
Use of Prednisolone, CBD and Behavior Modification as a Treatment for Atopic Dermatitis in a Canine: A Case Report
*Corresponding Author(s):
Chie MogiDepartment Of Animal Health Technology, Yamazaki University Of Animal Health Technology, Tokyo, Japan
Tel:+81 426530901,
Fax:+81 426530902
Email:c_mogi@yamazaki.ac.jp
Abstract
Introduction: Canine Atopic Dermatitis (CAD) is a chronic, pruritic skin disease. Although Cannabidiol (CBD) has neuroprotective, analgesic, anxiolytic, and anti-inflammatory effects, few studies have examined its use in dogs with CAD. This study aimed to evaluate the efficacy of CBD-containing hemp oil in combination with behavior modification therapy in the treatment of CAD.
Case presentation: A 48-month-old castrated male Maltese dog with a history of Canine Atopic Dermatitis (CAD) and adverse food reaction presented with genital licking behaviors that began approximately two years prior to presentation. The patient had received dermatological treatment two years prior to presentation, but the licking behavior continued. During the visit, the patient was diagnosed with stereotypical genital licking. The behavior was temporarily interrupted when the dog’s owner intervened verbally but would continue shortly thereafter. A diagnosis of obsessive compulsive disorder was made and behavior modification therapy was initiated. An elimination diet was prescribed and topical steroids were administered. These treatments alleviated the pruritis in the extremities but did not alter the frequency of genital licking. Therefore, Cannabidiol (CBD) was administered for 21 days after the initiation of the behavior modification therapy. Twenty-seven days later, the genital licking behavior decreased and could be stopped via verbal intervention from the dog’s owner.
Conclusion: In this patient, the stereotypical behavior was treated with CBD. Factors that contribute to stereotypic behavior are frustration and conflict. It is likely that the behavior began due to lack of care and unsatisfied motor drive. To date, potential efficacy has been reported in human dermatology; however, there have been no reports of CBD being used to treat CAD in dogs. These results highlight the importance of careful medical evaluations and treatment of a primary illness even when behavioral issues are prominent, as well as the potential use of CBD to treat stereotypical behaviors.
Keywords
Atopic dermatitis; Behavior therapy; Cannabidiol; Canine; Steroids
Introduction
Canine Atopic Dermatitis (CAD) is a chronic, pruritic skin disease that is seen with high frequency in veterinary clinics [1]. In atopic dermatitis, there is an excessive immune response in the skin, abnormalities in epidermal barrier function and scratching behavior [2]. Generalized pruritis is present in more than 40% of cases. Behaviors such as scratching, rubbing, and excessive grooming are seen due to the intense pruritis [3]. Acral lick dermatitis is a common skin disease in dogs caused by stereotypical licking of localized areas of the skin, such as the lower legs and armpits, and is believed to be caused by inadequate housing conditions and lack of social interaction and care. This behavior can be treated with serotonin modulators, suggesting an association with serotonin dysregulation [4].
Cannabidiol (CBD) is a non-psychoactive component of cannabis that has many beneficial effects on the body. CBD does not have a direct effect on the CB1 and CB2 receptors of the endogenous cannabinoid system, but has been reported to have neuroprotective, analgesic, anxiolytic, and anti-inflammatory effects. CBD and other hemp-derived natural constituents are expected to improve atopic dermatitis due to their involvement in the regulation of the endogenous cannabinoid system [5].
However, few studies have been conducted on the use of CBD in dogs with CAD [6]. The purpose of this study was to evaluate the efficacy of CBD-containing hemp oil in combination with behavior modification therapy in the treatment of CAD.
Case Presentation
A 48-month-old castrated male Maltese (2.5 kg) dog with a history of atopic dermatitis presented with stereotypical genital licking. The patient was obtained from a pet shop at the age of 2 months. From that time, frequent vomiting and diarrhea occurred and were effectively treated using an antidiarrheal drug. The patient was also noted to frequently have a decreased appetite. While the patient was walked outdoors for approximately 20 minutes per day, he did not urinate or defecate as he was focused on smelling the surroundings and scavenging for food. He swallowed anything he could put in his mouth. The patient played with toys with his owner twice a day and did not bark to make demands. The patient was kept within an enclosed area of the home with a place to urinate and defecate and an area to sleep when his owners were not home and overnight. Throughout the day, he independently went to his bed to lick his genitals or sleep.
At the age of 24 months, the patient’s hair began to change color as a result of licking his hind legs. He was treated with steroids, though the licking behavior would restart once the medication was discontinued. At 44 months of age, allergen identification and a lymphocyte reaction test were performed. The patient was identified as reactive to beef, pork, chicken, eggs, sheep, horse, turkey, duck, and salmon. He was diagnosed with Canine Atopic Dermatitis (CAD) and Adverse Food Reaction (AFR). A wheat-based diet resulted in normalized stools and appetite.
The patient also had a history of growling and was diagnosed with a learned behavior of defensive aggression for self-protection. Growling was observed during the consultation when the veterinarian attempted to palpate the patient and was reported to occur when the owners attempted to remove items from the patient’s mouth, stop the patient from licking his genitals, or take away toys or snacks. The patient was also diagnosed with pica based on reports of his behaviors during outdoor walks. The owner stated that the patient would put garbage and stones into his mouth that the owner was unable to remove.
The patient was treated with prednisolone (1.25 mg every 3 days), oclacitinib (0.9 mg/ day on days he did not take prednisolone), paracasei (lactic acid bacterium Lactobacillus paracasei: approximately 20 billion (live bacteria)/capsule, one capsule per day), and kestose (400 mg/day). On treatment day 35, CBD treatments were initiated. The patient was administered Sweet Potato Soft Chewables (3 mg CBD) (Treatibles; AD Remedies, Inc., TN, USA) three times daily. On treatment day 91, the CBD chewables were decreased to twice daily. On treatment day 94, the oclacitinib was discontinued. On treatment day 150, the prednisolone was adjusted to 1.25 mg every four days.
The patient was maintained on a wheat-based food (pure protein wheat), allergen-restricted diet with gluten-free quinoa biscuits as needed. Erythritol mist, an epithelial moisturizing bacteriostatic mist, was sprayed on the locations that the patient licked. On treatment day 53, the patient’s diet was changed from pure protein wheat to cod (Figures 1 & 2).
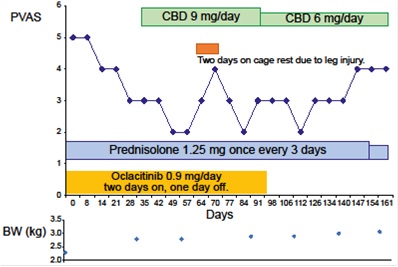 Figure 1: Schematic diagram of the treatment process. Changes in PVAS and the drug and CBD doses during treatment and at follow-up.BW, body weight; CBD, Cannabidiol; PVAS, Pruritus Visual Analog Score.
Figure 1: Schematic diagram of the treatment process. Changes in PVAS and the drug and CBD doses during treatment and at follow-up.BW, body weight; CBD, Cannabidiol; PVAS, Pruritus Visual Analog Score.
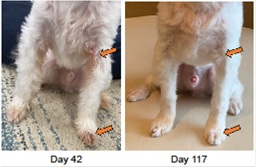 Figure 2: The axilla and forelimb after treatment. Discoloration of the coat has faded. The arrows show the lesion sites before and after treatment. The number of days corresponds to the time that has elapsed since the behavioral treatment was initiated.
Figure 2: The axilla and forelimb after treatment. Discoloration of the coat has faded. The arrows show the lesion sites before and after treatment. The number of days corresponds to the time that has elapsed since the behavioral treatment was initiated.
Behavior modification methods
The patient’s strict diet was increased as needed when the patient’s desire to eat increased. The owner was instructed to make the patient walk faster so that he could not put foreign objects in his mouth while walking. When the dog tried to sniff the ground during the walk, she gave him a cue to "sit" and rewarded him if he sat down without sniffing. The owner was also instructed to hold the patient during outdoor walks, as needed. Due to the increased walking speed, the patient was allowed additional sleep time throughout the day.
To inhibit genital licking behavior, the patient was trained to obey the commands "sit," "down," and "wait" using positive reinforcement methods by rewarding with highly palatable, hypoallergenic treats. Treats were also used for counter conditioning to the licking behavior. In other words, the owner cued him to "come" when he tried to lick and rewarded him if he approached the owner without licking. During the follow-up period after behavioral modification began, aggressive growling and biting behaviors were no longer observed when the owner reached out while the patient was licking.
Result
Case description through treatment stages.The patient's progress was obtained via an online interview with his owner. One week after starting the behavioral treatment, the patient did not stop licking when the owner verbally commanded him to come. On day 35 CBD (9mg/day) was administered twice a day to shorten the licking time. The patient no longer licked his genitals four weeks after he started receiving CBD. When the patient suffered an injury to his leg, the licking behavior increased during his two-day cage rest period. After two weeks the patient’s licking behavior decreased. He could sleep without licking. The dose of CBD was decreased to 6 mg/day. The patient continued licking his genitals before sleeping overnight. The behavior stopped when the patient was commanded to come to his owner for a treat (Table 1).
|
Treatment stage |
I |
II |
III |
IV |
|
Behavioral modification |
When the patient starts to lick genital area, the owner verbally commands to come to the owner. |
|||
|
CBD |
not used |
9mg/day |
9mg/day |
6mg/day |
|
Patient behavior |
He stopped as soon as the command was given, but quickly resumed licking again. |
The patient no longer licked his genitals. |
The patient suffered an injury to his leg. The licking behavior increased during his two-day rest period. |
The patient continued licking his genitals before sleeping. |
Table 1: Treatment stage.
Discussion
Stereotypical behavior (obsessive-compulsive disorder) in dogs can exhibit as a variety of behavioral patterns. Most often, dogs experience frustration and conflict when placed in a particular situation and adapt their behavior accordingly. Over time, this behavior begins to occur outside of these specific situations regardless of external stimuli. These behaviors often include an intervention by the owner, which may result in behavioral conditioning [7]. This patient’s licking behavior started at the age of one year, when his allergies were not managed; the behavior likely began secondary to pruritis. Although the pruritic sensation decreased after steroid treatment, the behavior washabitualized and difficult to control. As the licking behavior occurred after meals and the patient could not stop licking even when commanded to do so, an unmet desire for food was likely a factor.
The stereotypical behavior of licking is often associated with dermatological conditions. Licking behaviors occur due to skin pain and pruritus. Licking worsens the condition of the skin, further increasing the pain and pruritus, leading to a vicious cycle that increases the licking behavior [8]. In this patient, pruritis due to dietary allergic diseases is believed to be the main cause of the licking behavior. Therefore, the licking behavior became more frequent as the skin problems worsened. When dermatological treatments alleviated the pruritis, the licking behavior persisted due to habitualization.
Genital self-harm as an abnormal clinical symptom of separation anxiety has been reported in dogs [9]. Separation anxiety symptoms include barking, trembling, housesoiling and stereotypical licking behaviors when a dog is separated from its owner or other persons to whom they are attached [10]. As this patient rarely engaged in licking behavior when his owner was not present and there were no other signs of separation anxiety (such as excessive barking or tremors at the onset of separation), separation anxiety was excluded. Frustration due to a lack of exercise can also lead to excessive aggression, increased self-grooming and vocalization, repetitive motor behaviors and pica [11]. This patient's desire for exercise was likely not satisfied as he could not stop eating foreign objects during the walks, causing the owner to be hesitant to take him out for walks. The licking behavior decreased when the patient was encouraged to walk faster.
Cannabidiol (CBD) is a non-psychoactive ingredient found in cannabis plants that has been shown to have many beneficial effects on the body while having no direct action on the CB1 and CB2 receptors of the endocannabinoid system. CBD has been reported to have neuroprotective, antioxidant, and anti-inflammatory effects [5]. As cannabis-derived natural ingredients such as CBD are involved in the regulation of the endocannabinoid system, they are expected to improve various skin symptoms. Cannabinoid receptors (CB1 and CB2) have been shown to be more highly expressed in the skin of CAD-affected dogs than in healthy dogs [12]. CBD is effective against the reduced skin barrier function, increased inflammation [13] and pruritis-induced anxiety that occurs during itching behaviors [14]. Therefore, the use of CBD reduced this patient's perception of pruritis, conflict, and anxiety. As CBD is effective for several conditions, it is a safe treatment even when an accurate diagnosis is difficult. However, there are few studies regarding the use of CBD for canine skin diseases in veterinary practice [15] and there are no reports of the combined use of CBD and steroids. In this case study, the combination therapy was reduced as the patient’s quality of life and symptoms improved, suggesting that CBD is a safe and effective supplement in canines.
Acknowledgment
All preparations for the importation and use of CBD products were made by the kind courtesy of Ken Takakura, President of Takakura New Industries Inc. We would like to thank Editage (www.editage.com) for English language editing.
Data Deposition Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authorship Confirmation Statement
Chie Mogi made substantive contributions to the design conception and implementation of the work. Koji Kawano and Norihito Mizuno acquired and interpreted the data for the work; Takaaki Fukuyama contributed to the design concept of the work and facilitated the implementation of the research.
Funding
The present study was funded by the Research scholarship from Takakura New Industries Inc. and a research grant from the Yamazaki University of Animal Health and Technology.
Competing Interest Declaration
The primary and last author receives compensation from Takakura New Industries Inc. The other authors have no conflicts of interest to disclose.
References
- Saridomichelakis MN, Olivry T (2016) An update on the treatment of canine atopic dermatitis. Vet J 207: 29-37.
- Kabashima K (2013) New concept of the pathogenesis of atopic dermatitis: interplay among the barrier, allergy, and pruritus as a trinity. J Dermatol Sci 70: 3-11.
- Olivry T, Boer DJ, Favrot C, Jackson HA, Mueller RS, et al. (2015) International Committee on Allergic Diseases of Animals. Treatment of canine atopic dermatitis: 2015 updated guidelines from the International Committee on Allergic Diseases of Animals (ICADA). BMC Vet Res 11: 210.
- Walsh BR (2020) A critical review of the evidence for the equivalence of canine and human compulsions. Appl AnimBehav Sci 234: 105166.
- Atalay S, Karpowicz IJ, Skrzydlewska E (2020) Antioxidative and anti-inflammatory properties of cannabidiol. Antioxidants 9: 21.
- Mogi C, Yoshida M, Kawano K, Fukuyama T (2021) Effects of cannabidiol without delta-9-tetrahydrocannabinol on canine atopic dermatitis: a retrospective assessment of 8 cases. Can Vet J.
- Tynes VV, Sinn L (2014) Abnormal repetitive behaviors in dogs and cats: a guide for practitioners. Vet Clin Small Anim Pract 44: 543-564.
- Luescher AU (2003) Diagnosis and management of compulsive disorders in dogs and cats. Vet Clin Small AnimPract 33: 253-267.
- Ghaffari MS, Khorami N, Marjani M, Aldavood SJ (2007) Penile self?mutilation as an unusual sign of a separation?related problem in a crossbreed dog. J Small AnimPract 48: 651-653.
- Harvey ND, Craigon PJ, Shaw SC, Blott SC, England GCW (2019) Behavioural differences in dogs with atopic dermatitis suggest stress could be a significant problem associated with chronic pruritus. Animals 9: 813.
- Schipper LL, Vinke CM, Schilder MBH, Spruijt BM (2008) The effect of feeding enrichment toys on the behaviour of kennelled dogs (Canis familiaris). Appl AnimBehav Sci 114: 182-195.
- Campora L, Miragliotta V, Ricci E, Cristino L, Di Marzo V, et al. (2012) Cannabinoid receptor type 1 and 2 expression in the skin of healthy dogs and dogs with atopic dermatitis. Am J Vet Res 73: 988-995.
- Baswan SM, Klosner AE, Glynn K, Rajgopal A, Malik K, et al. (2020) Therapeutic potential of cannabidiol (CBD) for skin health and disorders. Clin CosmetInvestig Dermatol 13: 927.
- Crippa JA, Guimarães FS, Campos AC, Zuardi AW (2018) Translational investigation of the therapeutic potential of cannabidiol (CBD): Toward a new age. Front Immunol 9: 2009.
- Cindy HJ, Rupasinghe HPV (2021) Cannabidiol-based natural health products for companion animals: Recent advances in the management of anxiety, pain, and inflammation. Res Vet Sci 140: 38-36.
Citation: Mogi C, Kawano K, Mizuno N, Fukuyama T (2021) Use of Prednisolone, CBD and Behavior Modification as a Treatment for Atopic Dermatitis in a Canine: A Case Report. J Altern Complement Integr Med 7: 207.
Copyright: © 2021 Chie Mogi, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

