
Transplanting a Polycystic Kidney; Trojan Horse or Silver Lining
*Corresponding Author(s):
Mohammad AbuzeinehDepartment Of Medicine, Johns Hopkins University School Of Medicine, Transplant Nephrology Fellow, Baltimore, United States
Tel:+1 4106140081,
Email:m_abuzainah@hotmail.co.uk/ mabuzai1@jhmi.edu
Abstract
Renal transplant, when possible, is the treatment of choice for patients with advanced renal failure approaching End Stage Renal Disease (ESRD). Unfortunately, there is a significant gap between supply and demand for available kidney transplants. With the 2014 updated Kidney Allocation System (KAS), patients with older age have shorter expected post-transplant survival, thus have less chances to get transplanted. In this case report, we describe a 76 year-old male who underwent a successful deceased renal transplant from a donor who had known Autosomal Dominant Polycystic Kidney Disease (ADPKD). His chances of having an “ordinary” kidney were low; hence we opted to offer him a rather “unordinary” kidney, which was successfully transplanted with near normal post-transplant renal allograft function. This case report presents a silver lining for aging ESRD population, with a chance to improve their survival and quality of life by keeping them off dialysis.
Keywords
Polycystic kidney; Renal transplant
BACKGROUND
As of April 2020 there were almost 95,000 candidates awaiting kidney transplants in the United States [1]. The median wait time for an individual’s first kidney transplant is close to four years and can vary depending on health, compatibility and availability of organs. There is a significant gap between supply and demand for kidney transplants. For example, in year 2016, 19,061 kidney transplants took place in the United States, however, there were 124,675 newly reported cases of End Stage Renal Disease (ESRD) and there were total 726,331 prevalent cases of ESRD [2]. ESRD aging population (>75 years) is a growing population in the United States (Figure 1). However, they have fewer chances to get a kidney transplant. Thus, our 76 year old patient had a rather unusual, but successful kidney transplant from a deceased donor who had known Autosomal Dominant Polycystic Kidney Disease (ADPKD).
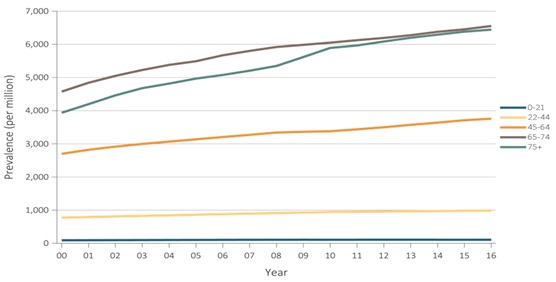 Figure 1: Standardized prevalence of ESRD, by age group, in the U.S. population, 2000-2016.
Figure 1: Standardized prevalence of ESRD, by age group, in the U.S. population, 2000-2016.
Source: USRDS [2].
CASE PRESENTATION
Recipient
A 76 year old Caucasian male with long standing Chronic Kidney Disease (CKD) presumed to be secondary to prior analgesic use was referred to transplant center by his primary nephrologist after discussion about risk and benefits of dialysis Vs transplant in old age. Patient had been in stage 5 of CKD for one year prior to transplant. At his last follow up visit before transplant, he reported increasing fatigue, loss of appetite and decided to see a surgeon for peritoneal dialysis catheter placement. His labs at that visit showed a Blood Urea Nitrogen (BUN) of 61 mg/dl, Creatinine (Cr) 4.63 mg/dl with an estimated Glomerular Filtration Rate (eGFR) of 12 mL/min. A few days later, the transplant center called him with an offer for kidney. His Estimated Post-Transplant Survival (EPTS) score was 70%.
Donor
27 year old male, victim of gunshot wound and head trauma, who was pronounced brain dead the day after the incident, was known to have ADPKD since childhood and was followed by a nephrologist. He also had a history of hypertension and was non-compliant with medications. His family history was significant for ADPKD and ESRD with multiple family members on dialysis. Donor's Cr had been 1.2 mg/dl a year before with eGFR of 78 mL/min and no proteinuria. Prior data showed Cr value 0.8 mg/dl four years before and 1.0 mg/dl two years before the incident. Donor's Cr went from 1.2 mg/dl on admission up to 1.8 mg/dl, but improved back to 1.17 mg/dl. Infectious disease workup was negative. Donor was negative for Cytomegalovirus (CMV) and the recipient was positive for CMV. Kidney biopsy showed the left kidney to have 12% glomerulosclerosis with minimal to mild arterial/arteriolar damage, mild interstitial fibrosis and mild inflammatory processes along with several small microcytic structure with diffuse and dilated tubules. Right kidney showed 3% glomerulosclerosis with minimal to mild arterial/arteriolar damage, mild interstitial fibrosis and mild inflammatory processes along with dilated tubules, small sub capsular cyst and rare microcytic structures. Recipient’s Panel Reactive Antibody (PRA) was 0% and donor’s Kidney Donor Profile Index (KDPI) was 17%. Cold ischemic time was 15.25 hours.
Post-transplant course
The recipient received the left kidney. Patient’s post-transplant Cr improved from 4.7 mg/dl to 1 mg/dl in 5 days. He received thymoglobulin and steroids for induction and was later started on mycophenolate mofetil and tacrolimus for maintenance immunosuppression per protocol. Bactrim, valganciclovir and clotrimazole were started for infection prophylaxis as per routine protocol. On postoperative day four, he developed acute left sided weakness with facial droop. A Magnetic Resonance Image (MRI) of brain revealed watershed type bilateral infarcts and neurology was consulted. He was discharged to rehab where he developed acute upper gastrointestinal bleed. Upper endoscopy revealed a gastric ulcer. He did well thereafter and outpatient follow up showed good graft function with patient’s serum Cr of 1.28 mg/dl at 3 months post-transplant and 1.20 mg/dl at 6 months post-transplant.
DISCUSSION
The Organ Procurement and Transplantation Network (OPTN)’s Kidney Allocation System (KAS) was changed on December 2014. Lower Kidney Donor Profile Index (KDPI) kidneys are associated with better post-transplant survival. Similarly, transplant candidates on the waiting list are risk-stratified based on Estimated Post-Transplant Survival (EPTS), which takes into account candidate age, dialysis duration, prior solid organ transplant and diabetes status [3]. Generally, older age, longer dialysis duration, prior solid organ transplant and presence of diabetes are associated with higher EPTS scores and shorter expected post-transplant survival [3]. Figure 1 shows the increasing number of patients with ESRD who are of 75 years of age or more [2]. Table 1 shows that kidney transplant rates among patients who are 75 years or more are extremely lower when compared to younger age groups (on 2016 was 0.3 per 100 dialysis patient-years) [2]. With high demand for kidney transplants, 76 years old with “higher” EPTS score, the chance for “ordinary” kidney transplant is diminished. That being said, our patient had the chance for “unordinary” kidney transplant from deceased donor with known ADPKD which was successful.
|
Age |
2007 |
2008 |
2009 |
2010 |
2011 |
2012 |
2013 |
2014 |
2015 |
2016 |
|
0-21 |
31.6 |
32.5 |
34.7 |
32.8 |
32.0 |
32.5 |
31.6 |
31.9 |
33.4 |
34.4 |
|
22-24 |
9.5 |
8.8 |
8.7 |
8.1 |
7.7 |
7.6 |
7.3 |
7.2 |
8.6 |
8.5 |
|
45-64 |
5.4 |
5.1 |
4.9 |
4.8 |
4.5 |
4.2 |
4.3 |
4.1 |
4.0 |
4.3 |
|
65-74 |
2.5 |
2.6 |
2.6 |
2.6 |
2.6 |
2.5 |
2.4 |
2.4 |
2.2 |
2.4 |
|
> 75 |
0.4 |
0.3 |
0.4 |
0.4 |
0.4 |
0.4 |
0.3 |
0.4 |
0.3 |
0.3 |
Table 1: Unadjusted kidney transplant rates, all donor types, by age per 100 dialysis patient-years, 2007-2016.
Source: USRDS [2].
ADPKD occurs worldwide and in all races with an estimated incidence of 1 in 500 to 1 in 1000, with most patients presenting in third to fifth decade. Once they develop CKD, eGFR typically declines 4.4-5.9 ml/min/year and ESRD usually occurs within 5 to 10 years after developing CKD [4]. Kidneys from donors affected by ADPKD are, in general, considered unsuitable for transplantation. Although not part of Expanded Criteria Donors (ECD) (ECD is defined as any brain-dead donor aged > 60 years or a donor aged > 50 years with 2 of the following conditions: history of hypertension, terminal serum Cr level > or = 1.5 mg/dL, or death resulting from a cerebrovascular accident) [5], our case’s donor kidney did not fall under the Standard Criteria Donor (SCD) either, given the nature of the kidney (polycystic) and hypertension in donor.
Shamali et al. [6], reviewed a case series of 16 ESRD patients who had renal transplants from donors with ADPKD, which showed encouraging results with median post-transplant serum Cr at 1.40 mg/dl and 13 out of the 16 patients had functioning grafts at median graft follow up of 36 months .This case presentation adds up to the successful cases of polycystic kidney transplantation from donors with ADPKD, with very good post-transplant graft function as shown by 6 month post-transplant Cr of 1.20 mg/dl.
This case report presents a silver lining and an appealing option especially for ESRD patients with older age and/or lower life expectancy. Transplanting a polycystic kidney with donor of younger age, smaller kidney size, and preserved renal function seems to be a very reasonable option and should be discussed and assessed by experienced transplant team and if found suitable, to explain in depth the risks/benefits with the patient and get fully informed consent. Moreover, in post-transplant period, specific considerations related to the polycystic kidneys should be kept in mind, such as complications related to the cysts (i.e. rupture, hemorrhage and stone formation), polycythemia and future risk of malignancy.
CONCLUSION
The limited availability of donors and kidneys for transplant is a significant challenge especially for aging ESRD population in the U.S. Carefully selected renal allografts from deceased donors with ADPKD are reasonable and appealing option for elderly ESRD population or those with reduced life expectancy. In post-transplant period, extra attention should be sought for potential complications related to the polycystic renal allograft.
AUTHOR CONTRIBUTIONS
Dr. Abuzeineh had full access to all the data in the case report and takes responsibility for the integrity of the data. Drafting of the manuscript: Dr. Abuzeineh, Dr. Dalal and Dr. Malhotra.
CONFLICT OF INTEREST/DISCLOSURES
None
REFERENCES
- S. Department of Health & Human Services. Organ Procurement and Transplantation Network. Virginia, USA.
- United States Renal Data System. Minneapolis, USA.
- Israni AK, Salkowski N, Gustafson S, Snyder JJ, Friedewald JJ, et al. (2014) New national allocation policy for deceased donor kidneys in the United States and possible effect on patient outcomes. J Am Soc Nephrol 25: 1842-1848.
- Torres VE, Harris PC (2009) Autosomal dominant polycystic kidney disease: The last 3 years. Kidney Int 76: 149-168.
- Pascual J, Zamora J, Pirsch JD (2008) A systematic review of kidney transplantation from expanded criteria donors. Am J Kidney Dis 52: 553-586.
- Shamali A, Milsom-Mcquillan S, Gibbs P (2018) Outcomes of renal transplant from donors with polycystic kidney disease. Int J Surg 51: 229-232.
Citation: Abuzeineh M, Dalal P, Malhotra K (2020) Transplanting a Polycystic Kidney; Trojan Horse or Silver Lining. J Nephrol Renal Ther 6: 027.
Copyright: © 2020 Mohammad Abuzeineh, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

