Type A Acute Aortic Dissection Complicated With Cerebral Malperfusion
*Corresponding Author(s):
Ying-Fu ChenDepartment Of Surgery, Division Of Cardiovascular Surgery, Kaohsiung Medical University, Kaohsiung, Taiwan, Province Of China
Tel:+886 73121101,
Fax:+886 73127056
Email:yfchen@cc.kmu.edu.tw
Keywords
INTRODUCTION
Type A Acute Aortic Dissection (TAAAD) has been associated with a poor prognosis without prompt optimal management. Even though the overall mortality declined over these years, the in-hospital mortality was still high up to 19.7% for those patients receiving emergent surgery and 57.1% in those medically treated based on a 17-year analysis of International Registry of Acute Aortic Dissection (IRAD) [1]. The most typical symptom of patients with TAAAD is abrupt onset of chest and/or back pain, often depicted as the worst one they have ever experienced. Besides, dissecting plane may sometimes obstruct the blood flow distribution to peripheral organ or even lead to generalized ischemia, causing malperfusion and leading to adverse outcomes [2]. The associated clinical manifestations depend on the ischemic location and can be divided into localized ischemia (cerebral, spinal, mesenteric, renal, limb, and coronary malperfusion) and generalized ischemia. The reported overall incidence of malperfusion is 21-33% and the in-hospital mortality is 16-44% [3-5].
Considering Cerebral Malperfusion (CM), it accounts for an incidence of 8-26% [3,4,6]. The definition varies among centers. Pacini et al., [3] defined CM as stroke or transient ischemic attack, while Morimoto et al., [6] defined it with symptoms of newly developed neurologic deficits along with evidence from contrast CT or carotid ultrasonography of decreased blood flow in carotid arteries. Image modality is valid to assist in diagnosis since most cases develope dissection of supra-aortic branches [7] (Figure 1).
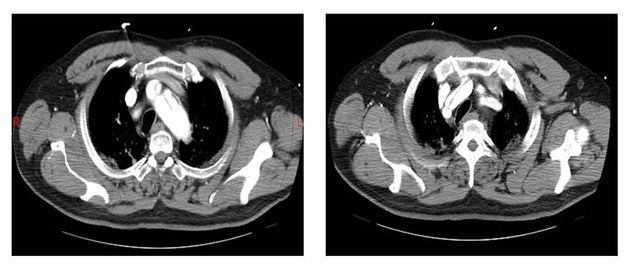
Figure 1: Type-A-Acute-Aortic-Dissection-Complicated-With-Cerebral-Malperfusion.
The optimal treatment for patients with CM remains controversial, owing to high mortality around 21~50% [8-10]. Debate persists about whether to adopt delaying the repair surgery with initially medical management or to undergo immediately operation. Physicians who advocate to treat with initially medical management and delay the surgery because of concerning the risk of conversion to hemorrhagic infarction after blood flow restoration to ischemic regions and anticoagulation use during cardiopulmonary bypass [11]. In this situation, carotid stenting is a good alternative [8]. As well, some investigators had demonstrated a better outcome of those with initially medical treatment [12]. Nevertheless, Nakamura et al., [13] commented three disadvantages noted in delaying surgery: 1. medical treatment was related to poor prognosis according to their experiences; 2. tight blood pressure control might reduce cerebral perfusion pressure, impairing the blood flow to the ischemic region; 3. it would require the patients to get in bed rest for a period of time and delay the rehabilitation, leading to poor recovery from neurologic dysfunction. They performed immediate aortic repair followed by early rehabilitation in 10 patients with TAAAD complicated by CM and no one died in hospital, besides, the overall neurological function improved both postoperatively and mid-term follow-up [13].
Although more and more investigations agree that CM is not a contraindication of emergent operation [6,11,13,14], the timing cut off from symptoms onset to surgery is still unclear. Morimoto et al., [6] reviewed 41 surgical patients complicated with CM and evaluated their pre- and post-operative neurologic function, using the National Institutes of Health Stroke Scale (NIHSS) score. They came to a conclusion that the optimal cutoff points for predicting lack of neurologic improvement were NIHSS score more than 11 and the time to surgery longer than 9.1 hours [6]. On the other hand, Estrera et al., [11] surveyed on patients who suffered from preoperative stroke. They found that the proportion of neurologic improvement was 80% in patients with surgery within 10 hours, but 0% in those patients with surgery beyond 10 hours (p = 0.02) [11]. It seems that operation for patients with CM as soon as possible is a good choice. In addition, patients with lower severity of neurologic dysfunction is associated with better prognosis. Nonetheless, the water-shed of better timing to surgery and the adequate management for patients in different severity of CM are still less surveyed.
As mentioned above, the in-hospital mortality of TAAAD complicated with CM remains high in current era. Therefore, it is reported as a significant risk factor of TAAAD [2,3,8]. In terms of long-term follow-up, the long-term survival rate was less promising with 1-, 5-, and 10-year survival rates of patients with surgical repair being 50.0 ± 12.5%, 37.5 ± 12.1%, and 12.5 ± 11.0%, respectively, for patients with CM. On the contrary, TAAAD patients without CM had 1-, 5-, and 10-year survival rates of 81.5 ± 2.7%, 64.7 ± 3.6%, and 49.1 ± 5.4%, were significantly higher than that of the CM group (p = 0.0002) [15].
CONCLUSION
Even though the medical progress is more and more advanced, TAAAD is still a lethal disease, especially in those with complication of Cerebral Malperfusion (CM) and the management for these patients has been a dilemma for a long time. Recently, a number of investigators supported that immediate surgery could have a better results in patients complicated with CM, although it remains controversial about the cutoff point of time for surgery. Nonetheless, a conclusion from the latest articles review could be suggested that operation should be performed as soon as possible base on aforementioned evidences from a number of investigators.
REFERENCES
- Pape LA, Awais M, Woznicki EM, Suzuki T, Trimarchi S, et al. (2015) Presentation, Diagnosis, and Outcomes of Acute Aortic Dissection: 17-Year Trends From the International Registry of Acute Aortic Dissection. J Am Coll Cardiol 66: 350-358.
- Li HW, Shih YC, Liu HH, Chen CW, Chien TM, et al. (2016) Reconsidering the Impact of Pre-Operative Malperfusion on Acute Type A Dissection: The Modified Penn Classification. J Am Coll Cardiol 67: 121-122.
- Pacini D, Leone A, Belotti LM, Fortuna D, Gabbieri D, et al. (2013) Acute type A aortic dissection: significance of multiorgan malperfusion. Eur J Cardiothorac Surg 43: 820-826.
- Immer FF, Grobéty V, Lauten A, Carrel TP (2006) Does malperfusion syndrome affect early and mid-term outcome in patients suffering from acute type A aortic dissection? Interact Cardiovasc Thorac Surg 5: 187-190.
- Cho YH, Sung K, Kim WS, Jeong DS, Lee YT, et al. (2014) Malperfusion syndrome without organ failure is not a risk factor for surgical procedures for type A aortic dissection. Ann Thorac Surg 98: 59-64.
- Morimoto N, Okada K, Okita Y (2011) Lack of neurologic improvement after aortic repair for acute type A aortic dissection complicated by cerebral malperfusion: predictors and association with survival. J Thorac Cardiovasc Surg 142: 1540-1544.
- Urbanski PP, Wagner M (2012) Perfusion and repair technique in acute aortic dissection with cerebral malperfusion and damage of the innominate artery. J Thorac Cardiovasc Surg 144: 982-984.
- Tanaka H, Okada K, Yamashita T, Morimoto Y, Kawanishi Y, et al. (2005) Surgical results of acute aortic dissection complicated with cerebral malperfusion. Ann Thorac Surg 80: 72-76.
- Augoustides JG, Geirsson A, Szeto WY, Walsh EK, Cornelius B, et al. (2009) Observational study of mortality risk stratification by ischemic presentation in patients with acute type A aortic dissection: the Penn classification. Nat Clin Pract Cardiovasc Med 6: 140-146.
- Girdauskas E, Kuntze T, Borger MA, Falk V, Mohr FW (2009) Surgical risk of preoperative malperfusion in acute type A aortic dissection. J Thorac Cardiovasc Surg 138: 1363-1369.
- Estrera AL, Garami Z, Miller CC, Porat EE, Achouh PE, et al. (2006) Acute type A aortic dissection complicated by stroke: can immediate repair be performed safely? J Thorac Cardiovasc Surg 132: 1404-1408.
- Fukuda I, Imazuru T (2003) Intentional delay of surgery for acute type A dissection with stroke. J Thorac Cardiovasc Surg 126: 290-291.
- Nakamura Y, Tagusari O, Ichikawa Y, Morita A (2011) Impact of immediate aortic repair on early and midterm neurologic status in patients with acute type a aortic dissection complicated by cerebral malperfusion. Ann Thorac Surg 92: 336-338.
- Di Eusanio M, Patel HJ, Nienaber CA, Montgomery DM, Korach A, et al. (2013) Patients with type A acute aortic dissection presenting with major brain injury: should we operate on them? J Thorac Cardiovasc Surg145: 213-221.
- Geirsson A, Szeto WY, Pochettino A, McGarvey ML, Keane MG, et al. (2007) Significance of malperfusion syndromes prior to contemporary surgical repair for acute type A dissection: outcomes and need for additional revascularizations. Eur J Cardiothorac Surg 32: 255-262.
Citation: Hsiu-Wen Li, Ting-Hsuan Lin, Yu-Cheng Shih, Hao-Hsun Liu, Chao-Yang Wang et al. (2016) Type A Acute Aortic Dissection Complicated With Cerebral Malperfusion. J Cardiol Stud Res 3: 012.
Copyright: © 2016 Hsiu-Wen Li, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.