
Treatment of Irritable Bowel Syndrome with Auricular Acupuncture: A controlled pilot study
*Corresponding Author(s):
Antonello LovatoAIRAS (Italian Association For The Research And The Scientific Update), Padua, Italy
Tel:+39 0444832740,
Email:lovatoantonello@gmail.com
Abstract
Introduction: Irritable Bowel Syndrome (IBS) is a chronic gastrointestinal condition. Auricular Acupuncture (or AA) is a treatment option for IBS though literature is scanty for evidence on its effectiveness.
Objective: Evaluate if AA is a viable treatment for IBS and which between 2 different AA treatment protocols gives the best results from IBS patients perspective on single specific symptoms.
Materials and Methods: A total of thirty-four IBS subjects underwent four sessions of AA. Six evaluations were done with a questionnaire rating from 0 to 10 the extent of symptoms diarrhoea, constipation, meteorism, abdominal pain and food tolerance.
Results: Both protocols achieved positive results. Group A obtained best results for meteorism and good for abdominal pain while Group B best for diarrhoea, constipation and abdominal pain with good for meteorism. No results for food intolerance were obtained.
Discussion: Overall, group B obtained better results than group A, contrary to expectation.
Conclusion: AA is a viable treatment of IBS and Group B protocol could be a first approach of AA treatment in IBS. Nonetheless, protocol choice must be based more on results from clinical trials and less on theoretical AA reasoning.
Keywords
Auricular Acupuncture; Ear Acupuncture; Irritable Bowel Syndrome; IBS
Introduction
Irritable Bowel Syndrome (IBS) is a chronic gastrointestinal condition belonging to the field of functional bowel disorders. IBS is classified using the Rome IV criteria and is characterized by abdominal pain associated with alterations of bowl movement frequency and of stool characteristics such as shape and consistency [1]. Disorders related to this condition are recurrent, so much so that 50% of patients require a specialist evaluation [2].
The etiopathogenesis has not been yet fully understood though it has been acknowledged to be multifactorial since alterations in visceral motility and sensitivity and of the visceral stimuli analysis done by the central nervous system are involved. More recently, alterations in intestinal microbiota, gastrointestinal immune system and intestinal permeability have been acknowledged to be possible etiological factors for IBS.
IBS mainly affects the developed world, mostly women and predominantly people of working age. In Italy it has been estimated that IBS affects 1 in 10 subjects, mostly women aged between 20 and 50 years of age [3].
IBS is classified in four subgroups based on frequency of bowel movement, namely: IBS-C (where Constipation is most common), IBS-D (where diarrhoea is most common), IBS-M (where both are common) and IBS-U (or Unclassified), respectively [4].
In 77% of cases patients have a moderate or severe form of IBS based on self-reported gastrointestinal symptoms. The latter appears to be associated to extra-intestinal symptoms with a degree of perceived disability and illness-related behaviours that cause limitations to daily activities [5].
As a matter of fact, it has been calculated that a patient with IBS tends to have double as many workplace absences as compared to an unaffected subject. In the United States and the United Kingdom, on average, a patient with IBS was absent from work for 8.5 to 21.6 days per year [6]. In Denmark, the average cost per patient with IBS due to absence from work was estimated at 1.508 USD per year [7]. In 2013 a European study conducted in 6 European countries documented that in Italy the annual healthcare cost per patient with IBS-C was 937 Euros (of which 485 Euros were patient out-of-pocket expenses since not all healthcare costs are refunded) [3].
It follows that the impact of IBS on quality of life is important even though an exact measurement is difficult due to variability in between different nations. In a 2017 study involving 1094 patients with IBS-D it emerged that 52% had to either cancel commitments at the last moment or (still in the same percentage) avoid eating before or during social commitments for fear that they could trigger IBS symptoms [8].
IBS therapy is too multifaceted, including use of symptomatic therapy (i.e., antispasmodic drugs, anti-diarrheal drugs or osmotic laxatives) together with an approach characterized by counselling concerning patient education to promote a healthy lifestyle that involves both nutritional aspects and creating healthy habits and routines. In the last decade prescription of symptomatic drugs that act both on constipation and pain have been implemented. Considering that, though it does not modify life expectancy, IBS significantly limits quality of life and reduces the performance of affected subjects. However, as documented by an analysis recently promoted by a pharmaceutical company, an ideal therapy for IBS has not yet been made available [9].
The most important databases show that acupuncture has been taken into consideration as a treatment of IBS with relative delay. The oldest study available on PubMed about acupuncture for IBS treatment dates back to 1986 since then only 288 publications have been registered.
Publications on acupuncture as a treatment option in gastroenterology concern a whole series of disturbances that could be related to IBS, for example constipation in the elderly [10], pharyngeal globe [11] and dysphagia [12]. The result of a 2019 meta-analysis, that included 41 randomized controlled trials for a total of 3440 patients, hypothesized a complementary role for acupuncture as compared to conventional medical therapy for IBS treatment [13], which appeared promising.
Transcutaneous Auricular Vagal Nerve Stimulation (or t-VNS) has been shown to be effective in reducing pain and improving constipation symptoms in IBS-C patients. Results suggest a significant improvement in rectoanal inhibitory reflex (or RAIR) and rectal sensation with a lower volume of rectal distension needed to elicit RAIR even though the rectum is not innervated by the vagus nerve [14].
In a similar paper, t-VNS described improved colon transit reducing constipation [15]. Recently it has been shown that auricular therapy and specifically t-VNS presented an anti-nociceptive effect on visceral pain associated with a reduction of hypersensitivity in subjects with acid-induced esophageal pain [16].
Literature is scarce as regards evidence on effectiveness of Auricular Acupuncture (or AA) therapy for IBS. AA textbooks propose AA IBS treatments based on the AA clinical experience and theoretical knowledge of their authors. There is a need for more studies to evaluate if AA could be a viable option for IBS treatment. Furthermore, the assessment and comparison of different given AA IBS treatment protocols is needed to evaluate if there can be a specificity to AA IBS treatment protocols that could produce the best results on given specific IBS symptoms in different IBS subgroups.
Objective
Primary objective is to evaluate if Auricular Acupuncture (or AA) can be a viable option as treatment for IBS through the analysis of results obtained from the perspective of IBS patients treated with AA IBS treatment protocols on single specific IBS symptoms.
Secondary objective is to evaluate 2 different AA treatment protocols as regards best results obtained from the perspective of IBS patients of modification of single specific IBS symptoms.
Materials And Methods
Thirty-four consecutive subjects with a diagnosis of IBS were enrolled regardless of diagnosed IBS classification.
Exclusion criteria were: needle phobia, ongoing autoimmune condition, ongoing demyelinising condition, ongoing treatment with antidepressants and/or benzodiazepines, recent IBS diagnosis (i.e., less than 24 months) and being pregnant.
Inclusion criteria were: age older or equal to 18 years, IBS diagnosis done by a specialist, willingness to do AA and to fill out the evaluation questionnaires at follow-ups.
All subjects gave written informed consent for study participation.
Baseline demographic data was collected, including: age, gender, anthropometric data and type of IBS.
Furthermore, data was collected on diagnostic procedures carried out due to IBS (i.e., colonoscopy, abdominal echography, Esophagogastroduodenoscopy, other and any combination of these).
Eligible subjects were allocated in 1 of 2 groups by assigning a number to each subject in a progressive order. Subjects with an odd number were placed in group A while those with an even number were placed in group B.
Subjects in both groups underwent AA on both auricles, starting from the left auricle without considering subject’s laterality.
As reference for AA point detection and identification and AA areas of the auricle, Terry Oleson's nomenclature and 24 auricular landmarks were used (where the whole auricle is divided into proportional areas that are comparable throughout subjects, similarly to how somatic acupuncture points are identified using the anatomical references and the “cun” measurement for distance reference [17,18] (Figure 1).
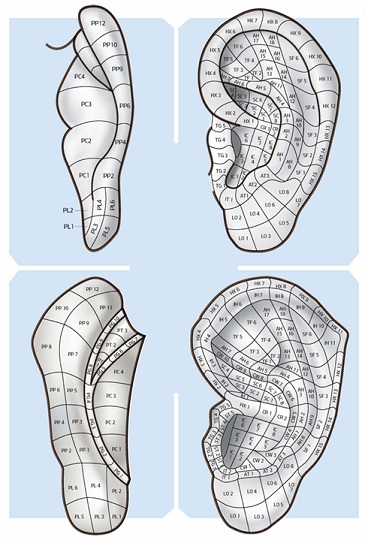 Figure 1: Lateral and medial surface of the auricle by A. Lovato: Agopuntura Auricolare teoria e clinica, NOI Ed 2019; with the division into areas according to the nomenclature of T. Oleson.
Figure 1: Lateral and medial surface of the auricle by A. Lovato: Agopuntura Auricolare teoria e clinica, NOI Ed 2019; with the division into areas according to the nomenclature of T. Oleson.
AA points were searched and identified evaluating baroesthetic sensitivity using Pain Pressure Test (or PPT) with a Sedatelec Palpeur® [19]. Semi-permanent AA needles were then positioned and left in place for five days and subsequently self-removed by the subjects. Patients were asked to massage the needle using the index-thumb technique three times a day [18]. Particular attention was paid to the sequential order of the insertion of the needles. Semi-permanent needles type SEIRIN New PYONEX® 0.20 x 0.90 mm were used on all patients for AA.
All subjects underwent a total of four sessions of AA therapy, with 15 days in-between sessions. Treatment protocols for group A and group B are described as follows. Points were treated in the same order they are named
Group A: On the left ear the “Relax Triad”, as proposed by Kovacs, was carried out [20]. Namely the Shen Men point [TF2], the Master Sensory Point [LO4] and the Prime Zero or corpus callosum [TG2-TG4] were identified and treated, together with the Large Intestines (or LI) point [SC3-SC4] (i.e., in the superior hemi-concha) as an additional point. On the right ear only the LI point [SC3-SC4] was identified and treated (Figure 2).
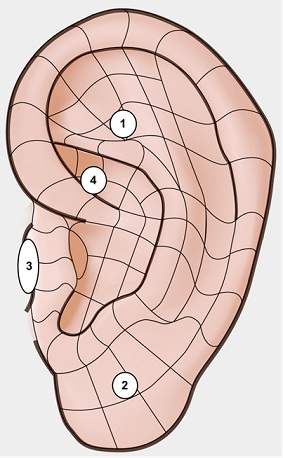 Figure 2: Left Ear: 1 Shen Men, 2 Master Sensorial Point, 3 Corpus Callosum or 0’, 4 Large Intestine; Right Ear: 4 Large Intestines.
Figure 2: Left Ear: 1 Shen Men, 2 Master Sensorial Point, 3 Corpus Callosum or 0’, 4 Large Intestine; Right Ear: 4 Large Intestines.
The “Relax Triad” has been described to help the patient perceive a general feeling of relaxation together with a reduction of anxiety, a modulation of the autonomic sympathetic system and a positive effect on surrounding environment perception (as could be pain) [21,22].
The LI point was added to this AA treatment protocol since it was always identified being tender to PPT (i.e., identified as the activated reflex point associated with the subject’s medical issue and therefore specific for colon pathologies).
Group B: On both left and right auricles two points were identified and treated, namely the point Zero [CR1-HX1] and the LI point [SC3-SC4] (Figure 3).
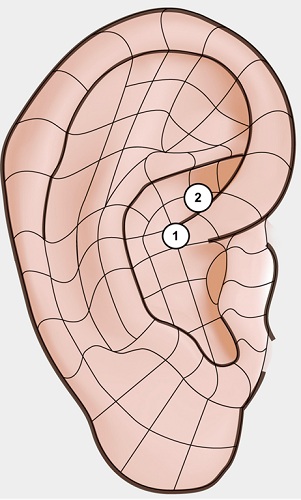 Figure 3: Left and Right Ear: 1 Point Zero, 2 Large Intestines.
Figure 3: Left and Right Ear: 1 Point Zero, 2 Large Intestines.
Point Zero is classified with Shen Men as the primary master points. Point Zero has been used since the French AA school identified it as a master point that regulates general “homeostasis, producing a balance of energy, a balance of hormones, and a balance of brain activity. It supports the actions of other auricular points and returns the body to the idealized state” [23].
Evaluation was performed at each AA session (namely T0, T1, T2 and T3) and at 2 follow-up sessions (namely T4 and T5). Follow-up was carried out at 15 days and 1 month after AA treatment, respectively. Evaluation consisted of answering a questionnaire to rate the extent of symptoms. Rating was given with a number from 0 to 10 where 0 meant no symptom and 10 the maximum discomfort/disturbance endured by the subject. A total of six evaluations were produced by each subject. At T0 the questionnaire was completed during physician evaluation where all questions and critical points brought forth by the patient were answered. T0 was considered a baseline for evaluation for all subjects of both groups. Following questionnaires were self-administered. All questionnaires were filled out before treatment session for T0 to T3. Symptoms rated by subjects were diarrhoea, constipation, meteorism (including abdominal bloating/distention), abdominal pain and food intolerance (i.e., limitations on diet and eating or need to restrict diet or IBS issues due to diet).
Statistical Analysis
Selection of statistical tools for data analysis was based on assumption of normality for data distribution. The tests used were one-way ANOVA, paired samples t-test and Chronbach alpha. The Cronbach's alpha was used to analyse internal coherence of evaluations carried out both within the session (i.e., a comparison of responses given by subjects in each different evaluation session) and in relation to the overall coherence of the data. A one-way ANOVA and a paired samples t-test allowed to compare two or more groups of data by comparing the internal variability of these groups with the variability in between the two groups. A t-test was carried out to evaluate if there was a statistically significant difference between T0 and T3 (i.e., before treatment and at the last treatment session), T0 and T5 (i.e., before treatment and at the last follow-up session), and T3 and T5 (i.e., before treatment and at the last follow-up session), respectively.
Results And Statistical Analyses
A total of 34 subjects were recruited and completed all treatment sessions and evaluation sessions for the study. Of the 34 subjects, 17 were assigned to group A and 17 to group B, respectively. 79.41% of subjects were female, while only 20.59% were male. Similar gender proportions were found in the two groups. The age variable showed a mean of 44 years (D.S. ± 9.9 years), where a slightly higher value is observed in Group A (44.5 years with SD ± 9.6 years) if compared to Group B (43.5 years with SD ± 10.5 years) (Table 1).
|
|
Obs |
Mean |
SD |
Min |
Max |
|
Total |
34 |
44 |
±9.9 |
26 |
61 |
|
Group A |
17 |
44.5 |
±9.6 |
26 |
60 |
|
Group B |
17 |
43.5 |
±10.5 |
27 |
61 |
Table 1: Age variable for all patients and for groups A and B.
As regards diagnostic procedures carried out due to IBSD a total 54 were counted. Nevertheless, 10 subjects denied having done afore mentioned diagnostic procedures. A mean of 2.25 diagnostic procedures undertaken by each of the remaining 24 subjects was calculated. The most frequent diagnostic procedures related to IBS was found to be colonoscopy and abdominal ultrasound.
Cronbach's alpha gave values always resulting greater than 0.90, thus validating the excellent reliability of data collected. Overall, the value was equal to 92.10% of reliability. For the statistical analysis we used the one-way Anova test. Each symptom was analysed as follows.
Diarrhoea
Rating of symptom Diarrhoea overall (i.e., combined data of group A and group B) did not show much change from T0 to T5 though with a slight decrease towards the last evaluations, with an average rating of 4.65 (SD ± 2.07) at T0 to 3.74 (SD ± 1.96) at T5, respectively (Table 2).
|
Symptom |
Total (n 34) |
Group A (n 17) |
Group B (n 17) |
|
|||
|
Assessment |
mean |
SD |
mean |
SD |
mean |
SD |
p-value* |
|
Diarrhoea |
|
|
|
|
|
|
|
|
T0 |
4.65 |
±2.07 |
4.59 |
±2.18 |
4.71 |
±2.02 |
0.8715 |
|
T1 |
4.29 |
±1.85 |
4.65 |
±1.87 |
3.94 |
±1.82 |
0.2727 |
|
T2 |
4.15 |
±2.18 |
4.59 |
±2.35 |
3.71 |
±1.96 |
0.2430 |
|
T3 |
4.24 |
±2.23 |
4.65 |
±2.15 |
3.82 |
±2.30 |
0.2885 |
|
T4 |
3.82 |
±2.15 |
4.59 |
±2.12 |
3.06 |
±1.95 |
0.0362a |
|
T5 |
3.74 |
±1.96 |
4.71 |
±1.83 |
2.76 |
±1.60 |
0.0024b |
|
Constipation |
|
|
|
|
|
|
|
|
T0 |
3.88 |
±1.74 |
3.71 |
±1.83 |
4.06 |
±1.68 |
0.5616 |
|
T1 |
3.79 |
±1.39 |
3.76 |
±1.44 |
3.82 |
±1.38 |
0.9039 |
|
T2 |
3.56 |
±1.76 |
3.76 |
±1.86 |
3.35 |
±1.69 |
0.5039 |
|
T3 |
3.38 |
±1.63 |
3.76 |
±1.71 |
3.00 |
±1.50 |
0.1760 |
|
T4 |
3.21 |
±1.79 |
3.71 |
±1.83 |
2.71 |
±1.65 |
0.1039 |
|
T5 |
2.97 |
±1.85 |
3.71 |
±1.83 |
2.24 |
±1.60 |
0.0180 a |
|
Meteorism |
|
|
|
|
|
|
|
|
T0 |
8.47 |
±1.11 |
8.41 |
±1.12 |
8.53 |
±1.12 |
0.7620 |
|
T1 |
6.82 |
±1.27 |
6.59 |
±1.28 |
7.06 |
±1.25 |
0.2855 |
|
T2 |
4.82 |
±1.51 |
4.65 |
±1.46 |
5.00 |
±1.58 |
0.5031 |
|
T3 |
3.47 |
±1.24 |
3.06 |
±0.83 |
3.88 |
±1.45 |
0.0506 a |
|
T4 |
2.53 |
±1.05 |
2.00 |
±0.50 |
3.06 |
±1.20 |
0.0020b |
|
T5 |
2.79 |
±1.39 |
2.06 |
±0.90 |
3.53 |
±1.42 |
0.0010b |
|
Abdominal Pain |
|
|
|
|
|
|
|
|
T0 |
6.91 |
±1.36 |
6.71 |
±1.31 |
7.12 |
±1.41 |
0.3844 |
|
T1 |
5.41 |
±1.28 |
5.35 |
±1.27 |
5.47 |
±1.33 |
0.7937 |
|
T2 |
4.85 |
±1.28 |
4.82 |
±1.29 |
4.88 |
±1.32 |
0.8960 |
|
T3 |
3.71 |
±1.12 |
3.65 |
±1.06 |
3.76 |
±1.2 |
0.7637 |
|
T4 |
2.91 |
±1.08 |
2.94 |
±1.14 |
2.88 |
±1.05 |
0.8771 |
|
T5 |
2.74 |
±0.90 |
3.18 |
±0.88 |
2.29 |
±0.69 |
0.0027b |
|
Food Tolerance |
|
|
|
|
|
|
|
|
T0 |
4.74 |
±2.09 |
4.76 |
±2.11 |
4.71 |
±2.14 |
0.9362 |
|
T1 |
4.65 |
±2.03 |
4.59 |
±2.03 |
4.71 |
±2.08 |
0.8687 |
|
T2 |
4.26 |
±2.50 |
4.18 |
±2.48 |
4.35 |
±2.60 |
0.8407 |
|
T3 |
4.59 |
±2.24 |
4.41 |
±2.27 |
4.76 |
±2.28 |
0.6537 |
|
T4 |
4.44 |
±1.91 |
4.47 |
±1.94 |
4.41 |
±1.94 |
0.9301 |
|
T5 |
4.74 |
±2.26 |
4.76 |
±2.31 |
4.71 |
±2.28 |
0.9409 |
Table 2: Mean and Standard Deviation (SD) of scores for symptoms diarrhoea, constipation, meteorism, abdominal pain and food tolerance listed as total and for groups A and B at each assessment session, respectively. P-value calculated between Group A and Group B at each single assessment session for each symptom. Std Dev: standard deviation.
Group A showed a slight increase of the average rating of this symptom, while Group B showed a decrease in rating that passed from an average scoring of 4.71 to 2.76 between T0 and T5 (except for a small increase as seen in T3), respectively (Graphic 1a, 1b). 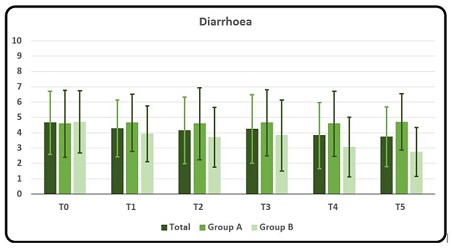
Graphic 1a: Mean and DS rating of symptom Diarrhoea as a whole, for Group A and for Group B at T0, T1, T2, T3, T4 and T5, respectively. Rating scores from number from 0 to 10 where 0 meant no symptom and 10 the maximum discomfort/disturbance endured by the subject.
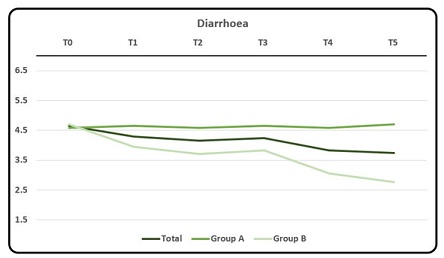 Graphic 1b: Mean rating of symptom Diarrhoea.
Graphic 1b: Mean rating of symptom Diarrhoea.
Anova showed a statistically significant difference between the ratings of the two groups at T4 and T5, with p-Value values lower than 0.05 and 0.01, respectively. At T4 the overall average rating done by Group B (i.e., 3.06) was lower than that done by Group A (i.e., 4.59). T-test gave a statistically significant difference (p <0.1) between overall ratings at T0 and at T5 with ratings that decreased in time.
The evaluation of rating scores at T4 and at T5 between group A and group B resulted in a statistically significant lower difference (with values of p = 0.0362 at T4 and p = 0.0024 at T5, respectively) in group B as compared to group A (Table 3).
|
Symptom |
T0 à T5 |
T0à T3 |
T3à T5 |
|
Diarrhoea |
0.0667 |
0.4332 |
0.3296 |
|
Constipation |
0.0400 a |
0.2257 |
0.3342 |
|
Meteorism |
0.0000 b |
0.0000 b |
0.0376 a |
|
Abdominal Pain |
0.0000 b |
0.0000 b |
0.0002 b |
|
Food Tolerance |
1.0000 |
0.7808 |
0.7886 |
a p < 0.05; b p < 0.01
Table 3: T-test results for statistical significance of scores recorded between T0 and T5, T0 and T3 and T3 and T5, respectively.
Constipation
Rating of symptom Constipation resulted in an overall gradual decrease of scores throughout the evaluations submitted where the average value passed from 3.88 (D.S. ± 1.74) at T0 to 2.97 (D.S. ± 1.85) at T5, respectively. Table 2 As regards the two groups A and B, there was a different trend between Group A and Group B. While rating of symptom Constipation in Group B showed a decline that passed from an average of 4.05 to 2.24 between T0 and T5, Group A rating showed no significant difference between T0 and T5 (Graphic 2a, 2b).
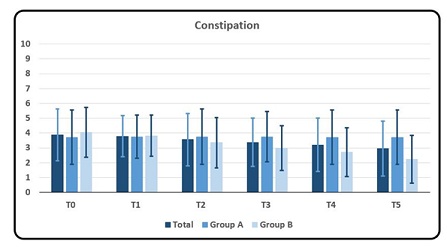 Graphic 2a: Mean and DS rating of symptom Constipation as a whole, for Group A and for Group B at T0, T1, T2, T3, T4 and T5, respectively. Rating scores from number from 0 to 10 where 0 meant no symptom and 10 the maximum discomfort/disturbance endured by the subject.
Graphic 2a: Mean and DS rating of symptom Constipation as a whole, for Group A and for Group B at T0, T1, T2, T3, T4 and T5, respectively. Rating scores from number from 0 to 10 where 0 meant no symptom and 10 the maximum discomfort/disturbance endured by the subject.
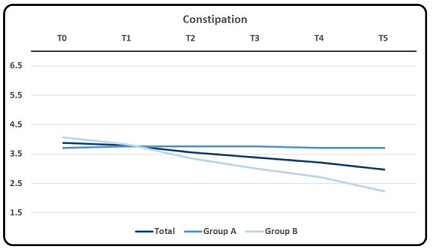 Graphic 2b: Mean rating of symptom Constipation.
Graphic 2b: Mean rating of symptom Constipation.
ANOVA showed a statistically significant difference between group A and B at T5 (p = 0.0180). Analyzing the averages of the two groups, a lower value emerges for Group B. T-test showed a statistically significant difference (p < 0.05) between the T0 and T5 rating scores. The evaluation of rating scores at T5 between group A and group B resulted in a statistically significant lower difference (with values of p = 0.0180) in group B as compared to group A table 3.
Meteorism
Rating of symptom Meteorism resulted in an overall considerable decrease in scores as the mean score fell from 8.47 (D.S. ± 1.11) at T0 to 4.82 (D.S. ± 1.51) at T2 to reach 2.53 (± 1.05) at T4 (though with a slight increase as seen at T5) table 2. The same trend is seen in each group. Average rating scores in group A (though similar at T0 to group B) were lower than in group B throughout all evaluations (Graphic 3a, 3b).
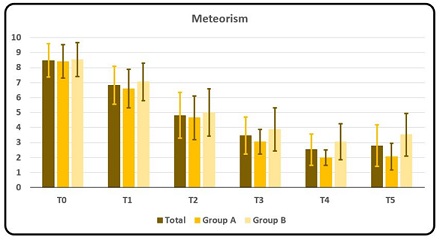 Graphic 3a: Mean and DS rating of symptom Meteorism as a whole, for Group A and for Group B at T0, T1, T2, T3, T4 and T5, respectively. Rating scores from number from 0 to 10 where 0 meant no symptom and 10 the maximum discomfort/disturbance endured by the subject.
Graphic 3a: Mean and DS rating of symptom Meteorism as a whole, for Group A and for Group B at T0, T1, T2, T3, T4 and T5, respectively. Rating scores from number from 0 to 10 where 0 meant no symptom and 10 the maximum discomfort/disturbance endured by the subject.
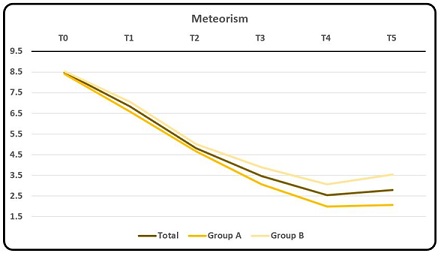 Graphic 3b: Mean rating of symptom Meteorism.
Graphic 3b: Mean rating of symptom Meteorism.
ANOVA showed a statistically significant difference between average scores in group A and B at T4 and T5 evaluations, respectively. T-test showed a statistically significant decrease in scores (p < 0.005) between T0 and T3 and between T0 and T5, respectively. Furthermore, T test showed a statistically significant decrease in scores (p < 0.05) between T3 and T5 Table 3.
Abdominal pain
Rating of symptom Abdominal pain resulted in an overall considerable decrease in scores as mean score fell from 6.91 (±1.36) at T0 to 2.74 (±0.90) at T5 [Table 1]. The same trend can also be found in the two groups, in which it is necessary to detect a slight increase in values at T5 in Group A (Graphic 4a, 4b).
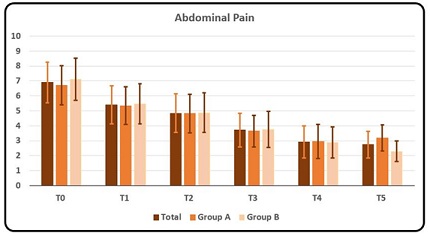 Graphic 4a: Mean and DS rating of symptom Abdominal Pain as a whole, for Group A and for Group B at T0, T1, T2, T3, T4 and T5, respectively. Rating scores from number from 0 to 10 where 0 meant no symptom and 10 the maximum discomfort/disturbance endured by the subject.
Graphic 4a: Mean and DS rating of symptom Abdominal Pain as a whole, for Group A and for Group B at T0, T1, T2, T3, T4 and T5, respectively. Rating scores from number from 0 to 10 where 0 meant no symptom and 10 the maximum discomfort/disturbance endured by the subject.
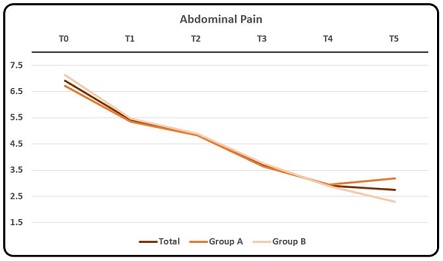 Graphic 4b: Mean rating of symptom Abdominal Pain.
Graphic 4b: Mean rating of symptom Abdominal Pain.
ANOVA showed a statistically significant difference between average scores in group A and B only at T5, where average scoring of group B resulted lower than group A. T-test showed a statistically significant difference (p < 0.005) between T0 and T3, between T0 and T5 and between T3 and T5, respectively [Table 2]
Food Intolerance
Rating of symptom Food Intolerance resulted in a fluctuating trend without any significant changes in rating scores throughout all evaluations both as overall evaluation as well as the single groups. Tab.1. T0 and T5 showed similar average scores. Only T2 showed a slight decrease in overall average scores and of the single groups. Group B at T3 showed a slight increase in average score (4.76 con D.S. ± 2.28) (Graphic 5a, 5b).
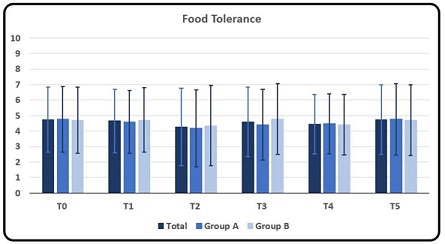 Graphic 5a: Mean and DS rating of symptom Food Tolerance as a whole, for Group A and for Group B at T0, T1, T2, T3, T4 and T5, respectively. Rating scores from number from 0 to 10 where 0 meant no symptom and 10 the maximum discomfort/disturbance endured by the subject.
Graphic 5a: Mean and DS rating of symptom Food Tolerance as a whole, for Group A and for Group B at T0, T1, T2, T3, T4 and T5, respectively. Rating scores from number from 0 to 10 where 0 meant no symptom and 10 the maximum discomfort/disturbance endured by the subject.
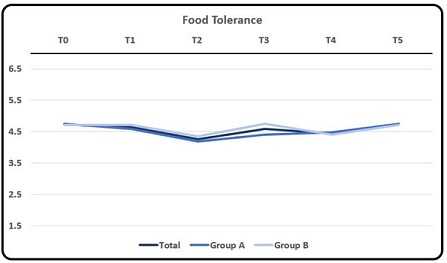 Graphic 5b: Mean rating of symptom Food Tolerance.
Graphic 5b: Mean rating of symptom Food Tolerance.
ANOVA did not show any statistically significant difference between average scores in group A and B. T-test did not show any statistically significant differences between scores at analyzed evaluations table 2.
Discussion
In this study 34 subjects were enrolled and completed all evaluations. Subjects were allocated to one of two groups with the only difference being the treatment protocol. The study did not include a placebo group since baseline was considered by data collected at T0, which, after statistical analysis, confirmed similar characteristics throughout the 2 study groups.
Subjects enrolled had superficial knowledge of AA and would not have been able to tell the difference between the two AA protocols carried out. Furthermore, the 2 treatment protocols varied for only few AA points that are difficult to discern for non-AA practitioners. Thus, it is reasonable to assume that there is a blinding of the subjects to the treatment protocol.
IBS Patients frequently observe that their symptoms impede normal daily activity. The symptoms of IBS are very varied and for this reason five most frequently cited variables in literature were considered for evaluation of results from the 2 protocols proposed: diarrhoea, constipation, meteorism, abdominal pain and food Intolerance.
Results showed that IBS patients treated with AA obtained positive results with improvement on single specific IBS symptoms. Though not all IBS symptoms analyzed gave positive results, it is reasonable to believe that such a therapy could be implemented to obtain modification of single specific IBS symptoms.
The symptom diarrhoea overall did not achieve great positive results if data was analyzed as aggregate. In the single groups results showed no significant change as regards group A but did show a gradual positive result that could be considered effective in group B. Thus, the protocol used in group B could be proposed to IBS-D patients.
Also, the symptom constipation showed a similar situation as seen from results obtained, where an overall gradual decrease of this symptom was observed. Data showed that treatment protocol for group B was significantly effective as regards bowel movement frequency thus to be considered a viable AA treatment option in IBS-C patients. On the other hand, no significant change was observed as regards group A.
As regards meteorism, remarkable immediate results were obtained both overall and in the single treatment protocol groups, with slightly better results obtained with treatment protocol for group A as compared to group B. Furthermore, it is to be noted that these positive results were confirmed at follow-up evaluations.
Results from scoring of abdominal pain also were very good with overall and each group obtaining an immediate significant reduction in their scorings that was confirmed at follow-up evaluations. Here too, abdominal pain obtained better results from the treatment protocol used in group B then group A.
Food intolerance did not show any change in scoring between evaluations as overall nor in each single group.
Thus, group A protocol treatment obtained the best results as regards the symptom meteorism with good results also for abdominal pain. On the other hand, group B obtained the best results as regards the symptoms diarrhoea, constipation and abdominal pain with good results also for meteorism. It is reasonable to believe that the protocol used in group B could be used as a first approach in AA treatment in any-type IBS patient.
Interestingly, none of the treatment protocols obtained results as regards food intolerance. It can be speculated that probably a longer follow-up would give a change in rating due to time necessary to change eating habits and evaluation of effects of previously “forbidden” foods.
Remarkably, it was interesting to observe that of the 2 AA treatment protocols, group B in general obtained better overall results than group A, contrary to what was expected. Though both protocols achieved positive results it can better be defined which type of treatment protocol would be suitable for IBS patients through a direct comparison to prove efficacy as based on results obtained through trials and less on theoretical AA reasoning.
Limitations of the study can be identified as follows. A limited number of patients have been evaluated if compared to the number of IBS patients in the population. A greater number of subjects to enrol would give a higher value to results obtained. The time period of evaluation can be considered limited since the evaluation of long-term results and the evaluation of change in patient quality of life would better demonstrate the effect of AA on IBS symptoms if done at longer follow-up. Limited randomization of patients can give rise to bias even though it must be considered that the only difference between the two groups was the AA treatment protocol used. The aspects evaluated were limited to the 5 most frequent IBS symptoms as seen in literature which are easily investigated. Further investigation into other aspects would better evaluate impact of AA treatment on quality of life of IBS patients. Lastly, the use of exclusion criteria to wean out subjects highly influenced by the placebo effect could better validate results obtained.
Conclusion
From obtained results it is reasonable to believe that AA is a viable, limited-resource, well tolerated, acceptable treatment for IBS to help reduce discomfort, symptoms and factors associated with severity. AA treatment protocol choice must be based on results obtained from clinical trials that compare different protocols choices. Though this paper is to be considered a pilot study due to the limited number of subjects enrolled, it is reasonable to believe that further research with a larger sample of subjects will better validate results obtained with AA on IBS patients. Furthermore, there is a need for further research to evaluate which AA IBS protocol to use on IBS patients will obtain the best results. Conclusions from the latter will enable AA practitioners to offer the most efficient AA treatment to their IBS patients.
Acknowledgment
A special thanks to all AIRAS for their precious human and scientific technical support.
References
- Douglas A (2016) Drossman; Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features, and Rome IV. Gastroenterology 150: 1262-1279.
- Cremonini F, Talley NJ (2005) Irritable bowel syndrome: epidemiology, natural history,
health care seeking and emerging risk factors. Gastr Clin North Am 34: 189-204. - Fortea J, Prior M (2013) Irritable Bowel Syndrome With Constipation: A European-focused Systematic Literature Review of Disease Burden. J Med Econ 16: 329-341.
- Mearin F, Lacy BE, Chang L, Chey WD, Lembo AJ, et al. (2016) Bowel disorders. Gastroenterology 150: 1393-1407.
- Drossman DA, Chang L, Bellamy N, Torres HEG, Lembo A, et al. (2011) Severity in irritable bowel syndrome: a RomeFoundation Working Team report. Am J Gastroenterol 106: 1749-1759.
- Sayuk GS, Wolf R, Chang L (2017) Comparison of symptoms, healthcare utilization, and treatment in diagnosed and undiagnosed individuals with diarrhea-predominant irritable bowel syndrome. Am J Gastroenterol 112: 892-899.
- Begtrup LM, Engsbro AL, Kjeldsen J, Larsen PV, Muckadell OS, et al. (2013) A positive diagnostic strategy is noninferior to a strategy of exclusion for patients with irritable bowel syndrome. Clin Gastroenterol Hepatol 11: 956-962.
- Cangemi DJ, Lacy BE (2019) Management of irritable bowel syndrome with diarrhea: a review of nonpharmacological and pharmacological interventions. Ther Adv Gastr 12: 1-19.
- Ford AC, Lacy BE, Talley NJ (2017) Irritable bowel syndrome. N Engl J Med 376: 2566-2578.
- Muchtar NJ, Helianthi DR, Nareswari I (2020) Effectiveness of Acupuncture for Management in a Hospitalized Geriatric Patient With Constipation. Med Acupunct 32: 116-120.
- Zhou W, Deng Q, Jia L, Zhao H, Yang M, et al. (2020) Acute Effect of Transcutaneous Electroacupuncture on Globus Pharyngeus: A Randomized, Single-Blind, Crossover Trial. Front Med 7: 179.
- Guo Y, Wei W, Chen JDZ (2020) Effects and mechanisms of acupuncture and Electroacu- puncture for functional dyspepsia: A systematic review. World J Gastroenterol 26: 2440-2457.
- Zheng H, Chen R, Zhao X, Li G, Liang Y, et al. (2019) Comparison between the Effects of Acupuncture Relative to Other Controls on Irritable Bowel Syndrome: A Meta-Analysis. Pain Res Manag 2019: 2871505.
- Shi X, Hu Y, Zhang B, Li W, Chen JD, et al. (2021) Ameliorating effects and mechanisms of transcutaneous auricular vagal nerve stimulation on abdominal pain and constipation. JCI Insight 6: 150052.
- Zhang Y, Lu T, Meng Y, Maisiyiti A, Dong Y, et al. (2021) Auricular vagal nerve stimulation improves constipation by enhancing colon motility via the central-vagal efferent pathway in opioid-induced constipated rats. Nuromodulation 24: 1258-1268.
- Farmer AD, Albusoda A, Amarasinghe G, Ruffle JK, Fitzke HE, et al. (2020) Transcutaneous vagus nerve stimulation prevents the development of, and reverses, established oesophageal pain hypersensitivity. Aliment Pharmacol The 52: 988-996.
- Oleson T (2019) Standardized Ear Acupuncture Nomenclature Utilizing Auricular Landmarks and 3-D Graphic Imaging for Delineating Different Auricular Zones. Med Acupunct 31: 145-156.
- Lovato A, Ceccherelli F, Gagliardi G, Postiglione M (2022) The Medial Surface of the Auricle: Historical and Recent Maps. What Are the Possible Expectations of the "Thumb-Index Technique". Medicines (Basel) 9: 13.
- Romoli M, Greco F, Giommi A (2016) Auricular acupuncture diagnosis in patients with lumbar hernia. Complement Ther Med 26:61-65.
- Renè JH K (1983) Lauriculomédecine en consultation journalière. Maloine SA, Paris, France.
- Lovato A (2019) Agopuntura Auricolare: Teoria a Clinica. NOI Edizioni. Milano, Italy.
- Ridolfi AW (2019) The History of Ear Acupuncture and Ear Cartography: Why Precise Mapping of Auricular Points Is Important. Med Acupunct 31: 145-156.
- Terry O (2014) Auriculotherapy Manual. Elsevier edizioni, Toronto, Canada.
Citation: Lovato A, Gagliardi G, Merlini N, Soiat M, Postiglione M, et al. (2022) Treatment of Irritable Bowel Syndrome with Auricular Acupuncture: A controlled pilot study. J Altern Complement Integr Med 8: 267.
Copyright: © 2022 , ,, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

