary and mandibular teeth (Leonard's technique) [55]. Patients managing effective tooth brushing with these methods without causing traumatic problems or disease should not alter their brushing methods just for the sake of change [56]. Stillman’s method was originally developed to provide gingival stimulation [57]. The toothbrush is positioned with the bristles inclined at a 45-degree angle to the apex of the tooth, with part of the brush resting on the gingiva and the other part on the tooth. A vibratory motion is used with a slight pressure to stimulate the gingiva. The brush is lifted and then replaced in the same area, and pulsing is repeated. Charters advocated a pressure-vibratory technique to clean interproximal areas [58]. The toothbrush should be placed at a 90-degree angle to the long axis of the teeth so that the bristles are gently forced between the teeth but do not rest on the gums. The brush is moved in several small rotary motions so that the sides of the bristles are in contact with the gum margin. After two or three such motions, the brush is removed and replaced in the same area and the motions are repeated. It is important to note that the Bass technique was the first to focus on the removal of plaque and debris from the gingival sulcus by the combined use of a soft toothbrush and dental floss. The method is effective for removing plaque adjacent to and directly beneath the gingival margins as part of the self-care regimen for controlling periodontal disease and caries. In the Bass technique, the toothbrush is positioned in the gingival sulcus at a 45-degree angle to the tooth apex. The bristles are then gently pressed to enter the sulcus. A vibratory action, described as a back-and-forth horizontal jiggle, causes a pulsing of the bristles to clean the sulci [59]. Ten strokes are advised for each area. In the rolling-stroke method, the toothbrush bristles are positioned parallel to and against the attached gingiva, with the toothbrush head level with the occlusal plane. The wrist is then turned to flex the toothbrush bristles first against the gingiva and then the facial surface. A sweeping motion is continued until the occlusal or incisal surface is reached. The toothbrush bristles are at right angles to the tooth surface as the brush passes over the crown. The press roll action is repeated at least five times before proceeding to the next site [60].
Modified Brushing Methods
In attempts to enhance brushing of the entire facial and lingual tooth surfaces, the original techniques have been modified. Some modifications like the Bass method may induce a more pronounced gingival trauma with standard brushes [61]. New toothbrush designs such as multilevel and cross-section bristles that have been tested are not only more effective but can be also less harmful [62]. The following considerations are important when teaching patients a particular tooth brushing technique: (1) the patient’s oral health status, including number of teeth, their alignment, patient’s mouth size, presence of removable prostheses, orthodontic appliances, periodontal pockets, and gingival condition; (2) the patient's systemic health status, including muscular and joint diseases, and mental retardation; (3) the patient's age; (4) the patient's interest and motivation; (5) the patient's manual dexterity; and (6) the ease and effectiveness with which the professional can explain and demonstrate proper tooth brushing procedures.
Recommended Powered Tooth brushing Methods
Most powered toothbrush manufacturers do not recommend a specific brushing method, however, the electric brushes should be used in a specified manner. The Swiss Dental Society, in 2001 developed an instruction manual [63]. Instructions for brushes with a sweeping and /or oscillating rotary motion are as follows:
- The brushes are positioned on the tooth surfaces in a 45- or 90-degree angle to the incisal plane. Only when positioned should the brush be switched to "on." The mouth should be almost
- The brush should be moved slowly over and around each tooth for 3 to 5 seconds, making sure that the bristles clean the crevices between the
- The brush head can be lifted distally and mesially into the interproximal areas to reach the interdental area; the brush always remains on a single
- After a period of approximately 5 seconds, the brush is moved to the next tooth surface and
- Experienced individuals can use the brush also in a perpendicular angle to the teeth and gums, but the applied force has to be gentle. In this way, each tooth in the upper and lower arch is cleaned on the buccal and lingual surfaces.
- It is best to divide the mouth into four quadrants (upper-right, upper-left, lower-right, and lower-left) and to start brushing on a tooth in the upper rear and then clean one surface after the other very
- It is an easy way, gives good control for the individual, and does not omit any tooth surface. This method takes more time, because at a single time interval, only one tooth surface can be
Tooth Brushing Time and Frequency
For many years the dental professional advised patients to brush their teeth after every meal. The ADA has modified this position by use of the statement that patients should brush “regularly”. Research has indicated that if plaque is completely removed every other day, there will be no deleterious effects in the oral cavity [64]. On the other hand, because few individuals completely remove plaque, daily brushing is still extremely important to maximize sulcular cleaning as a periodontal disease control measure, as well as to afford an opportunity to use fluoride dentifrices more often in caries control. Where periodontal pockets exist, even more frequent oral hygiene procedures are indicated. Studies have been conducted in which patients were asked to brush exactly as they did at home and then covertly monitored to determine the length of time of brushing. In the last two decades, the average brushing time was shown to have increased from about 20 to 30 seconds, to 60 seconds [65,66], and to 80 seconds in a 1995 study [67]. In all of these studies, the individuals claimed that they usually brushed for 2 or 3 minutes. These results demonstrate that people greatly overestimate their efforts or else are telling their professionals what the individuals believe or would like the professionals to hear. Thorough tooth brushing requires a different amount of time for each individual, depending on such factors as the innate tendency to accumulate plaque and debris; the psychomotor skills; and the adequacy of clearance of foods, bacteria, and debris by the saliva. Only after patients have repeatedly brushed their teeth under the supervision of a dental professional can the adequacy of cleaning in a given time be determined. Often a compromise is made by suggesting 5 to 10 strokes in each area or by advocating the use of a timer. This amount of time, which might be adequate for the average person, may not be sufficient for patients in most need of maximum plaque- control programs. To ensure continued commitment to a personal oral-hygiene program, the benefits of proper oral care must be explained and demonstrated to patients [9].
Tooth Brushing Procedures
Occlusal surfaces: The occlusal surfaces may be cleaned by either (1) short vibratory strokes, with pressure being maintained to accomplish as deep a penetration of the pits and fissures as possible; or (2) a rapid back- and-forth vibrating motion to force the bristles into the pits and fissures, followed by a sweeping motion to expel the dislodged debris. Long, sweeping, horizontal strokes are contraindicated, because the toothbrush bristles have minimum contact in the deeper and more critical fissures. The orifices of the pits and fissures are too narrow for bristle penetration and, whatever the technique, are inaccessible for adequate cleaning. This helps explain why more than 60% of all carious lesions in the mouth are found on the occlusal surface, even though most individuals attempt to brush this surface.
The Anterior Lingual Areas: Access to the lingual surfaces of the mandible and maxilla is difficult. Brushing in these areas can be facilitated by cutting off all tufts on a brush, except the first four or five rows in the toe. This modified brush has unimpeded access to the gingival sulci and lingual fossae area. In the lower arch, the heel of the brush can be used for the same purpose.
Brushing Sequence
A routine brushing pattern should be established to avoid exclusion of any area. One systematic pattern is to teach children to begin by cleaning the occlusal surfaces of the maxillary arches, starting with the molars, and then the same on the mandibular arches. For children it is most important to brush the pit and fissures. The use of a three-dimensional brush can be recommended as long as children are not able to brush the more difficult buccal and lingual surfaces [68]. Such toothbrushes that hug the teeth and clean the buccal, lingual, and occlusal surfaces simultaneously are easier for children to use, as the brush guides itself from tooth to tooth. Studies show that children favor such toothbrushes. Adult patients are taught to begin with the distal surface of the most posterior tooth and to continue brushing the occlusal and incisal surfaces around the arch until the last molar on the other side of the arch has been reached. The lower arch is then brushed in a similar manner. Patients tend to apportion more time and effort on the facial areas of the anterior teeth [69]. Often, right-handed people do not brush the right side of the arch as well as the left side; left-handed people similarly neglect the left side over the right side.
Clinical Assessments of Tooth Brushing
Whatever techniques are recommended, the main purpose of tooth brushing is to remove dental plaque from the teeth, including the gingival crevice, with the minimum amount of damage to the teeth and surrounding structures. Disclosing agents provide the means of evaluating the thoroughness of cleaning the teeth [56,70]. The most widely marketed red disclosing products contain FD&C Red #28. Disclosing agents may be in either a liquid or tablet form. The chewable tablet or the liquid disclosant should be swished around in the mouth for 15 to 30 seconds and then expectorated. Home use of disclosants by the patient should be encouraged to permit self-evaluation of the effectiveness of plaque-control programs. Clinical assessments should be made for evidence of improper tooth brushing. Minor damage that may be noted includes abrasion to the soft tissues (scuffing, bruising, and punctate lesions) or damage to the tooth surface. Toothbrush abrasion, or the wearing away of tooth substances, occurs from the use of highly abrasive dentifices, too-firm brush bristles, incorrect brushing methods, and excessive pressure during brushing. Common abrasion locations are on the surfaces of the teeth displaced facially and on the cervical areas of exposed root surfaces. Because enamel is harder than cementum, tooth damage usually occurs as a V-shaped, horizontal notch immediately apical to the cementoenamel junction. Further progress of the abrasion can be minimized by use of soft-bristle brushes, changes in brush angulation, pulsing instead of stroking, the use of less abrasive dentifrices, and less pressure during brushing.
Toothbrush Replacement
Toothbrush wear (splayed, bent, or broken bristles) is influenced more by brushing methods than by the length of time or number of brushings per day [71]. The average “life” of a manual toothbrush is approximately 3 months. This estimate can vary greatly, however, because of differences in brushing habits. It is also sound advice for patients to have several toothbrushes and to rotate their daily use, to assure drying between brushings. If toothbrushes need to be replaced more frequently than every three months, the patient's brushing technique should be checked. Even if the brushing technique is acceptable or has been corrected, toothbrushes should still be replaced frequently. Indeed, after every oral or contagious medical illness, it is imperative that patients be made aware of the importance of having a new toothbrush.
Special Needs
Tongue Brushing: Malodor from the mouth most often has its origin on the tongue. Therefore, for persons expiring mouth odor, tongue brushing is important. Tongue cleaning is also indicated for patients harboring a coated tongue. A coated tongue is a bacterial reservoir but could also be a locus for intraoral transmission of organisms during toothbrushing, through infection or reinfection of periodontally treated pockets. This is another reason that Quirynen, et al. introduced the full-mouth disinfection concept in periodontal patients to prevent recolonization of bacteria [28]. The brushing of the tongue and palate helps reduce the debris, plaque, and number of oral microorganisms. The papillae on the tongue provide an area especially conducive to bacterial and debris retention. Tongue cleansing can be accomplished by placing the side of the toothbrush near the middle of the tongue, with the bristles pointed toward the throat. The brush is swept forward, and this motion is repeated six to eight times in each area. The palate should also be cleansed with a sweeping motion. A dentifrice should be used with this brushing of soft tissues to improve cleansing action [72].
Abutment teeth and orthodontic appliances: Abutment teeth, implants, fixed bridgework and fixed orthodontic appliances require special emphasis on sulcular brushing to prevent gingivitis. Thorough cleansing between orthodontic appliances and gingiva will prevent dental caries. A pre-teen or teenager, as well as patients with extensive reconstruction bridgework, are prone to dental diseases but are also more motivated; therefore, a rigid, preventive program is required. A powered brush and auxiliary aids are suggested. The effectiveness of a new toothbrush design in orthodontic patients has been documented in different publications. At the end of a 4-month study, a three-sided manual toothbrush significantly decreased gingivitis and was more effective in plaque removal compared to a flat multitufted toothbrush [73]. Powered toothbrushes have been documented to provide superior efficacy in orthodontic patients compared to results in patients using manual toothbrushes [9].
Dentures and removable orthodontic appliances: Patients with full dentures can meet their oral hygiene needs with a soft nylon brush for the oral tissues and a denture brush that cleans all areas of the denture. The denture brush with a nonabrasive cleaner should reach into the recessed alveolar ridge area of the denture to ensure maximum cleansing. The oral tissues should be brushed at least once a day using a gentle vibration and long, straight strokes from the posterior to anterior mouth regions [70]. Patients with removable partial dentures and removable orthodontic appliances need at least three toothbrushes, one for the natural teeth, another for the appliance, and a third for clasps. Brushing clasps, wires, and other metal parts can wear out a regular toothbrush. A clasp brush 2 or 3 inches long, narrow, and tapered can be obtained as a third brush. Special care is needed to carefully clean all plaque from the clasps as a preventive measure for the supporting teeth.
Handicapped patients: Some handicapped patients are able to brush their own teeth and can often do so with support and encouragement from dental personnel and the use of special toothbrushes. A manual brush with an enlarged handle, elastic cuff, or small strap attached to the brush or a long-handled holder for patients who cannot raise their arms or do not have hands, permits the patient to brush [74]. The elastic cuff is fitted around the hand and holds the toothbrush in the patient's palm. Patients who are unable to reach their mouths for brushing can, at times, attach the brush in a stationary upright position by using a clamp [75]. The patients bend over to position the brush in the mouth. The National Foundation of Dentistry for the Handicapped is developing a preventive program to encourage tooth brushing to the beat of music. A brush wheel, which can be used in between the teeth and moved through the dentiton without using the hands might be helpful for tetraplegics. The results are almost comparable with hand brushes [76,77]. Mentally retarded patients can often brush using a soft toothbrush with the plastic handle bent for better grasping. A horizontal scrub is often the best that these patients can manage. A three-headed toothbrush or a powered toothbrush assisted by a caregiver can be useful [37].
Special uses for powered toothbrushes: Powered toothbrushes can be beneficial for parental brushing of children's teeth; for children and adults who are physically handicapped, mentally retarded, aged, arthritic, or otherwise with poor dexterity; and for those patients who are poorly motivated. These brushes are especially recommended for patients who require a larger handle, because powered models are easier to grasp.
Conclusion
Tooth brushing alone cleans buccal and lingual tooth surfaces. No single tooth brushing technique adequately cleans occlusal pits and fissures. No tooth brushing procedure removes all interproximal and subgingival plaque, especially around malposed teeth and fixed prostheses. Interproximal cleaning aids are necessary to complete the tooth-cleaning process. No one toothbrush design has been demonstrated to be most effective for all patients in long-term studies. Dental professionals should be familiar with various toothbrush products, primarily from their own use experience, and have examples of toothbrushes demonstrating various degrees of splaying or bending. These should be demonstrated when prevention methods are being discussed with their patients. Although manufacturers are advertising variations in bristle shape, bristle size, and number of filaments, no accepted criteria exist for product labeling. The American Dental Association does not yet consider one toothbrush design superior to another but is developing clinical-testing guidelines associated with both plaque and gingivitis reductions. Thoroughness and frequency of brushing are probably more important than a specific tooth brushing method and tooth brushing products. Any method that is taught should be effective, not damaging to the hard or soft tissues, routinely used and should not cause excessive tooth wear. In initiating effective tooth brushing, it is necessary to (1) select the appropriate toothbrush(es) suitable for the patient; (2) instill in individuals the goals of tooth brushing and the need for good oral physiotherapy; (3) teach a technique or combination of brushing methods needed to meet special needs; and (4) assess thorough and effective tooth brushing as a part of the total oral hygiene program.
References
- Hirschfeld I (1939) The toothbrush: Its use and abuse. Brooklyn, NY: Dental Items of Interest Publishing Co., Page no: 1-591.
- Hattab FN (1997) Meswak: The natural toothbrush. J Clin Dent 8: 125-129.
- Golding PS (1982). The development of the toothbrush. A short history of tooth cleansing: Part 1. Dent Health (London) 21: 25-27.
- Smith C (2000) Toothbrush technology--Even the Pharaohs brushed their teeth. J Dent Technol 17: 26- 27.
- Yankell SL, Emling RC (1978) Understanding dental products: What you should know and what your patient should know. U Pa Cont Dent Educ 1: 1-43.
- Volpe AR, Emling RC, Yankell SL (1992).The toothbrush? A new dimension in design, engineering and clinical evaluation. J Clin Dent, 3: 29-S32.
- Mintel TE, Crawford J (1992). The search for a superior toothbrush design technology. J Clin Dent, 3: 1-4.
- Saxer UP, Yankell SL (1997) Impact of improved toothbrushes on dental diseases II. Quintessence Int, 28: 513-525.
- Saxer UP, Yankell SL (1997) Impact of improved toothbrushes on dental diseases II. Quintessence Int, 28: 573-593.
- Benson BJ, Henyon G, Grossman E (1993) Clinical plaque removal efficacy of three toothbrushes. J Clin Dent 4: 21-25.
- Volpenhein DW, Handel SE, Hughes TJ, Wild J (1996) A comparative evaluation of the in vitro penetration performance of the improved Crest Complete toothbrush versus the current Crest Complete toothbrush, the Colgate Precision toothbrush and the Oral-B P40 toothbrush. J Clin Dent 7: 21-25.
- Garcia-Godoy F (2000) A new toothbrush design. Am J Dent 13: 4.
- Chava VK (2000) An evaluation of the efficacy of a curved bristle and conventional toothbrush. A comparative study. J Periodontol 71: 785-789.
- Yankell SL, Emling RC, Shi X, Perez B (1996) A six-month evaluation of the Dentrust toothbrush. J Clin Dent 7: 106-109.
- Zimmer S, Diedner B, Roulet JF (1999) Clinical study on the plaque-removing ability of a new triple-headed toothbrush. J Clin Periodontol 26: 281-285.
- Saxer UP, Yankell SL (1997) A review of laboratory methods to determine toothbrush safety and efficacy. J Clin Dent 8: 114-119.
- Beals D, Ngo T, Feng Y, Cook D, Grau DJ, et al. (2000) Development and laboratory evaluation of a new toothbrush with a novel brush head design. Am J Dent 13: 5-14.
- Hotta M, Yoshida T, Sekine I, Imada S, Sauo A (1997) Evaluation of tapered-end toothbrush bristles regarding subgingival access efficacy. J Clin Dent 8: 156-158.
- Yankell SL, Shi X, Emling RC, Harris M (1998) Laboratory evaluation of the Reach Tooth & Gum Care toothbrush and three additional manual toothbrushes for subgingival access. J Clin Dent 9: 1-4.
- Yankell SL, Shi X, Emling RC, Loudin S, Homan G, et al. (2001) Laboratory evaluations of a toothbrush with diamond-shaped filaments for stiffness and efficacy. J Clin Dent 12: 112-115.
- Bass CC (1948) The optimum characteristics of toothbrushes for personal oral hygiene. Dent Items Int, 70: 697-718.
- Nygaard-Ostby P, Yankell SL (1981) Evaluation of the end-roundedness of toothbrushes filaments in laboratory and clinical studies. J Dent Res 60: 394.
- McLey L, Boyd RL, Sarker S (1997). Clinical and laboratory evaluation of powered electric toothbrushes: Relative degree of bristle end-rounding. J Clin Dent 8: 86-90.
- Sforza NM, Rimondini L, diMenna F, Camorali C (2000) Plaque removal by worn toothbrush. J Clin Periodontol 27: 212- 216.
- Silverstone LM, Featherstone MJ (1988) A scanning electron microscope study of the end rounding of bristles in eight toothbrush types. Quintessence Int 19: 87-107.
- Mulry CA, Dellerman PA, Ludwa RJ, White DJ, Wild TE (1992). A comparison of the end-rounding of nylon bristles in commercial toothbrushes: Crest Complete and Oral-B. J Clin Dent 3: 47-50.
- Checchi L, Minguzzi S, Franchi M, Forteleoni G (2001) Toothbrush filaments end-rounding: stereomicroscope analysis. J Clin Periodontol 28: 360-364.
- Quirynen M, De Soete M, Dierickx K, Van Steenberghe D (2001) The intraoral translocation of periodontopathogens jeopardizes the outcome of periodontal therapy. A review of the literature. J Clin Periodontol 28: 499-507.
- International Organization for Standardization (1987) Dentistry-Stiffness of the Tufted Area of Toothbrushes. References ISO 8627: 1987.
- Ring ME (1985) Dentistry: An illustrated history. The C.V.Mosby Company St. Louis, Mo, 1-319.
- Boyd RL (1997) Clinical and laboratory evaluation of powered electric toothbrushes: Review of the literature. J Clin Dent 8: 67- 71.
- Warren PR, Smith RT, Cugini M, Chater BV (2000) A practice-based study of a power toothbrush: Assessment of effectiveness and acceptance. JADA 131: 389-394.
- Haesman P (2001) Introduction to this special issue. J Clin Dent 12: 1.
- Grossman E, Dembling W, Proschkin HM (1995) A comparative clinical investigation of the safety and efficacy of an oscillating/rotating electric toothbrush and a sonic toothbrush. J Clin Dent 6: 108-112.
- Robinson PJ, Maddalozzo D, Breslin S (1997) A six-month clinical comparison of the efficacy of the Sonicare and the Braun Oral-B electric toothbrushes on improving periodontal health in adult periodontitis patients. J Clin Dent 8: 4-9.
- Yankell SL, Emling RC, Shi X (1997) Interproximal access efficacy of Sonicare Plus and Braun Oral-B Ultra compared to a manual toothbrush. J Clin Dent 8: 26-29.
- Zimmer S, Diedner B, Roulet J-F (1999) Clinical study on the plaque-removing ability of a new triple-headed toothbrush. J Clin Periodontol 26: 281-285.
- Soparkar PM, Rustogi KN, Petrone ME, Volpe AR (2000) Comparison of gingivitis and plaque efficacy of a battery- powered toothbrush and an ADA provided toothbrush. Compend Cont Educ Dent 21: 14-18.
- Rulman D, Bartizak RD, Biesbrock AR (2002) Comparative efficacy of two battery-powered toothbrushes on dental plaque removal. J Clin Dent 13: 95-99.
- Menghini G (2001) Personal communication.
- Aass AM, Gjermo P (2000) Comparison of oral hygiene efficacy of one manual and two electric toothbrushes. Acta Odontol Scand 58: 166-170.
- Gunsolley JC, Quinn SM, Tew J (1998) The effect of smoking on individuals with minimal periodontal destruction. J Periodontol 69: 165-170.
- Albander JM, Kingman A (1999) Gingival recession, gingival bleeding, and dental calculus in adults 30 years of age and older in the United States, 1988-1994. J Periodontol 70: 30-43.
- Donly KJ, Vargas M, Meckes M (1996) In vitro comparison of restoration wear and tensile strength following extended brushing with Sonicare and a manual toothbrush. J Clin Dent 8: 30-35.
- Emling RC, Yankell SL (1997) The application of sonic technology to oral hygiene: The third generation of powered toothbrushes. J Clin Dent 8: 1-3.
- Glaze PM, Wade AB (1986) Toothbrush age and wear as it relates to plaque control. J Clin Periodontol 13: 52-56.
- American Dental Association (1983). Dentist’s desk reference: Materials, instruments and equipment. Aids to oral hygiene and oral health: Powered toothbrushes (2nd ed.) Chicago, USA. Page no: 418.
- Baab DA, Johnson RH (1989) The effect of a new electric toothbrush on supragingival plaque and gingivitis. J Periodontol 60: 336-341.
- Weinstein P, Getz T, Milgrom P (1991) Oral self-care. Strategies for preventive dentistry. Why most plaque programs do not work. Univ Wash Cont Dent Educ (3rd edn) Chapter 1. Page no: 1-11.
- Nygaard-Ostby P, Edvardsen S, Spydevold B (1979) Access to interproximal tooth surfaces by different bristle designs and stiffnesses of toothbrushes. Scand J Dent Res 87: 424-430.
- Imfeld T (2001) Comparison of the mechanical effects of a toothbrush and standard abrasive on human and bovine dentin in vitro. J Clin Dent 13: 92-96.
- Council on Scientific Affairs, American Dental Association: American Dental Association Acceptance Program. Guidelines for Toothbrushes, January 1996.
- Tsamtsouris A, White CE, Clark ER (1979) The effect of instruction and supervised toothbrushing on the reduction of dental plaque in kindergarten children. J Dent Child 465: 204-209.
- Fones AC (1934) Mouth hygiene (4th ed.) Philadelphia: Lea & Febiger, 1934: 294-315.
- Leonard HJ (1939) Conservative treatment of periodontoclasia. JADA 26: 1308-1318.
- Carranza FA, Newman MG (1996) Clinical periodontology (8thedn) Philadelphia: WB Saunders Co, USA, Page numbers: 1-1033.
- Stillman PR (1932) A philosophy of the treatment of periodontal disease. Dent Dig 38: 315-319.
- Charters WJ (1948) Home care of the mouth I Proper home care of the mouth. J Periodontol 19: 136-137.
- Bass CC (1954) An effective method of personal oral hygiene, Part II. J Louisiana State Med Soc 106: 100-112.
- Gibson JA, Wade AB (1977) Plaque removal by the Bass and roll brushing techniques. J Periodontol 48: 456-459.
- Smuckler H, Landberg J (1984) The toothbrush and gingival traumatic injury. J Periodontol 55: 713-719.
- Imfeld T, Sener B, Simonovic I (2000) In vitro-untersuchen der mechanischen wirkung von handelsublichen handzahnbursten. Acta Med Dent Helv 5: 27-37
- Imfeld T, Saxer UP (2001) Anleitung zur Zahnreinigung mit elektrishen zahnbursten. Swiss Dent Soc 1-813.
- Lang KP, Cumming BR, Loe H (1973) Toothbrushing frequency as it relates to plaque development and gingival health. J Periodontol 44: 396-405.
- Emling RC, Flickinger KC, Cohen DW, Yankell SL (1981) A comparison of estimated versus actual brushing time. Pharm Therap Dent 6: 93-98.
- Saxer UP, Emling R, Yankell SL (1983) Actual vs. estimated tooth brushing time and toothbrush used. Caries Res 17: 179-180.
- Saxer UP, Barbakow J, Yankell SL (1998) New studies on estimated and actual toothbrushing times and dentifrice use. J Clin Dent 9: 49-51.
- Zimmer S (2001). Neuartige Handzahnbursten: Marketing-gag oder zahnmedizinischer fortschritt? Quintessenz Team-Journal 31: 187-192.
- Tsamtsouris A (1978) Effectiveness of tooth brushing. J Pedodontics 2: 296-303.
- Wilkins EM (1994) Clinical practice of the dental hygienist (7thedn) Philadelphia: Lea & Febiger 1-893.
- Craig TT, Montague JL (1976) Family oral health survey. JADA 92: 326-332.
- Christen AG, Swanson BZ Jr (1978) Oral hygiene: A history of tongue scraping and brushing. JADA 96: 215-219.
- Yankell SL, Greco MR, Lucash DA, Emling RC (1997) Four-month assessment of the Dentrust and Oral-B P35 toothbrushes in orthodontic patients. J Clin Dent 8: 95-99.
- Fuller L, Dunn MJ (1966) An occupational therapist’s role in oral hygiene for the handicapped. Am J Occup Therap 20: 35-36.
- Birch RH, Mumford JM (1963) Electric tooth brushing. Dent Practice 13: 182-186.
- Marthaler TM, Menghini G, Bultmann H, Ingold R (1987) Beeinflussunng der gingivalen verhaltnisse durch den gebrauch einer zahnburste oder eines kauradchens. Schweiz Monatsschr Zahnmed 97: 591-594.
- Kozlovsky A, Dreiangel A, Perlmutter S (1991) The chewing wheel device: plaque removing efficiency and use in oral hygiene programs. Quint Int 22: 727-730.
Citation: Mehta DS, Kishore A, Sharma KS, Agrawal N, Singh M, et al. (2022) Toothbrushes and Tooth Brushing Methods: A Periodontal Review. J Clin Stud Med Case Rep 9: 0129.
Copyright: © 2022 Neeraj Agrawal, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

