
Undiagnosed Hard-to-Heal Wound Cases: A Case Series
*Corresponding Author(s):
Tuna GumusDepartment Of Undersea And Hyperbaric Medicine, University Of Health Sciences, Kartal Dr. Lutfi Kirdar City Hospital, Istanbul, Turkey
Tel:+90 5427876732,
Fax:+90 2164413900
Email:tunagumus@yahoo.com
Abstract
Introduction: The aim of this study is to raise awareness in our colleagues who read the article by addressing hard-to-heal wound cases that have been misdiagnosed or undiagnosed in the outpatient wound care clinics. The common feature of these cases is the diseases that can be found in the etiology of all and can be fatal. Many of the cases in this article were evaluated in various hospitals and different branch outpatient wound care clinics before admission and were followed up with standard wound care with different diagnoses, but there was no improvement in their wounds.
Methods: The wounds evaluated in this study are calciphylaxis, Antiphospholipid Syndrome (APS), Amelanotic Melanoma (AM), Basosquamous Cell Carcinoma (BSC) and Factor V Leiden (FVL) mutation. The oldest of the 5 cases is 68 years old and the youngest is 8 years old. 4 cases were referred to our outpatient clinic by the centers where they were followed up, to receive wound care and, if indicated, Hyperbaric Oxygen (HBO) therapy. 1 case applied without any referral as a result of her own research.
Results: Among the adult cases, patients with calciphylaxis and basosquamous carcinoma passed away respectively on the ninth day and the eleventh month after admission due to the underlying diseases that caused their injuries. 1 child received the appropriate treatment after the correct diagnosis and approach. In 3 cases, surgical intervention was required during the follow-up process (debridement, amputation, wide resection).
Conclusion: In the evaluation of chronic wounds, it is necessary to look at them from a wide perspective. If a wound does not heal, another underlying disease should be investigated. In treatment-resistant atypical cases, the clinician should take a biopsy in the slightest doubt and the diseases that cause thrombophilia in etiology should be evaluated. Early and accurate diagnosis is essential in cases of chronic wounds. These diseases can cause loss of limb or even death. A doctor evaluating chronic wounds should be informed about the diseases mentioned in this study.
Keywords
Chronic wound; Thrombophilia; Wound biopsy
Introduction
The aim of this study is to raise awareness in our colleagues who read the article by addressing hard-to-heal wound cases that have been misdiagnosed or undiagnosed in the wound care related outpatient and inpatient clinics. The common feature of these cases is the diseases that can be found in the etiology of all and can be fatal. Many of the cases in this article were evaluated in various hospitals and different branch outpatient clinics before admission and were followed up with standard wound care with different diagnoses, but there was no improvement in their wounds.
Methods
The wounds evaluated in this study are calciphylaxis, antiphospholipid syndrome, amelanotic melanoma, basosquamous cell carcinoma and Factor V Leiden mutation. The oldest of the 5 cases is 68 years old and the youngest is 8 years old. 4 cases were referred to our outpatient clinic by the centers where they were followed up, to receive wound care and, if indicated, Hyperbaric Oxygen (HBO) therapy. 1 case applied without any referral as a result of her own research.
Patient 1
The 68 years old female patient has a 23-year history of Type 2 diabetes mellitus and a 5-year history of dialysis. Dressing follow-up was made for 3 months with the diagnosis of diabetic foot. Her biggest complaint at the time of admission was severe pain and foul smelling discharge. The patient stated that she changed dressings twice a day and dressed the wound with an antibiotic cream. The patient had follow-up examination for her wounds at a university hospital once every 10 days. The wounds on both feet started to appear on her legs within 1 week. Before the wounds were opened, there was a discoloration, blistering, and then the wounds occurred after the lesions exploded. After the wounds occurred, they formed black scabs (Figure 1). She is receiving on hemodialysis three days a week. During the follow-up process, her pain and discharge from her wounds increased continuously. She did not respond to empirical antibiotics. Silver and alginate wound dressings were also used, but they did not provide any benefit. At the time of admission, her results were as follows; HbA1c: 9.8, WBC: 12300, Sedimentation: 68 and CRP: 132. When the patient's dressing was opened, it was determined that all dressing material was green. There was a foul smell before the dressing was opened, and the bad smell increased when the dressing was opened. All the wounds were hypersensitive to palpation. Wound culture and skin biopsy were taken from the wounds. Foot and leg radiographs were requested. Calcium, phosphorus, urea, calcium and coagulation and blood tests were requested. Pseudomonas aeruginosa growth occurred in the patient's culture. As a result of the biopsy, which was determined 14 days later, the diagnosis of calciphylaxis was made. Arterial calcifications were observed on plain radiographs. Since the biopsy result did not come out, the planned intravenous sodium thiosulfate treatment could not be started before the patient died. The patient passed away as a result of the development of sepsis 9 days after the application, before the biopsy result. 
Figure 1: Calciphylaxis.
Patient 2
An 8-year-old girl applied to the outpatient clinic for HBO therapy due to thigh and leg wounds accompanied by her father. The patient was crying with pain at the time of admission. There were 2 ulcers on the upper lateral of the thigh and on the posterior side of her right leg, in sizes of 5x9 cm and 4x11 cm respectively, the base of which was covered with necrotic tissue and they were extremely sensitive to palpation (Figure 2). The patient’s relative stated that they have come from a town outside the city, that the wounds had been present for 9 months, and that they were followed up with a dressing. From time to time, the wounds were debrided, but then they got bigger and started to turn black inside. Antibiotherapy planned according to the taken wound cultures did not provide any benefit. He stated that they used antibiotic cream and some wound products that they did not know the name of. They applied to a university hospital due to the widening of the wounds and the blackening of the base. From there, they were directed to be evaluated for HBO therapy and debridement. At the first examination of the patient's wounds, a thrombophilic disease was suspected. In the patient’s history, there was no finding explaining the current situation in the first degree relatives. The patient was referred to the genetic department for peripheral blood thrombophilia panel and to hematology for investigation of possible related diagnoses and to the plastic surgery departments for debridement under anesthesia. As a result of the examinations and tests, the patient was diagnosed with anti-phospholipid syndrome. The patient was hospitalized and appropriate medical and surgical wound care was planned simultaneously with appropriate antithrombotic treatment. 
Figure 2: Antiphospholipid syndrome.
Patient 3
A 44years old female patient who had been diagnosed with diabetes mellitus for 8 years was admitted to the outpatient clinic with a wound on the small toe of her left foot that did not heal for 11 months and grew larger. During the inspection at the admission, a hypergranular wound extending to the metatarsophalangeal joint was detected in the proximal phalanx lateral of the fifth finger of the left foot (Figure 3). In the history of the patient, it was determined that she was followed up with diabetic foot ulcer diagnosis in various hospitals only with different dressing recommendations and antibiotherapy. No osteomyelitis was detected in the direct radiography and MRI examinations of the patient which were taken before admission. The infection laboratory findings of the patient, were within normal limits other than HbA1c (7.8%)at the time of admission. She had 2+ edema in her foot. There was no hyperemia, no erythema. Dorsalispedis and tibialis posterior arteries were palpable. The patient was referred to be evaluated in terms of HBO therapy. First, an incisional biopsy was taken from the patient's lesion because malignancy was suspected during the inspection. The patient was diagnosed with amelanotic melanoma according to the biopsy result which arrived 14 days later. The patient was referred to plastic surgery and medical oncology departments. 
Figure 3: Amelanotic melanoma.
Patient 4
A 38 years old male patient was admitted with a wound complaint that had been on his back and did not heal for 8 months and was expanding gradually. He stated that his wound initially looked like a big pimple, took the form of a wound within 2 months and he made the first application to the hospital at that time. Since the occurrence of the wound, the patient has used antibiotic cream, antibiotherapy planned according to the empirical or wound culture results, and various wound dressings. In the process, the wound deepened and expanded even more. When the wound did not heal, he was referred to be evaluated for HBO therapy. It was determined that the patient did not have any additional disease in his history. And his family history was normal as well. At the time of admission, a wound with a partially irregular edges and with granulation tissue in the form of yellowish islets on the base, approximately 4x7x05 cm in size was detected in the right scapular region (Figure 4). Incisional biopsy was taken from 3 different areas of the wound, as the wound caused suspicion of malignancy during the inspection. Wound culture was also taken to be evaluated for infection due to the smell of the wound dressing and exudate density. According to the wound culture whose result came after 3 days, pseudomonas aeruginosa and staphylococcus aureus growth occurred. Daily dressing was planned with appropriate antibiotherapy and silver-containing wound dressing. HBO therapy was not planned until the biopsy result was determined. After 14 days, the diagnosis of baso-squamous cell carcinoma was made with the biopsy result. The patient's pulmonary computerized tomography scan revealed lung metastasis at the time of diagnosis. HBO therapy plan was canceled and the patient was referred to plastic surgery, thoracic surgery and oncology departments. The patient passed away 11 months later (Figure 5). 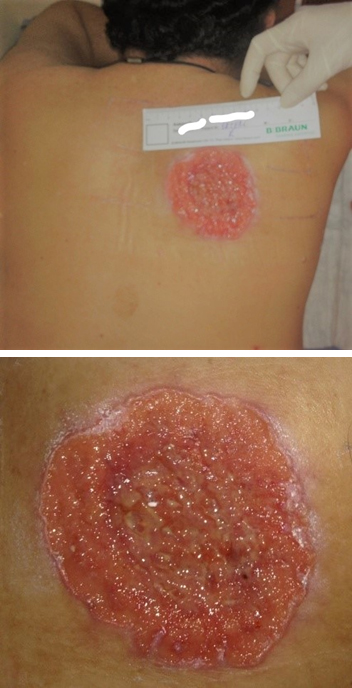 Figure 4: Basosquamous cell carcinoma.
Figure 4: Basosquamous cell carcinoma.
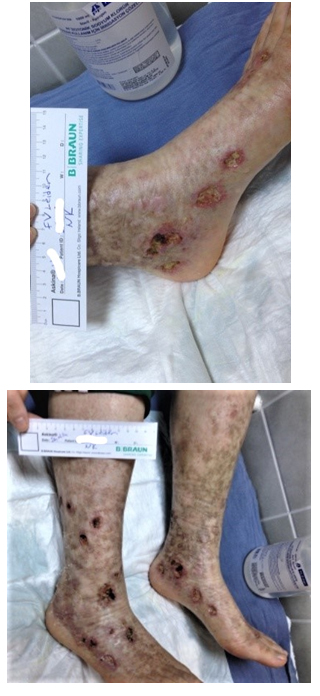 Figure 5: Factor V Leiden.
Figure 5: Factor V Leiden.
Patient 5
A 21 years old female patient was admitted to the outpatient clinic after 2.5 years of many open and closed wounds in different parts of both legs because the wounds that occurred about 1 year ago did not heal. The patient had come from abroad in hopes of getting her wounds treated. During the application, ulcers suggesting ischemic etiology, which are extremely sensitive to palpation and between 0.5 x 0.5-2x1 cm in size were observed in many parts of both legs. There were traces of previously opened and closed wounds and color changes in bilateral feet and legs. The patient stated that she had been unable to sleep at night due to pain for 3 months and that the discharge and smell of her wounds had increased recently. She was an active smoker with a history of 5 pack-years of smoking.
The patient stated that she was a university student and that she got depressed due to the smell of her wounds and was ashamed to be seen by her friends due to the appearance of her legs and that she had frozen her school registration for a year and was thinking of dropping out of school. She had started using anti-depressants with the diagnosis of a depressive reaction. She stated that she dresses her wounds regularly every day and uses many wound products and oral antibiotics to date, and as a last resort, she decided to come from abroad and apply to the hospital for HBO therapy.
Although she was a young patient, the formation of many ulcers in bilateral feet and legs raised the suspicion that there was a systemic disease in the etiology. Wound culture was taken from the patient first. Hemogram, sedimentation, CRP, rheumatoid factor, anti-nuclear antibody and peripheral blood thrombophilia panel were requested in the first place since a rheumatological and thrombophilic disease was suspected in the etiology. Proteusmirabilis grew in the wound culture. Homozygous factor V Leiden mutation was detected in the thrombophilia panel. HBO therapy was started in addition to appropriate anti-coagulant and antibiotherapy. The patient's wounds completely closed after 53 days.
Results
Among the adult cases, patients with calciphylaxis and basosquamous carcinoma passed away respectively on the ninth day and the eleventh month after admission due to the underlying diseases that caused their injuries. 1 child received the appropriate treatment after the correct diagnosis and approach. In 3 cases, surgical intervention was required during the follow-up process (debridement, amputation, wide resection).
Discussion
A chronic non-healing wound may not be just a simple deterioration of tissue integrity. The underlying disease may cause loss of limb or death of the patient. They should be suspected especially in terms of malignancy and should be evaluated in thrombophilic diseases in the etiology.
Calciphylaxis is a rare condition, but its consequences can be serious or even fatal [1]. It is most common in dialysis patients with chronic renal failure [2]. Although the mortality rate of patients diagnosed with calciphylaxis within one year is 45-80%, this rate is much higher in patients with ulcerated lesions due to sepsis [3]. Calciphylaxis clinically manifests itself with painful skin lesions. The development of infection in these lesions is typical [4]. Calcification and micro thrombosis of the dermal and subcutaneous arteries are typical [5]. There may be livedo reticularis and violet lesions at the beginning. Subsequently, black eschar-coated lesions usually occur [6].
APS is an autoimmune disease characterized by recurrent venous or arterial thrombosis [7]. The prevalence of APS is 40-50 cases per 100000 people and the incidence is 5 cases per 100000 people per year [8]. In the pathogenesis of APS, there is platelet, endothelial cell and monocyte activation that trigger thrombosis [9]. In addition to the clinical diagnosis of APS vascular thrombosis and/or pregnancy problems, lupus anti-coagulant and/or anti-cardiolipin antibodies and/or anti-beta-2 glycoprotein1 antibodies should be at a certain level in plasma. Antibodies should be detected twice within 12 weeks [10]. Although the thrombosis seen in APS is both arterial and venous, the most affected areas are the lower extremity deep veins and cerebral arteries [11]. Other clinical manifestations of APS are preeclampsia, eclampsia, pulmonary hypertension, and leg ulcers [12]. Arterial thromboses may be more prone to recurrence than venous thromboses [13].
AM is a very rare type of melanoma [14]. Acral melanoma accounts for less than 3-15% of all melanoma cases [15]. AM may be hypomelanotic or non-pigmented. In the histological examination of nonpigmented AMs, melanin pigment is found in less than 5% of tumor cells [16]. Since AMs can mimic many morphologies and occur in many different places, the rate of misdiagnosis can be up to 89% [17]. AM, especially seen in the acral regions, may be confused with diabetic foot ulcer, pyogenic granuloma, fungal infection, wart, vascular lesions, nevus or basal cell carcinoma, as in our case [18]. AM does not exhibit typical clinical features found in classical melanoma. The immunohistochemical dyes should also be used since only histological examination may be insufficient in diagnosis [17]. Since acral AMs are usually in advanced stage at the time of diagnosis, their prognosis is worse [19].
BSC is a non-melanoma aggressive skin malignancy that histopathologically includes the features of basal cell carcinoma and squamous cell carcinoma [20]. The incidence of BSC was found to be 1.2% and 1.4% respectively in various studies [21,22]. Although the clinical occurrence of BSC is not specific, it most often develops with the ulceration of a long-term nodule over time [23]. Although it is usually seen in areas with sun contact such as the head and neck (82-97%), it can rarely be seen in the body [24,25]. Biopsy and histopathological examination are the gold standard in diagnosis. For accurate diagnosis, incisional biopsy should be taken and should not be superficial. BSC has a worse prognosis because it has more metastasis and recurrence potential than BCC and SCC [23].The recurrence rate of BSC may increase up to 45% after a wide excision [26]. BSC metastasis rate is in the range of4 - 8.4% [27].
FVL results from the point mutation of the FV gene encoding the factor 5 protein in the plasma in the coagulation cascade. Factor V is a glycoprotein produced in the liver which is vitamin K-dependent [28]. Factor V Leiden Mutation, which provides resistance to Activated Protein C (APC), which inactivates factor V and VIII in the coagulation cascade, is the most common genetic thrombophilia [29]. Although Factor V Leiden Mutation increases the risk of venous thrombosis more, it also increases the risk of arterial thrombosis as it increases thrombin production [30]. Women with a history of smoking or who are active smokers have a higher risk of thrombosis than men [31]. In a study, the risk of thrombosis in FVL patients was found to be 6.6 times higher than in the normal population [32]. In a cross-sectional study conducted with 4407 people, the prevalence of FVL was found to be in the range of 1% to 8%, with the highest prevalence in the white race and the lowest prevalence in people of Asian origin [33].
Conclusion
Given the possible mortality and morbidity rate of hard-to-heal wounds, in the evaluation it is necessary to look at them from a wide perspective. If a wound does not heal, another underlying disease should be investigated. In treatment-resistant atypical cases, the clinician should take a biopsy in the slightest doubt and the diseases that cause thrombophilia in etiology should be evaluated. Early and accurate diagnosis is essential in cases of chronic wounds. These diseases can cause loss of limb or even death. A doctor evaluating chronic wounds should be informed about the diseases mentioned in this study.
Conflict of Interest
Human subjects: Consent was obtained or waived by all participants in this study. Author have declared that no financial support was received from any organization for the submitted work.
References
- Rees JK, Coles GA (1969) Calciphylaxis in man. British Medical Journal 2: 670672.
- Brandenburg VM, Cozzolino M, Ketteler M (2011) Calciphylaxis: a stillunmetchallenge. J Nephrol 24: 142-148.
- Weenig RH, Sewell LD, Davis MD, McCarthy JT, Pittelkow MR (2007) Calciphylaxis: natural history, risk factor analysis, and outcome. J Am Acad Dermatol 56: 569-579.
- Brandenburg VM, Kramann R, Specht P, Ketteler M (2012) Calciphylaxis in CKD and beyond. Nephrol Dial Transplant 27: 1314-1318.
- Mochel MC, Arakaki RY, Wang G, Kroshinsky D, Hoang MP (2013) Cutaneous calciphylaxis: a retrospective histopathologic evaluation. Am J Dermatopathol 35: 582-586.
- Dauden E, Onate MJ (2008) Calciphylaxis. Dermatologic Clinics 26: 557-568.
- Lim W (2013) Antiphospholipid syndrome. Hematology Am Soc Hematol Educ Program 2013: 675.
- Gómez-Puerta JA, Cervera R (2014) Diagnosis and classification of the antiphospholipid syndrome J Autoimmun 48-49: 20-25
- Chighizola CB, Raschi E, Borghi MO, Meroni PL (2015) Update on the pathogenesis and treatment of the antiphospholipid syndrome. Curr Opin Rheumatol 27: 476-482.
- Grimaud F, Yelnik C, Pineton de Chambrun M, Amoura Z, Arnaud L, et al. (2019) Clinical and immunological features of antiphospholipid syndrome in the elderly: a retrospective national multicentre study. Rheumatology (Oxford) 58: 1006-1010.
- Keeling D, Mackie I, Moore GW, Greer IA, Greaves M (2012) Guidelines on the investigation and management of antiphospholipid syndrome. Br J Haematol 157: 47-58.
- Ruiz-Irastorza G, Crowther M, Branch W, Khamashta MA (2010) Antiphospholipid syndrome. Lancet. 376: 1498-1509.
- Chighizola CB, Raschi E, Borghi MO, Meroni PL (2015) Update on the pathogenesis and treatment of the antiphospholipid syndrome. Curr Opin Rheumatol27: 476-482.
- Stojkovic-Filipovic J, Kittler H (2014) Dermatoscopy of amelanotic and hypomelanotic melanomaJ. Ger. Soc. Dermatol 12: 467-472.
- Soon SL, Solomon AR Jr, Papadopoulos D, Murray DR, McAlpine B, et al. (2003) Acral lentiginous melanoma mimicking benign disease: the Emory experience. J Am Acad Dermatol 48: 183-188.
- Thomas NE, Kricker A, Waxweiler WT, Dillon PM, Busman KJ, et al. (2014) Comparison of clinicopathologicfeaturesandsurvival of histopathologicallyamelanoticandpigmentedmelanomas: a population-based study. JAMA Dermatol. 150: 1306-1314.
- Gong H-Z, Zheng H-Y, Li J (2019) Amelanotic melanoma. Melanoma Res 29: 221-230.
- Gumaste P, Penn L, Cohen N, Berman R, Pavlick A, et al. (2015) Acrallentiginous melanoma of thefootmisdiagnosed as a traumaticulcer. A cautionarycase. J Am Podiatr Med Assoc 105: 189-194.
- Bradford PT, Goldstein AM, McMaster ML, Tucker MA (2009) Acral lentiginous melanoma: incidence and survival patterns in the United States, 1986-2005. Arch Dermatol 145: 427-434.
- Cappilli S, Cinotti E, Lenoir C, Tognetti L, Perez-Anker J, et al. (2022) Line-field confocal optical coherence tomography ofbasosquamous carcinoma: a caseseries with histopathological correlation. J Eur Acad Dermatol Venereol 36: 1214-1218.
- Bowman PH, Ratz JL, Knoepp TG, Barnes CJ, Finlay RE (2003) Basosquamous carcinoma. Dermatol. Surg 29: 830-832.
- Schuller DE, Berg JW, Sherman G, Krause CJ (1979) Cutaneous basosquamous carcinoma of the head and neck: a comparative analysis. Otolaryngol. Neck Surg 87: 420-427.
- Tan CZ, Rieger KE, Sarin KY (2017) Basosquamous Carcinoma: Controversy, Advances, and Future Directions. Dermatol Surg 43: 23-31.
- Garcia C, Poletti E, Crowson AN (2009) Basosquamous carcinoma. J Am Acad Dermatol 60: 137-143.
- Ciazynska M, Slawinska M, Kaminska-Winciorek G, Lange D, Lewandowski Bet al. (2020) Clinical and epidemiological analysis of basosquamous carcinoma: results of the multicenter study. Sci Rep 10: 1-8.
- Volkenstein S, Wohlschlaeger J, Liebau J, Arens A, Lehnerdt G, et al. (2010) Basosquamous carcinoma-A rare but aggressive skin malignancy. J Plast Reconstr Aesthetic Surg 63: 304-306.
- Alam M, Desai S, Nodzenski M, Dubina M, Kim N, et al. (2015) Active ascertainment of recurrence rate after treatment of primary Basal Cell Carcinoma (BCC). J Am Acad Dermatol 73: 323-325.
- Page C, Rubin LE, Gusberg RJ, Dardik A (2005) Arterial thrombosis associated with heterozygous factor V Leidendisorder, hyperhomocysteinemia, and peripheral arterial disease: importance of synergistic factors. J Vasc Surg 42:1014-1018.
- Nakashima MO, Rogers HJ (2014) Hypercoagulable states: an algorithmic approach to laboratory testing and update on monitoring of direct oral anticoagulants. Blood Res 49: 85-94.
- Mazza JJ (2004) Hypercoagulability and venous thromboembolism: a review. WMJ 103: 41-49.
- Lalouschek W, Schillinger M, Hsieh K, Endler G, Tentschert S, et al. (2005) Matched case-control study on factor V Leiden and the prothrombin G20210A mutation in patients with ischemic stroke/transient ischemic attack up to the age of 60 years. Stroke 36: 1405-1499.
- Koster T, Rosendaal FR, de Ronde H, Briet E, Vandenbroucke JP, et al. (1993) Venous thrombosis due to poor anticoagulant response to activated protein C: Leiden Thrombophilia Study. Lancet 342: 1503-1506.
- Ridker PM, Miletich JP, Hennekens CH, Buring JE (1997) Ethnic distribution of factor V Leiden in 4047 men and women. Implications for venous thromboembolism screening. JAMA 277: 1305-1307.
Citation: Gumus T (2022) Undiagnosed Hard-to-Heal Wound Cases: A Case Series. J Clin Stud Med Case Rep 9: 0141.
Copyright: © 2022 Tuna Gumus, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

