
Urinary, Fecal, and Dual Incontinence among Hispanic Women from Seven Latin-American and Caribbean Cities
*Corresponding Author(s):
Min Ji KwakDepartment Of Internal Medicine, Division Of Geriatric And Palliative Medicine, University Of Texas McGovern Medical School, 6431 Fannin St, MSB 5.126 Houston, TX 77030, United States
Tel:+1 7135006576,
Fax:+1 7135000706
Email:Min.ji.kwak@uth.tmc.edu
Abstract
Introduction: Prevalence and risk factors of Urinary Incontinence (UI), Fecal Incontinence (FI) and Dual Incontinence (DI) among Hispanic women are not often studied. The objective of this study was to evaluate the prevalence and risk factors of UI, FI, and DI among Hispanic women in seven cities using data from the Health, Well-Being, and Aging in Latin America and the Caribbean (Salud, Bienestar y Envejecimiento en America Latina y el Caribe, or SABE) study.
Methods: We conducted a cross-sectional observational study, reporting the prevalence of each incontinence (UI, FI and DI). Multivariate logistic regression analyses were used to estimate the odds of each incontinence of sociodemographic and health factors.
Results: A total of 6,550 participants were included in this analysis. Across the seven cities, an average 20.9% of participants reported urinary incontinence, 5.4% reported fecal incontinence, and 4.1% reported dual incontinence. Current and previous estrogen use was associated with a higher odds ratio of urinary incontinence. History of hysterectomy was only associated with fecal incontinence.
Conclusion: The prevalence and factors that were associated with UI, FI and DI from this study were similar to other population-based studies. However, this study has valuable implication since it only focused on Hispanic women across seven Latin American countries.
Keywords
Dual incontinence; Fecal incontinence; SABE; Urinary incontinence
SUMMARY
We identified the prevalence of urinary incontinence (20.9%), fecal incontinence (5.4%) and dual incontinence (4.1%) among Hispanic women across seven Latin American countries.
ABBREVIATIONS
UI: Urinary Incontinence
FI: Fecal Incontinence
DI: Dual Incontinence
SABE: Salud, Bienestar y Envejecimiento en America Latina y el Caribe
PAHO: Pan American Health Organization
GDS: Geriatric Depression Scale
MMSE: Mini Mental State Examination. Medical conditions include arthritis, hypertension, diabetes, heart attack, stroke and cancer
IADL: Instrumental Activities of Daily Living
INTRODUCTION
Urinary and fecal incontinence both have significant, negative impacts on the quality of life in older women [1,2]. Urinary and fecal incontinence are related to negative health outcomes including functional decline, depressive symptoms, higher risk of fall, higher rate of nursing home placement, and greater caregiver burden [3-8]. Given these outcomes, it is important to be able to identify when patients are experiencing incontinence. The prevalence of urinary incontinence ranges from 17% to 55%. The prevalence of fecal incontinence ranges from 7% to 15% [3,7]. The prevalence of both urinary and fecal incontinence, or dual incontinence, has been reported as 9.4% to 24% [9]. However, patients often fail to report their symptoms of incontinence due to embarrassment or misunderstanding them as part of the aging process. Subsequently, the prevalence of incontinence could be underreported [3,7]. Moreover, information regarding the various types of incontinence and its socioeconomic or clinical risk factors among Hispanic population is still lacking [10,11]. The objective of this study was to assess the prevalence of urinary incontinence, fecal incontinence, and dual incontinence, as well as the risk factors of developing each incontinence among Hispanic women in seven countries in Latin America (Argentina, Barbados, Cuba, Mexico, Uruguay, Chile and Brazil) using population data from the Health, Well-Being and Aging in Latin America and the Caribbean (Salud, Bienestar y Envejecimiento en America Latina y el Caribe, or SABE) study.
MATERIALS AND METHODS
Study design
We conducted a cross-sectional observational study using survey data from the SABE study.
Study population
The population of this study was comprised of 6,550 women aged 60 years old and older from the SABE study. These women were interviewed in seven cities: Buenos Aires (Argentina), Bridgetown (Barbados), Havana (Cuba), Mexico D.F. (Mexico), Montevideo (Uruguay), Santiago (Chile) and Sao Paulo (Brazil).
Data source
The database from the SABE study consisted of a round of cross-sectional surveys from cities in seven Latin American and Caribbean countries during 1999-2000 [12,13]. The Pan American Health Organization (PAHO) coordinated the overall SABE study and directed its logistics. The Center for Demography and Ecology from the University of Wisconsin-Madison, together with the PAHO, designed the study. The interviewers in each city were trained by local, country-based teams, which were constituted by a principal investigator and their associates. The response rates were 60% in Buenos Aires, 85% in Bridgetown, 85% in Sao Paulo, 84% in Santiago, 85% in Mexico City, 95% in Havana, and 66% in Montevideo. A classical multistage clustered sampling with stratification of the units at the highest levels of aggregation was used. The primary sampling unit was a cluster of independent households within predetermined geographic areas, grouped into socioeconomic strata, and divided into secondary sampling units, each containing a smaller number of households. Finally, the household and target individuals, persons 60 years old and older, were randomly selected. Then, the potential participants were contacted to schedule home interviews. The interviews were conducted in English in Bridgetown (Barbados), Portuguese in Sao Paulo (Brazil) and in Spanish in the rest of the cities, using the same validated questionnaires. Oral and written consent forms were approved by the Human Subjects Committee at each city with the corresponding affiliated medical research institution or university, and were obtained from all subjects, and personal identifiers were deleted [12,13]. A separate approval from the Institutional Review Board at University of Texas Health Science Center was not obtained since our study was a secondary analysis of publicly available database.
Dependent variables
The dependent variables were urinary incontinence, fecal incontinence, or dual (urinary and fecal) incontinence. Urinary incontinence was assessed by asking if the participant had unintentionally wet herself during the last 12 months (responses: yes or no). Fecal incontinence was assessed by asking if the participant had ever lost control over her bowel movements during the last 12 months (responses: yes or no). Dual incontinence was considered if both urinary and fecal incontinence happened during the last 12 months (responses: yes or no).
Independent variables
The independent variables of this study include sociodemographic factors, number of children, history of estrogen, history of hysterectomy, medical conditions and depressive symptoms. Sociodemographic factors included age (response: years, 60-74 vs. 75+), marital status (response: currently married, yes or no), and years of education (response: years, 0-6 vs. 7+). The number of children was assessed by asking each woman how many children she had, not including step-children, adopted children, abortions or stillbirths (response: 0 to 22). History of estrogen was assessed by asking the participant if she had previously or is presently taking estrogen for menopause (response: yes or no). The participants were also asked if they had a history of undergoing hysterectomy (response: surgery to remove the uterus, yes or no).
Medical conditions were assessed by asking the respondent if she had been ever been formally diagnosed with diabetes mellitus, arthritis, hypertension, heart disease, stroke, or cancer (response: yes or no). A summary score for medical conditions was constructed from 0 to 6, and used as a continuous variable. Depressive symptoms were measured with the Geriatric Depression Scale (GDS) [14]. The GDS contains 15 items, with a possible score of 0 to 15. Cognitive status was evaluated by the abbreviated Mini-Mental State Examination (AMMSE), which was validated in the Chilean population [12]. The AMMSE consists of 9 items (versus the 19 items of the MMSE) [15] and has a possible score of 0 to 19. Functional status was assessed by eight Instrumental Activities of Daily Living items (IADL) [16]. The participants were asked if they had difficulty performing any of these eight activities at the time of the interview: using the telephone, traveling alone, going shopping for groceries, preparing their meals, taking their medicine, handling their money, doing light house work, or doing heavy house work. To note, IADL was used as categorical variable (none vs. one or more). History of fall was assessed by asking the participant if she had ever fallen down over the last 12 months (response: yes or no).
Data analysis
Descriptive analyses were used to report the prevalence of urinary incontinence, fecal incontinence, or dual (urinary and fecal) incontinence. Multivariate logistic regression analyses were used to estimate the odds of the outcomes (urinary incontinence, fecal incontinence or dual incontinence) by sociodemographic and health factors. Variables with a p-value less than 0.20 from bivariate analysis (tested by the Chi-square or the Student’s T-test: data not shown) were finally included into the multivariate models (models 1, 2 and 3) for final analysis. History of estrogen treatment was included only in the urinary incontinence model because it was not significantly associated with fecal and dual incontinence from the bivariate analysis. P-value less than 0.05 was considered statistically significant. For all analyses, Statistical Analysis System (SAS) version 9.4 for Windows was used (SAS Institute, Cary, North Carolina and USA).
RESULTS
Prevalence of incontinence
A total of 6,550 participants were included in this analysis. Of those, 36.8% were older than 75 years old. Participants in Mexico City were relatively younger than the other cities (26.9% were older than 75 years old). An average of 30.3% of the total participants was married, ranging from 21.0% in Havana to 38.8% in Mexico City. The percentage of those who received an education over 7 years was lowest in Sao Paulo (8.0%) and highest in Havana (37.3%), while the overall average was 24.3%. The average number of children (ages 0 to 27) was 3.6±3.1. The participants in Mexico City had the most children (5.5±3.6) while Buenos Aires had the least children (2.5±2.5). Among the total participants, 17.5% had undergone a hysterectomy, ranging from 12.8% in Buenos Aires to 30.4% in Bridgetown. An average of 2.1% of the total participants was on estrogen treatment at the time of survey. This ranged from 0% in Havana and 5.3% in Santiago. However, an average 10.6% participants from the study reported a history of estrogen treatment outside of the time of the study (ranging from 4.8% in Bridgetown to 19.3% in Sao Paulo). The overall average GDS score was 3.1±3.3, with the lowest average score in Bridgetown (1.7±1.8) and highest average score in Santiago (4.1±3.6). The average MMSE score was 16.3±3.0, with lowest average score in Santiago (15.2±4.2) and the highest average score in Bridgetown (17.1±2.6). The overall average of the number of medical conditions was 1.5±1.1. Participants in Mexico City had the least number of medical conditions (1.2±1.0) while those in Havana reported the highest number (1.8±1.2). An average of 31.2% of the participants reported difficulty in performing any IADL, ranging from 19.0% in Montevideo and 44.5% in Sao Paulo (Table 1).
|
|
Buenos Aires |
Bridgeto wn |
Sao Paulo |
Santiago |
Havana |
Mexico City |
Montevid eo |
Total sample |
|
|
N=656 |
N=924 |
N=1262 |
N=855 |
N=1197 |
N=740 |
N=916 |
N=6550 |
|
Age (yr) 75+ |
31.5 |
40.5 |
44.4 |
37.3 |
38.9 |
26.9 |
30.9 |
36.8 |
|
Married |
30.0 |
23.7 |
36.5 |
29.2 |
21.0 |
38.8 |
35.2 |
30.3 |
|
Education (yr) 7+ |
23.5 |
20.4 |
8.0 |
31.5 |
37.3 |
18.6 |
32.0 |
24.3 |
|
Number of children (0-27) |
2.5 ± 2.5 |
3.5 ± 2.9 |
3.9 ± 3.4 |
4.1 ± 3.1 |
2.7 ± 2.4 |
5.5 ± 3.6 |
3.0 ± 2.6 |
3.6 ± 3.1 |
|
History of hysterectomy |
12.8 |
30.4 |
15.1 |
13.1 |
16.5 |
18.2 |
15.6 |
17.5 |
|
Currently taking estrogens |
0.3 |
1.1 |
4.6 |
5.3 |
0.0 |
2.8 |
0.4 |
2.1 |
|
Has taken before estrogens |
8.2 |
4.8 |
19.3 |
17.7 |
6.4 |
6.8 |
8.4 |
10.6 |
|
GDS score (0-15) |
3.0 ± 3.1 |
1.7 ± 1.8 |
3.4 ± 3.2 |
4.1 ± 3.6 |
3.2 ± 3.6 |
3.2 ± 3.3 |
3.3 ± 3.4 |
3.1 ± 3.3 |
|
Abbreviate MMSE score (0-19) |
16.5 ± 2.3 |
17.1 ± 2.6 |
16.0 ± 3.1 |
15.2 ± 4.2 |
16.6 ± 2.6 |
15.4 ± 2.9 |
16.8 ± 2.5 |
16.3 ± 3.0 |
|
Medical conditions (0-6) |
1.5 ± 1.0 |
1.6 ± 1.1 |
1.5 ± 1.1 |
1.6 ± 1.1 |
1.8 ± 1.2 |
1.2 ± 1.0 |
1.5 ± 1.1 |
1.5 ± 1.1 |
|
Any IADL difficulty |
30.6 |
22.4 |
44.5 |
35.7 |
30.9 |
30.8 |
19.0 |
31.2 |
|
Any falls previous 12 months |
34.4 |
28.5 |
35.4 |
39.6 |
31.1 |
39.9 |
35.3 |
34.6 |
Table 1: Study population, women aged 60 years and older, SABE study (1999-2000).
Data is presented as percentages (%) or means ± standard deviation. GDS= Geriatric Depression Scale. MMSE= Mini Mental State Examination. Medical conditions include arthritis, hypertension, diabetes, heart attack, stroke and cancer. IADL= Instrumental Activities of Daily Living.
Across the cities, an average of 20.9% of patients reported urinary incontinence, 5.4% fecal incontinence and 4.1% dual incontinence. The prevalence of urinary incontinence was highest in Santiago with 31.1% while it was lowest in Bridgetown with 10.3%. Mexico City had the highest prevalence of fecal incontinence (8.1%) while Montevideo had the lowest (2.8%). Santiago reported the highest rate of participants who reported having dual incontinence (7%), while Montevideo reported the lowest rate (2%) (Figure 1).
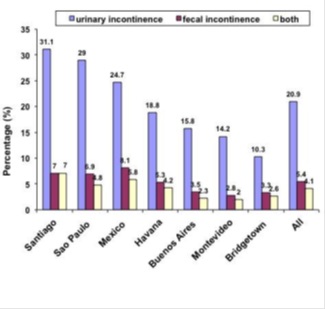 Figure 1: The percentage of urinary, fecal and dual incontinence for each city.
Figure 1: The percentage of urinary, fecal and dual incontinence for each city.
Factors that were associated with incontinence
Table 2 demonstrates multivariate analyses to predict urinary incontinence, fecal incontinence, or dual (urinary and fecal) incontinence in the combined sample of all seven cities. Significant predictors for urinary incontinence include ages 75 years and older, a higher number of children, history of taking estrogens (currently or before), a high depressive symptoms score, a lower cognitive function score, a higher number of medical conditions, having one or more IADL difficulties and a history of falls. Significant predictors for fecal incontinence include ages 75 years and older, a higher number of children, a history of hysterectomy, a high depressive symptoms score, a lower cognitive function score, a higher number of medical conditions, and having one or more IADL difficulties. Finally, significant predictors for dual incontinence include ages 75 years and older, a higher number of children, a high depressive symptoms score, a lower cognitive function score, a higher number of medical conditions, and having one or more IADL difficulties.
|
|
Urinary incontinence |
|
Fecal incontinence |
|
Dual incontinence |
|
|
Variables |
Odds ratio (95% confidence intervals) |
p-value |
Odds ratio (95% confidence intervals) |
p-value |
Odds ratio (95% confidence intervals) |
p-value |
|
Age 75+ (vs. 60-74) |
1.26 (1.09-1.47) |
0.002 |
1.33 (0.99-1.77) |
0.053 |
1.67 (1.19-2.33) |
0.003 |
|
Married (vs. no) |
0.93 (0.80-1.09) |
0.377 |
1.02 (0.75-1.38) |
0.906 |
1.11 (0.77-1.58) |
0.574 |
|
Education 7+ years (vs. 0-6) |
0.92 (0.77-1.07) |
0.325 |
1.16 (0.83-1.61) |
0.392 |
1.04 (0.69-1.55) |
0.872 |
|
Number of children (0-22) |
1.05 (1.03-1.07) |
<.001 |
1.07 (1.03-1.11) |
<.001 |
1.06 (1.02-1.11) |
0.005 |
|
History of hysterectomy (vs. no) |
0.96 (0.80-1.15) |
0.620 |
1.52 (1.10-2.10) |
0.012 |
1.42 (0.97-2.12) |
0.070 |
|
Currently taking estrogens (vs. no) |
2.25 (1.50-3.38) |
<.001 |
---* |
---* |
---* |
---* |
|
Has taken before estrogens (vs. no) |
1.42 (1.16-1.74) |
<.001 |
---* |
---* |
---* |
---* |
|
GDS score (0-15) |
1.11 (1.09-1.14) |
<.001 |
1.14 (1.10-1.17) |
<.001 |
1.14 (1.09-1.18) |
<.001 |
|
Abbreviate MMSE score (0-19) |
0.97 (0.94-0.99) |
0.005 |
0.91 (0.88-0.95) |
<.001 |
0.89 (0.85-0.93) |
<.001 |
|
Number of medical conditions (0-6) |
1.32 (1.24-1.40) |
<.001 |
1.42 (1.26-1.59) |
<.001 |
1.46 (1.28-1.68) |
<.001 |
|
Any IADL difficulty (vs. none) |
2.09 (1.80-2.42) |
<.001 |
2.02 (1.51-2.70) |
<.001 |
2.22 (1.58-3.12) |
<.001 |
|
Any falls within 12 months (vs. none) |
1.51 (1.32-1.74) |
<.001 |
1.38 (1.05-1.80) |
0.019 |
1.27 (0.93-1.74) |
0.136 |
Table 2: Multivariate logistic regression analyses for sociodemographic and health factors predicting urinary, fecal or dual incontinence in women aged 60 years and older (n=6,550), combined sample of seven cities, SABE study (1999-2000).
GDS= Geriatric Depression Scale. MMSE= Mini Mental State Examination. Medical conditions include arthritis, hypertension, diabetes, heart attack, stroke, and cancer. IADL= Instrumental Activities of Daily Living. Models 1 to 3 were adjusted for all variables into the models. (An asterisk (*) indicates that the metric was not included in multivariate regression because of non-significance from bivariate regression)
DISCUSSION
This study has assessed the prevalence and risk factors of urinary, fecal, and dual incontinence among women in seven cities in Latin America using the SABE database. Although there have been several studies assessing the epidemiology of incontinence using the SABE database, to the best of our knowledge, this is the first study using data from multiple cities from the SABE database to assess the epidemiology of all types of incontinence [7,9,17]. The overall average prevalence of urinary incontinence was 20.9%. This average is similar to previous studies [17,18]. However, the average prevalence of urinary incontinence varied from city-to-city, ranging from 10.3% in Bridgetown to 31.1% in Santiago. A wide range of prevalence of urinary incontinence is also consistent with the findings of other studies. It is thought that that the reason for such a wide range is due to underreport by participants due to embarrassment, misunderstanding the incontinence as a normal aging process, or variations in the definition of urinary incontinence [7,19].
The overall average prevalence of fecal incontinence was 5.4%, which is significantly lower than the prevalence of urinary incontinence. This average is somewhat lower than those from other studies. Tamanini et al., reported a rate of 13.2% for females in Brazil and Whitehead et al. reported a prevalaence of 8.3% among U.S. adults [17,20]. However, another study by Gouveia Santos et al. reported the prevalence of 4% among women in Brazil [21]. The range of prevalence of fecal incontinence includes 2.8% in Montevideo to 8.1% in Mexico City. Regarding dual incontinence, the average prevalence across the cities was 4.1%. The prevalence reported in the previous studies range from 1.7% to 24%, depending on the study’s design and population [9,22-25]. However, a more recent study reported a prevalence of 4.9% among community-based elderly women in Brazil, which is similar to the result of this current study [9]. The wide range of prevalence of incontinence was previously described in literature and believed to be due to inconsistent definitions of incontinence in various study settings [7].
Among the various factors that were associated with urinary, fecal, and dual incontinence, we found that age was not significantly associated with fecal incontinence, although it was significantly associated with urinary incontinence and dual incontinence. This result is somewhat similar to a previous study. Wu et al., reported that ages greater or equal to 80 years old were significantly associated with urinary incontinence and dual incontinence and not related to fecal incontinence. However, this study was comprised of U.S. men and women [25]. Use of estrogen, either prior or during the time of the study, was not significantly related to fecal or dual incontinence. However, it was highly associated with urinary incontinence. Estrogen deficiency is considered as one of the etiologies of urinary incontinence, and estrogen replacement therapy is one of the non-surgical treatment options of urinary incontinence for elderly women [26]. Given the limitation of the cross-sectional observational study, it is not possible to identify the temporality, but it is reasonable that estrogen use has significant association with urinary incontinence only.
Having more children was significantly related to all kinds of incontinence. This is a reasonable result considering pelvic muscle changes and potential pelvic organ damage during vaginal delivery. A history of hysterectomy was not associated with urinary incontinence, but was associated with fecal incontinence and it is also probably due to the direct damage to the pelvic floor during the surgery. This pattern was also observed in previous U.S. population based study by Wu et al., [25,27].
This current study holds several limitations. First, this study is an observational study using a survey method. Thus, statistical significance of the odds ratio does not necessarily mean causality. For example, estrogen use does not mean that estrogen causes urinary incontinence, but it more likely means that the subject was on estrogen treatment for underlying urinary incontinence. However, variables such as multiparity, hysterectomy and multicomorbidity could be considered as preceding risk factors of urinary incontinence. Second, the current study used relatively old data, from 1999 to 2000. However, no more recent data from the all seven Latin cities is available at this time, although more recent data from Sao Paulo is available. We conducted this project using the most available and most extensive dataset, so that the result can be generalized to other Hispanic population. Considering the significant knowledge gap in incontinence research in Hispanic population, we believe that the result of the study will be additional value in population health in this racial group, although it used old dataset.
CONCLUSION
This study assessed the prevalence of urinary, fecal, and dual incontinence among women from seven cities in Latin America (Argentina, Barbados, Cuba, Mexico, Uruguay, Chile and Brazil) using population data from Health, Well-Being and Aging in Latin America and the Caribbean Study. Across the cities, an average 20.9% participants reported urinary incontinence, 5.4% reported fecal incontinence and 4.1% reported dual incontinence. Current and previous use of estrogen was associated with higher odds ratio of urinary incontinence. History of hysterectomy was only associated with fecal incontinence. No specific socioeconomic factors (education or marital status) were associated with any kind of incontinence. Despite the limitations of an observational study, this study has implications that it used a wide range of population database across the Lain American countries and assessed various covariates to identify risk factors of all kinds of incontinence focusing on Hispanic women.
AUTHORS’ CONTRIBUTION
M Kwak and R Felix - manuscript writing/editing and interpreting the results. D Carbonell and CA Reyes-Ortiz - project development, data analysis, manuscript editing.
REFERENCES
- Goode PS, Burgio KL, Richter HE, Markland AD (2010) Incontinence in older women. JAMA 303: 2172-2181.
- Ko Y, Lin S-J, Salmon JW, Bron MS (2005) The impact of urinary incontinence on quality of life of the elderly. Am J Manag Care 11: 103-111.
- Bharucha AE, Dunivan G, Goode PS, Lukacz ES, Markland AD, et al. (2015) Epidemiology, pathophysiology, and classification of fecal incontinence: State of the science summary for the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) workshop. Am J Gastroenterol 110: 127-136.
- Brown JS, Vittinghoff E, Wyman JF, Stone KL, Nevitt MC, et al. (2000) Urinary incontinence: does it increase risk for falls and fractures? Study of Osteoporotic Fractures Research Group. J Am Geriatr Soc 48: 721-725.
- Chiarelli PE, Mackenzie LA, Osmotherly PG (2009) Urinary incontinence is associated with an increase in falls: A systematic review. Aust J Physiother 55: 89-95.
- Holroyd-Leduc JM, Mehta KM, Covinsky KE (2004) Urinary incontinence and its association with death, nursing home admission, and functional decline. J Am Geriatr Soc 52: 712-718.
- Tamanini JTN, Pallone LV, Sartori MGF, Girão MJBC, dos Santos JLF, et al. (2018) A populational-based survey on the prevalence, incidence, and risk factors of urinary incontinence in older adults-results from the "SABE STUDY". Neurourol Urodyn 37: 466-477.
- Thom DH, Haan MN, Van Den Eeden SK (1997) Medically recognized urinary incontinence and risks of hospitalization, nursing home admission and mortality. Age Ageing 26: 367-374.
- Yuaso DR, Santos JLF, Castro RA, Duarte YA, Girão MJBC, et al. (2018) Female double incontinence: Prevalence, incidence, and risk factors from the SABE (Health, Wellbeing and Aging) study. Int Urogynecol J 29: 265-272.
- Escobar DA, Botero AM, Cash MG, Reyes-Ortiz CA (2016) Factors associated with hysterectomy among older women from Latin America and the Caribbean. Women Health 56: 522-539.
- Mallett VT, Jezari AM, Carrillo T, Sanchez S, Mulla ZD (2018) Barriers to seeking care for urinary incontinence in Mexican American women. Int Urogynecol J 29: 235-241.
- Albala C, Lebrão ML, León Díaz EML, Ham-Chande RH, Hennis AJ, et al. (2005) Encuesta Salud, Bienestar y Envejecimiento (SABE): Metodología de la encuesta y perfil de la población Revista Panamericana de Salud Pública 17: 307-322.
- Wong R, Peláez M, Palloni A, Markides K (2006) Survey data for the study of aging in Latin America and the Caribbean: Selected studies. J Aging Health 18: 157-179.
- Sheikh JI, Yesavage JA (1986) Geriatric Depression Scale: recent evidence and development of a shorter version. Clinical Gerontologist 5: 165-173.
- Folstein M, Folstein SE, McHugh PR (1975) "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12: 189-198.
- Fillenbaum GG (1985) Screening the elderly. A brief instrumental activities of daily living measure. J Am Geriatr Soc 33: 698-706.
- Tamanini JTN, de Jesus FA, Castro RA, Sartori MGF, Girão MJBC, et al. (2016) The prevalence of fecal incontinence and associated risk factors in older adults participating in the SABE study. Neurourol Urodyn 35: 959-964.
- Thomas TM, Plymat KR, Blannin J, Meade TW (1980) Prevalence of urinary incontinence. Br Med J 281: 1243-1245.
- Stewart WF, Hirsh AG, Kirchner HL, Clarke DN, Litchtenfeld MJ, et al. (2014) Urinary incontinence incidence: Quantitative meta-analysis of factors that explain variation. J Urol 191: 996-1002.
- Whitehead WE, Borrud L, Goode PS, Meikle S, Mueller ER, et al. (2009) Fecal incontinence in US adults: Epidemiology and risk factors. Gastroenterology 137: 512-517.
- de Gouveia Santos VLC, de Cássia Domansky R, Hanate C, Matos DS, Benvenuto CVC, et al. (2014) Self-reported fecal incontinence in a community-dwelling, urban population in southern Brazil. J Wound Ostomy Continence Nurs 41: 77-83.
- Matthews CA, Whitehead WE, Townsend MK, Grodstein F (2013) Risk factors for urinary, fecal, or dual incontinence in the Nurses' Health Study. Obstet Gynecol 122: 539-545.
- Roberts RO, Jacobsen SJ, Reilly WT, Pemberton JH, Lieber MM, et al. (1999) Prevalence of combined fecal and urinary incontinence: A community-based study. J Am Geriatr Soc 47: 837-841.
- Stenzelius K, Mattiasson A, Hallberg IR, Westergren A (2004) Symptoms of urinary and faecal incontinence among men and women 75+ in relations to health complaints and quality of life. Neurourol Urodyn 23: 211-222.
- Wu JM, Matthews CA, Vaughan CP, Markland AD (2015) Urinary, fecal, and dual incontinence in older U.S. Adults. J Am Geriatr Soc 63: 947-953.
- Cody JD, Jacobs ML, Richardson K, Moehrer B, Hextall A (2012) Oestrogen therapy for urinary incontinence in post-menopausal women. Cochrane Database Syst Rev 10: CD001405.
- Pucciani F (2018) Post-surgical fecal incontinence. Updates Surg 70: 477-484.
Citation: Kwak MJ, Felix R, Carbonell D, Reyes-Ortiz CA (2020) Urinary, Fecal, and Dual Incontinence among Hispanic Women from Seven Latin-American and Caribbean Cities. J Gerontol Geriatr Med 6: 067.
Copyright: © 2020 Min Ji Kwak, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

