
Transarterial Embolization of a Hepatic Pseudoaneurysm with Hemobilia
*Corresponding Author(s):
Canales RosaResident Doctor, General Surgery, Cayetano Heredia National Hospital, Lima, Peru
Tel:+51 972732795,
Email:rosacanalesc@hotmail.com
Abstract
We report a case of severe hemobilia due to a Right Hepatic Artery Pseudoaneurysm (RHAP) occurring 4 months after a laparoscopic converted to open cholecystectomy. The abdominal CT, ultrasound and an endoscopic retrograde cholangio pancreatography strongly suggested a RHAP. Our patient underwent a new open laparotomy; however, active bleeding recurred. The patient became hemodynamically unstable and received several globular units to avoid hypovolemic shock. A celiac trunk angiography confirmed a RHAP. Using a coaxial technique, geometry guided microcatheter reached a stable position in close proximity to the RHAP and an embolic mixture of n-butyl cyanoacrylate dissolved in lipiodol was injected achieving a successful deconstructive obliteration of both RHAP and RHA. Our patient made an uneventful and rapid recovery.
Keywords
ABBREVIATIONS
RHAP: Right Hepatic Artery Pseudoaneurysm
INTRODUCTION
CASE PRESENTATION
 Figure 1: Upper digestive tract endoscopy showing a massive fresh clot coming out the ampulla of Vater.
Figure 1: Upper digestive tract endoscopy showing a massive fresh clot coming out the ampulla of Vater.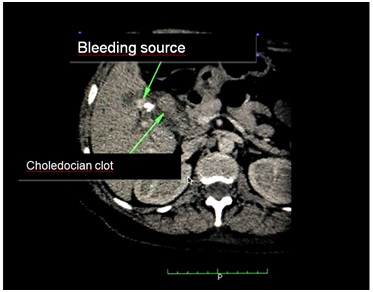 Figure 2: Non contrast CT scan showing the bleeding focus close to the surgical clips and liver hilium region (punto de sangrado) and a large clot in the choledocus lumen (coagulo coledociano).
Figure 2: Non contrast CT scan showing the bleeding focus close to the surgical clips and liver hilium region (punto de sangrado) and a large clot in the choledocus lumen (coagulo coledociano).|
Date |
15/08 |
18/08 |
25/08 |
|
Hemoglobin (g/dL) |
3.7 |
10.4 |
10.0 |
|
MCV / mch (fl / pg) |
83/26 |
85/29 |
92/30 |
|
Leucocytes (cEl/ul) |
4.41 |
11.09 |
9.6 |
|
RODS |
0 |
0 |
|
|
Segmented |
54 |
67 |
|
|
Platelets x 103 (cél/ul) |
269 |
190 |
312 |
|
Inr |
1.15 |
1.08 |
|
|
TTPa (sec) |
30.9 |
||
|
Urea / creatinine (mg/dl) |
45/0.6 |
25.9/ |
|
|
Proteins / albumin (g/dl) |
5.3/2.7 |
4.8/2.3 |
6.6 |
|
Bilirubin tot / dir (mg/dl) |
2.1/1.5 |
5.0/3.9 |
0.8/0.7 |
|
got / pgt (ui/l) |
218/124 |
49/72 |
32/34 |
|
Alkaline Phosphatase / ggtp (ui/l) |
467/440 |
215/224 |
252/162 |
DISCUSSION
The pathogenesis of a pseudoaneurysm of the hepatic and cystic arteries probably relates to disruption of the arterial wall related to mechanical and/or thermal vascular injury due to electrocautery and or to bile leakage with chemical injury related to surgical dissection at the infundibulum of the gallbladder [4-11]. If the pseudoaneurysm communicates with the biliary tree, the patient will present with hemobilia.
Hemobilia presents the triad of Quincke; gastrointestinal bleeding, abdominal pain and jaundice. The intensity of the symptoms may vary from mild pain, anemia with or without slight jaundice to massive, life threatening gastrointestinal bleeding [12-14]. The probability and severity of the bleeding correlates directly with the size of the pseudoaneurysm [9,12-15].
A recent surgical history and the clinical picture of hemobilia should prompt to endoscopy with retrograde endoscopic cholangiography, however it is often inconclusive [6,16]. Imaging studies such as Spiral CT and or ultrasound may reveal signs of the aneurysm [10,17-21]. The gold standard for the diagnosis is a visceral angiography [1,13,14,22].
Transarterial embolization is the first therapeutic option in case of a severe or recurrent bleeding and has a success rate of 80 to 100% with a few complications [1,14,22,23]. In case of compression of the bile duct or a fistula or failure from embolization, open surgery should be performed to ligate the affected artery [17]. In our patient, surgical ligature of the right hepatic artery was presumably performed, probably a branch, without occluding the main trunk of the RHA that harbored the pseudoaneurysm which led to recurrent bleeding that prompted embolization. Among the limitations of embolization are anatomical variations of the hepatic artery and recanalization of the aneurysm [24]. Hepatic artery embolization risks are hepatobiliary necrosis, bleeding, abscess formation and gallbladder fibrosis [24]. In case of embolization failure, open surgery for hemobilia is indicated [24,25].
In the scenario of hemobilia after laparoscopic cholecystectomy, a hepatic artery aneurysm must be strongly suspected, angiographically confirmed and embolized. If embolization fails, surgical intervention should be performed. This report aims to contribute to the awareness of the surgical community on the diagnosis and treatment of this infrequent situation and to highlight the relevance of endovascular embolization.
Among the therapeutic alternatives to occlude an aneurysmal sac, we have the reconstructive technique which uses metal coils or coated stents, and the deconstructive technique in which it is embolized by injecting occluding substances.
We decided for the second option before the difficult geometry of the celiac trunk that prevented the advance of our microcatheter guide towards the RHA and we used n-butyl cyanoacrylate plus lipiodol for its wide availability and lower cost in our environment as well as for our experience with this mixture in thousands of brain and systemic injuries. Particulate materials such as PVA, gel foam and others can only occlude the distal arteriolocapillary bed, but not large arteries, such as the RAE, which can increase the pressure of the stump and induce new hemorrhages.
REFERENCES
- Rivitz SM, Waltman AC, Kelsey PB (1996) Embolization of an hepatic artery pseudoaneurysm following laparoscopic cholecystectomy. Cardiovasc Intervent Radiol 19: 43-46.
- Fullarton GM, Bell G (1994) Prospective audit of the introduction of laparoscopic cholecystectomy in the west of Scotland. West of Scotland Laparoscopic Cholecystectomy Audit Group. Gut 35: 1121-1126.
- Peters JH, Ellison EC, Innes JT, Liss JL, Nichols KE, et al. (1991) Safety and efficacy of laparoscopic cholecystectomy. A prospective analysis of 100 initial patients. Ann Surg 213: 3-12.
- Balsara KP, Dubash C, Shah CR (1998) Pseudoaneurysm of the hepatic artery along with common bile duct injury following laparoscopic cholecystectomy. A report of two cases. Surg Endosc 12: 276-277.
- Milburn JA, Hussey JK, Bachoo P, Gunn IG (2007) Right Hepatic Artery Pseudoaneurysm Thirteen Months Following Laparoscopic Cholecystectomy. Eur J VascEndovasc Surg 13: 1-3.
- Parthenis DG, Skevis K, Stathopoulos V, Bellenis I, Vassilakopoulos T (2009) Postlaparoscopic Iatrogenic Pseudoaneurysms of the Arteries of the Peritoneal and Retroperitoneal Space: Case Report and Review of the Literature. Surg Laparosc Endosc Percutan Tech 19: 90-97.
- Moses V, Keshava SN, Wann VC, Joseph P, Sitaram V (2008) Cystic artery pseudoaneurysm after laparoscopic cholecystectomy presenting as haemobilia: a case report. Trop Gastroenterol 29: 107-109.
- Yao CA, Arnell TD (2010) Hepatic artery pseudoaneurysm following laparoscopic cholecystectomy. Am J Surg 199: 10-11.
- Rhee JW, Bonnheim DC, Upson J (1987) Cystic artery pseudoaneurysm. N Y State J Med 87: 47.
- Ribeiro A, Williams H, May G, Fulmer JT, Spivey JR (1998) Hemobilia due to hepatic artery pseudoaneurysm thirteen months after laparoscopic cholecystectomy. J Clin Gastroenterol 26: 50-53.
- De Molla Neto OL, Ribeiro MA, Saad WA (2006) Pseudoaneurysm of cystic artery after laparoscopic cholecystectomy. HPB (Oxford) 8: 318-319.
- Bulut T, Yamaner S, Bugra D, Akyuz A, Acarli K, et al. (2002) False Aneurysm of the Hepatic Artery after Laparoscopic Cholecystectomy. Acta Chir Belg 102: 459-463.
- Cheung HY, Tang CN, Fung KH, Li MK (2007) Bleeding pseudoaneurysms complicating upper abdominal surgery. Hong Kong Med J 13: 449-452.
- Liu TT, Hou MC, Lin HC, Chang FY, Lee SD (2003) Life-threatening hemobilia caused by hepatic artery pseudoaneurysm: A rare complication of chronic cholangitis. World J Gastroenterol 9: 2883-2884.
- Khan MR, Raza R, Salam B (2011) Leaking pseudoaneurysm of hepatic artery: A potentially life-threatening complication of a common procedure. J Pak Med Assoc 61: 504-506.
- Nicholson T, Travis S, Ettles D, Dyet J, Sedman P, et al. (1999) Hepatic Artery Angiography and Embolization for Hemobilia Following Laparoscopic Cholecystectomy. Cardiovasc Intervent Radiol 22: 20-24.
- Siablis D, Tepetes K, Vasiou K, Karnabatidis D, Perifanos S, et al. (1996) Hepatic artery pseudoaneurysm following laparoscopic cholecystectomy: transcatheter intraarterial embolization. Hepatogastroenterology 43:1343-1346.
- Clements WD, Wilson RH, Crothers JG, McIlrath EM, Johnston GW (1993) Pseudoaneurysm of the cystic artery following cholecystectomy. J R Coll Surg Edinb 38: 348-349.
- Nakajima M, Hoshino H, Hayashi E, Nagano K, Nishimura D, et al. (1996) Pseudoaneurysm of the cystic artery associated with upper gastrointestinal bleeding. J Gastroenterol 31: 750-754.
- Saldinger PF, Wang JY, Boyd C, Lang E (2002) Cystic artery stump pseudoaneurysm following laparoscopic cholecystectomy. Surgery 131: 585-586.
- Strickland SK, Khoury MB, Kiproff PM, Raves JJ (1991) Cystic artery pseudoaneurysm: a rare cause of hemobilia. Cardiovasc Intervent Radiol 14: 183-184.
- Maeda A, Kunou T, Saeki S, Aono K, Murata T, et al. (2002) Pseudoaneurysm of the cystic artery with hemobilia treated by arterial embolization and elective cholecystectomy. J Hepatobiliary Pancreat Surg 9: 755-758.
- Christensen TL, Matsuoka L, Heestand G, Palmer S, Mateo R, et al. (2006) Iatrogenic Pseudoaneurysms of the Extrahepatic Arterial Vasculature: Management and Outcome. HPB (Oxford) 8: 458-464.
- Sibulesky L, Ridlen M, Pricolo VE (2006) Hemobilia due to cystic artery pseudoaneurysm. Am J Surg 191: 797-798.
- Golich J, Rilinger N, Brado M, Huppert P, Vogel J, et al. (1999) Non-operative management of arterial liver hemorrhages. Eur Radiol 9: 85-88.
Citation: Canales R, del Castillo M, García-Encinas C, Plasencia A, Sierralta D, et al. (2018) Transarterial Embolization of a Hepatic Pseudoaneurysm with Hemobilia. J Angiol Vasc Surg 3: 012.
Copyright: © 2018 Canales Rosa, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

